

Case Report - Year 2023 - Volume 38 -
Galactorrhea after breast augmentation: case report and literature review
Galactorreia após mamoplastia de aumento: relato de caso e revisão da literatura
ABSTRACT
Introduction: Augmentation mammoplasty is one of the most frequently performed surgeries in plastic surgery. Among its rarer occurrences are galactorrhea, spontaneous milk output by the papilla, and galactocele, a collection of milky material in the surgical bed. There is little literature on this extremely rare occurrence, and through this article, we conduct a literature review and report on a case operated in our service.
Case Report: We present a case of a 35-year-old patient who underwent breast augmentation surgery via the inframammary fold, with an implant placed in the subglandular plane, which evolved, on the thirtieth postoperative day, with galactorrhea exteriorized through the incision, and we propose a treatment for such intercurrence. Six months after the operation, the breasts were symmetrical, without signs of contracture or additional alterations; the patient was satisfied with the result and without new episodes of galactorrhea or galactocele.
Conclusion: Although rare, with an incidence of less than 1%, galactorrhea can occur as a postoperative complication, and knowledge about it, as well as the forms of treatment, will benefit both patient and surgeon.
Keywords: Galactorrhea; Breast implantation; Mammaplasty; Breast diseases; Reconstructive surgical procedures; Case reports
RESUMO
Introdução: A mamoplastia de aumento é uma das cirurgias mais frequentemente realizadas na cirurgia plástica. Entre suas intercorrências mais raras, está a galactorreia, saída de leite pela papila de forma espontânea, e o galactocele, uma coleção de material leitoso no leito cirúrgico. Pouca literatura existe sobre esta raríssima intercorrência e por meio deste artigo realizamos uma revisão da literatura e relato de um caso operado no nosso serviço.
Relato de Caso: Apresentamos um caso de uma paciente de 35 anos que foi submetida a cirurgia de mamoplastia de aumento via sulco inframamário, com implante alocado no plano subglandular, que evoluiu, no trigésimo dia pós-operatório, com galactorreia exteriorizada pela incisão, e propomos um tratamento para tal intercorrência. Com seis meses de pós-operatório, as mamas se encontravam simétricas, sem sinais de contratura ou alterações adicionais, paciente satisfeita com o resultado e sem novos episódios de galactorreia ou galactocele.
Conclusão: Embora rara, com uma incidência de menos de 1%, a galactorreia pode ocorrer como intercorrência pós- operatória e o conhecimento desta, bem como as formas de tratamento, irá beneficiar tanto paciente como cirurgião.
Palavras-chave: Galactorreia; Implante mamário; Mamoplastia; Doenças mamárias; Procedimentos cirúrgicos reconstrutivos; Relatos de casos
INTRODUCTION
Augmentation mammoplasty using implants is a procedure performed with high frequency worldwide. In 2020 alone, 1,624,281 surgeries were performed, according to the International Society of Aesthetic Plastic Surgery (ISAPS)1. Although very safe, it is not free from complications. Some of these complications are well known, such as hematoma, seroma, capsular contracture, infection, unsightly scarring, and poor positioning of implants, and some are uncommon, such as galactorrhea2,3.
Galactorrhea and galactocele can occur in up to 0.96% of patients undergoing breast augmentation with implants. On average, they take 15-90 days to manifest. Galactocele was defined as the accumulation of milk in the surgical pocket, and this content can be drained spontaneously through the surgical wound4. Galactorrhea is defined as the spontaneous excretion of milk by the papilla without sucking stimulus3.
The cause of postoperative galactorrhea and galactocele has not yet been fully elucidated. It is believed that the trigger may be due to the increase in prolactin due to surgical stimulation or nerve compression of the rib cage. Some theories point out that the mechanical compression of the implants on the gland or even the effect of other medications taken by the patient may be responsible for such intercurrence5.
Treatment is based on prolactin inhibitors such as bromocriptine4,6,7 and may be associated with percutaneous or open surgical drainage of the galactocele7. Because it is a rare intercurrence that the surgeon may face one day, we present a case experienced in our service, as well as the treatment scheme used and the postoperative follow-up with 10 months of surgery.
OBJECTIVE
To present a case of galactocele in a patient who underwent breast augmentation with implants, to report on the management of the case, applied treatment, and results.
CASE REPORT
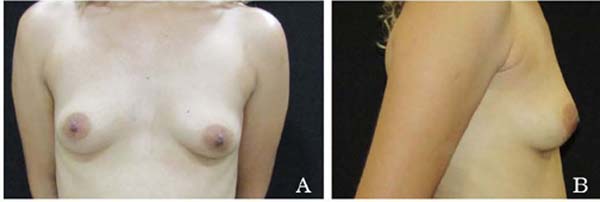
We report the case of a 35-year-old female patient, complaining of hypoplastic breasts and desire for breast augmentation (Figures 1A and 1B), admitted to Hospital Irmãos Penteado, Dr. Ricardo Barouldi, in Campinas, S P. She had two previous pregnancies and had stopped breastfeeding one year after the surgery. The patient tended to form a keloid scar without other important antecedents. In October 09, 2020 a breast augmentation surgery was performed using 300ml textured implants in the subglandular plane and via an access route in the inframammary fold. The postoperative period was uneventful, and the patient evolved adequately.
Thirty days after the surgical procedure, a milky secretion (Figure 2) drains spontaneously through the surgical wound without pain, fever, or other symptoms, in addition to bilateral galactorrhea. Cabergoline 0.5mg every 12 hours was used, associated with cefadroxil 500mg every 12 hours for 48 hours. This regimen of cabergoline pulses was repeated 45 days after the surgical procedure. With this approach, the patient presented a progressive decrease in secretion drained by the surgical wound, completely ceasing 60 days after the surgery.
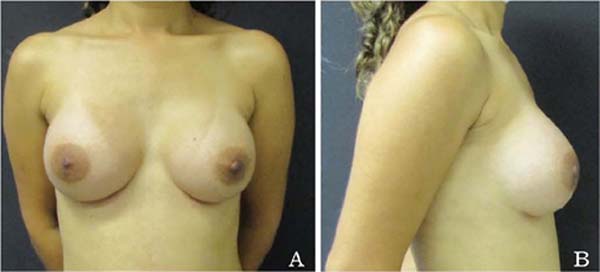
The patient evolved with a hypertrophic scar in the region of the inframammary fold, which was treated with four sessions of intra-cicatricial infiltration of triamcinolone acetate. Six months after the operation (Figures 3A and 3B), the breasts are symmetrical, without signs of contracture or additional alterations; the patient is satisfied with the result and without new episodes of galactorrhea or galactocele.
DISCUSSION
Galactorrhea is a rare complication that occurs in breast augmentation surgeries. It was first described in 1971 as the spontaneous release of milk not associated with breastfeeding6,7. Initially, it can be confused with infection or breast abscess due to edema, pain, and the appearance of secretion8. Among the causes of galactorrhea, we can highlight nipple stimulation, pregnancy, use of medications that increase prolactin production, iatrogenic hyperprolactinemia above 27ng/ml, thyroid alterations, renal alterations, and prolactinomas9.
Among the causes of postoperative galactorrhea after breast augmentation, it has been suggested that there is an increase in prolactin in response to lactotrophic cells in the anterior pituitary, which leads to milk production; prolactin can increase up to 5 times due to the surgical stimulus9. Another theory indicates that the surgery’s irritation of the costal nerves leads to a suppression of the hypothalamic axis, with a decrease in the release of dopamine4. However, the systematic review published by Sharma & Basu4 found that not all patients had high levels of prolactin in the postoperative period.
We can point out some risk factors associated with galactorrhea, such as the last pregnancy close to the surgery period, greater number of pregnancies, previous lactation, and use of contraceptive medication.
Regarding the implant insertion plane, those allocated in a subglandular position and periareolar incision are more related to galactorrhea4. According to Chun & Taghinia10, this is due to the obstruction of some galactophoric ducts in the breast. The onset of symptoms is reported in an average of 15 days and may manifest after 90 days after surgery3,6.
Some tests can be routinely used, such as measurement of serum levels of prolactin, Beta-HCG, complete blood count, C-reactive protein, thyroid tests, and IV Sudan test to determine milk6,7,11. Regarding imaging tests, ultrasonography, secretion cultures, and pituitary magnetic resonance in case of hyperprolactinemia above 100ng/ml4 may be necessary for diagnostic confirmation.
After confirmation of the condition, we must proceed with drug treatment. Authors propose different approaches, including using bromocriptine at a dose of 2.5mg twice daily as the first line and cabergoline 0.5mg 1-2 tablets per week and as the second line2,4,11. Antibiotic treatment may also be included due to the risk of infection associated with the implant4,11, dopamine inhibitors, leukotriene inhibitors, to avoid the chance of capsular contracture6, and explant with pocket washing4,6,11.
In the literature review, we found that most published studies are case reports similar to this one: two case series and one systematic review.
We believe that expanding the number of studies on this topic will be important to unify behaviors and minimize this intercurrence.
CONCLUSION
Galactorrhea and galactocele are rare complications of breast augmentation. With an adequate diagnosis and early treatment, we managed to treat it without changing the outcome of our surgeries. More investigations are needed regarding this rare intercurrence to unify conducts and minimize complications.
1. Hospital Irmãos Penteado, Serviço de Cirurgia Plástica Dr Ricardo Barouldi, Campinas,
São Paulo, Brazil
Corresponding author: Raphaela Silveira do Amaral Av. José Bonifácio, 2001, Campinas, S P, Brazil. Zip code: 13092-305 E-mail: rapha_samaral@hotmail.com







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter