

Special Article - Year 2022 - Volume 37 -
Harvest of fascia lata for use in a temporal orthodromic flap in the treatment of facial paralysis
Coleta de fáscia lata para uso em retalho ortodrômico temporal no tratamento da paralisia facial
ABSTRACT
Introduction: Facial palsy requires multidisciplinary treatment and surgical options are individualized for each patient and according to the experience of the medical team. The Orthodromic Temporalis Muscle Flap (OTF) is a well-documented form of correction in the literature, with satisfactory results. One of the steps of its accomplishment is the harvest of the fascia lata to bridge between the temporal tendon and the lips. The objective is to propose a standardization of the required amount of fascia lata and simplified harvest technique.
Methods: Surgical description of the fascia measurement required for the procedure and its harvest.
Results: Replicable and safe procedure according to the experience of the senior author.
Conclusion: The proposed harvest tactic can facilitate this procedure and make it safer for patients in diferent health services.
Keywords: Fascia lata; Facial asymmetry; Facial paralysis; Reconstructive surgical procedures.
RESUMO
Introdução: A paralisia facial necessita de um tratamento multidisciplinar e as opções cirúrgicas são individualizadas para cada paciente e conforme a experiência da equipe médica. O Retalho Ortodrômico Temporal (ROT) é uma forma de correção bem documentada na literatura, com resultados satisfatórios. Um dos passos de sua realização é a coleta da fáscia lata para ponte entre o tendão temporal e os lábios. O objetivo é propor uma padronização da quantidade necessária de fáscia lata e técnica de coleta simplificada.
Métodos: Descrição cirúrgica da medida de fáscia necessária para o procedimento e sua coleta.
Resultados: Procedimento replicável e seguro conforme experiência do autor sênior.
Conclusão: A tática de coleta proposta pode facilitar a realização deste procedimento e torná-lo mais seguro para os pacientes em diferentes serviços de saúde.
Palavras-chave: Fascia lata; Assimetria facial; Paralisia facial; Procedimentos cirúrgicos reconstrutivos.
INTRODUCTION
The facial nerve is the seventh cranial nerve and emerges from the brainstem, passing through the temporal bone until it exits through the stylomastoid foramen, from which it supplies multiple branches to innervate the muscles of facial expression1.
Among the various nerves, it is one of the most prone to some injury, which primarily impairs facial expression. When this occurs, temporarily or permanently, we can call this change facial paralysis, which can be central or peripheral2.
Despite having been studied for a long time and having a negative impact on a patient’s quality of life, the complexity involved in its pathophysiology and the varied clinical repercussions makes its treatment challenging and necessarily individualized.
Current treatments are commonly multidisciplinary, involving prolonged follow-ups with many specialists. They range from less invasive procedures, such as botulinum toxin, to major surgeries that rely on complex flaps, usually microsurgical, sometimes combining regional muscle transfers and cross-face nerve grafts3.
When the nerve injury has a period longer than 24 months, it is known that any attempt to neurotize the muscles, regardless of the method chosen, has a low chance of success due to muscle atrophy3. For these cases, measures such as the temporal orthodromic flap (TOF) are especially useful, as they can provide a satisfactory result, especially for excursion of the commissure, in a single step and without microsurgery, as well as without compromising the facial nerve in cases where it is still recovering4.
To perform the TOF, there must be tissue with good resistance and preferably autologous so that the tendon transfer is sustainable, durable and safe for the patient. At this time, the fascia lata appears as an excellent donor area.
The fascia lata is a complex layer of fibrous tissue that involves all the deep tissues of the thigh, with variations in thickness, being thicker in its lateral and proximal portion, with its connective fibers predominantly in the longitudinal direction5.
Its collection is possible in several ways and with multiple clinical and surgical objectives, involving periocular and frontal approaches, even vulvovaginal, in adult and pediatric patients6-8.
We present, below, a proposal to standardize its collection for the TOF.
OBJECTIVE
The present article aims to propose a standard estimate of the amount in centimeters of fascia lata that needs to be resected to make a temporal orthodromic flap in the treatment of facial paralysis, as well as to suggest a way of collecting the fascia lata in the anterolateral region of the thigh.
METHODS
The proposed standardization is based on the long experience of the senior author of this article, both in his private clinic and as a professor of the Plastic Surgery discipline at Hospital das Clínicas de Botucatu, Botucatu-SP, from 2005 to 2021.
Estimation of the size of the fascia to be collected
On the side affected by the paralysis, the distance between the middle third of the lower edge of the zygomatic arch to the ipsilateral buccal rim is measured, adding up to 4 cm.
Fascia lata collection
With the patient in the horizontal supine position and with the left thigh (when not dominant) in an anatomical position, draw a line parallel to the anterosuperior iliac crest and another line parallel to the superior border of the patella. A midline is drawn between the two previously drawn, where the groove between the anterior and posterior compartment of the thigh should be palpated. In it, 2 cm above this groove is the central point that will guide a longitudinal incision in the thigh of 5 to 6 cm (Figure 1).
This point will be in the center of a rectangle with a height measuring the size of the desired fascia and a width ranging from 2.5 to 3 cm.
The entire area should be infiltrated, preferably with a solution containing 0.9% saline solution, adrenaline in a dilution of 1:200,000 to 1:250,000 and local anesthetic.
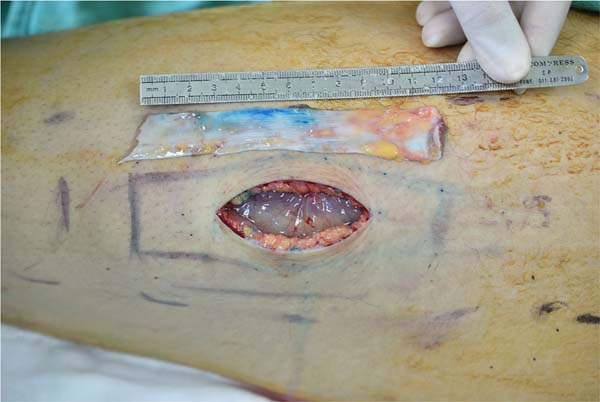
After the skin incision, the subcutaneous tissue is detached with Metzenbaum scissors until the fascia lata is identified (Figure 2).
The entire area of the drawn rectangle is detached, extending 1 cm in all directions to facilitate its closure. Peeling is facilitated with the use of Viterbo peelers, as well as with the aid of lighted retractors.
It is recommended that the rectangle drawn on the skin is now demarcated directly on the fascia lata with bright green or methylene blue.
The rectangle must be incised with a scalpel, taking care not to injure the underlying muscle. The entire fascia can be removed with a scalpel or, after the initial incision of the vertical lines, it can be removed with long Metzenbaum scissors.
Attention must be paid to superior and inferior resections to avoid beveling and irregularities in the shape of the fascia and inadvertent injury to the muscle.
After removing the fascia (Figure 3), a careful hemostatic review is initiated, and the remaining fascia is then closed, preferably with non-absorbable suture such as 3-0 mononylon suture with “U” or “X” stitches, leaving the nodes inverted.
After that, we recommend that the space created between the fascia and the subcutaneous tissue be reduced with adhesion sutures with long-lasting absorbable thread - in our experience, we recommend a continuous suture in the superior space and another in the inferior, with two monocryl threads 3- 0, which alternately transfix the fascia lata and the subcutaneous tissue, until they meet in the center of the incision. Finally, a subdermal suture is performed, followed by skin synthesis with an intradermal suture with a 4-0 monocryl thread (Figure 4).
General Care
The fascia lata is kept immersed in saline until the moment of its use in the TOF.
The dressing must be compressive in the first 48 to 72 hours, paying attention to any bruising and the risk of fascia disruption and muscle herniation.
The patient is already allowed to walk from the first day.
RESULTS
This procedure is safe in the senior author’s experience, and the clinical benefits outweigh the inherent risks.
DISCUSSION
When there is a need for surgical treatment for facial paralysis, when some form of neurotization of the mimic muscles is not possible, two possibilities stand out: free muscle flap or some form of tendon transfer, such as TOF9,10.
When comparing them, a similar effect on the smile is observed between the two interventions, with a slight superiority of the TOF as it does not cause the impression of an asymmetrical volume of the face, despite not having the ability to generate the same dynamic result of free muscle transfer. It is worth mentioning that the latter requires a more complex surgery, without necessarily an immediate result10,11. In addition, the TOF allows intraoral shortening of the fascia lata in a second surgical time if a gain in greater symmetry is required.
In TOF, as used in our group3,11, the objective is not to excessively manipulate the muscles or remove bone tissue as in the past but to preserve the muscle direction - hence the term orthodromic -connecting the temporal muscle tendon, which is functioning in the indicated patients, to the lip, using the fascia lata as a bridge11.
Therefore, the fascia lata is critical to this procedure.
Some authors reported minimally invasive forms of fascia lata removal, either with rigid endoscopes or by adopting graft expansion measures, such as the technique proposed by Evereklioglu8. In it, the fascia is cut into a strip in the shape of a “Z,” which the author called “kite tail,” to gain extension in length.
In the 39 patients reported by Pidgeon et al.4, the fascia lata was collected using a 10cm incision, removing a 12x2.5cm strip from the ipsilateral thigh next to the paralyzed face.
Giovannetti et al.12 preferred removing grafts from the right thigh with slight flexion and medial rotation. They usually make a linear incision of 4 to 8 cm, demarcated from 4 to 5 cm above the knee. This incision is performed to collect a fascia measuring about 3x6cm, cut with scissors. Closure of the remaining fascia is performed with 3-0 Vycril thread or as proposed by Vitali et al.13. These authors suggested covering the donor area with a collagen sheet derived from the bovine pericardium.
It is important to point out that patients with facial paralysis tend to have a greater aesthetic demand as they undergo more surgical procedures. Often, it is necessary to adapt the height of the incision to avoid low scars that can be exposed in some garments, such as skirts.
Comparing our collection technique with the literature, we must remember that many works need a smaller amount of fascia, as they work with shorter distances, as in frontal elevation. However, the central idea remains and can be applied in these situations since the incision suggestion can be reduced proportionally to the amount of required fascia.
CONCLUSION
The sequence of estimating the size of the fascia lata needed to perform the temporal orthodromic flap and collecting it according to the suggested steps can facilitate the performance of this intervention and make the procedure safe and of great clinical benefit to patients who need autologous tissue for surgical corrections
REFERENCES
1. Kochhar A, Larian B, Azizzadeh B. Facial Nerve and Parotid Gland Anatomy. Otolaryngol Clin North Am. 2016;49(2):273-84. DOI: 10.1016/j.otc.2015.10.002
2. Batista KT. Paralisia facial: análise epidemiológica em hospital de reabilitação. Rev Bras Cir Plást. 2011;26(4):591-5.
3. Viterbo F, Romão A, Brock RS, Joethy J. Facial reanimation utilizing combined orthodromic temporalis muscle flap and end-to-side cross-face nerve grafts. Aesthetic Plast Surg. 2014;38(4):788-95. DOI: 10.1007/s00266-014-0357-8
4. Pidgeon TE, Boca R, Fatah F. A technique for facial reanimation: The partial temporalis muscle-tendon transfer with a fascia lata sling. J Plast Reconstr Aesthet Surg. 2017;70(3):313-21. DOI: 10.1016/j.bjps.2016.10.011
5. Peabody T, Bordoni B. Anatomy, Bony Pelvis and Lower Limb, Fascia Lata. Treasure Island: StatPearls Publishing; 2020.
6. Naik A, Patel A, Bothra N, Panda L, Naik MN, Rath S. Endoscope-assisted harvest of autogenous fascia lata in frontalis suspension surgery: A minimally invasive approach revisited. Indian J Ophthalmol. 2018;66(3):440-4. DOI: 10.4103/ijo.IJO_819_17
7. Peng M, Sussman RD, Escobar C, Palmerola R, Pape DM, Smilen SS, et al. Rectus Fascia Versus Fascia Lata for Autologous Fascial Pubovaginal Sling: A Single-Center Comparison of Perioperative and Functional Outcomes. Female Pelvic Med Reconstr Surg. 2020;26(8):493-7. DOI: 10.1097/SPV.0000000000000761
8. Evereklioglu C. ‘Kite-tail’ fascia lata strips technique: frontalis suspension using a non-endoscopic minimally invasive single-thigh incision approach. Br J Ophthalmol. 2012;96(4):570-5. DOI: 10.1136/bjophthalmol-2011-300400
9. Batista KT, Cauhi AF. Reabilitação Cirúrgica da Face Paralisada. Rev Bras Cir Plást. 2007;22(4):253-60.
10. Erni D, Lieger O, Banic A. Comparative objective and subjective analysis of temporalis tendon and microneurovascular transfer for facial reanimation. Br J Plast Surg. 1999;52(3):167-72. DOI: 10.1054/bjps.1997.3060
11. Viterbo F, de Paula Faleiros HR. Orthodromic transposition of the temporal muscle for facial paralysis: made easy and better. J Craniofac Surg. 2005;16(2):306-9. DOI: 10.1097/00001665-200503000-00019
12. Giovannetti F, Barbera G, Priore P, Pucci R, Della Monaca M, Valentini V. Fascia Lata Harvesting: The Donor Site Closure Morbidity. J Craniofac Surg. 2019;30(4):e303-6. DOI: 10.1097/SCS.0000000000005223
13. Vitali M, Canevari FR, Cattalani A, Grasso V, Somma T, Barbanera A. Direct fascia lata reconstruction to reduce donor site morbidity in endoscopic endonasal extended surgery: a pilot study. Clin Neurol Neurosurg. 2016;144:59-63. DOI: 10.1016/j.clineuro.2016.03.003
1. Hospital das Clínicas da Faculdade de Medicina de Botucatu, Cirurgia Plástica,
Botucatu, SP, Brazil
Corresponding author: Balduino Ferreira de Menezes Neto Rua Hortênsia, 291, Apto 802, Jardim Bom Pastor, Botucatu, SP, Brazil, Zip Code: 18607-650, E-mail: balduino.neto@unesp.br
Article received: August 11, 2021.
Article accepted: December 13, 2021.
Conflicts of interest: none.










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter