

Original Article - Year 2023 - Volume 38 -
The L-shaped mastopexy
A mastopexia de aumento em L
ABSTRACT
Introduction: The mastopexy with implants and L-shaped scarring aims to correct grades I to II breast ptosis using implants in retroglandular space and retromuscular dual plane space, at the same surgical time. The objective is to describe the experience with the L-augmentation mastopexy technique, analyzing complications and reoperations.
Method: Retrospective study of 123 patients with mild to moderate breast ptosis, operated using the L-augmentation mastopexy technique from January 2011 to November 2021.
Results: The mean age of patients was 35.6 years. The average volume of implants used was 315ml (range 175 to 600ml). The placement of the prosthesis was in retroglandular (46.5%) and dual plane retromuscular space (53.5%). The average operative time was two hours and fifty-four minutes. The main complications presented were superficial dehiscence (7.3%), recurrence of ptosis (7.3%) and unsightly scars (5.7%). Surgical reviews took place in 13 patients (10.5%).
Conclusion: Safe and effective mastopexy technique with implant in the treatment of mild to moderate breast ptosis, providing well designed breasts with reduced L-shaped scars.
Keywords: Reconstructive surgical procedures; Mammaplasty; Breast; Breast implants; Breast implantation
RESUMO
Introdução: A mastopexia com implantes e cicatriz em L visa corrigir ptoses mamárias graus I a II com utilização de implantes em espaço retroglandular e retromuscular dual plane, no mesmo tempo cirúrgico. O objetivo é descrever a experiência com a técnica de mastopexia de aumento em L, analisando complicações e reoperações.
Método: Estudo retrospectivo de 123 pacientes com ptose mamária leve a moderada, operadas pela técnica de mastopexia de aumento em L no período de janeiro de 2011 a novembro de 2021.
Resultados: A média de idade das pacientes foi de 35,6 anos. O volume médio de implantes utilizado foi de 315ml (variação de 175 a 600ml). O posicionamento da prótese foi em espaço retroglandular (46,5%) e retromuscular dual plane (53,5%). O tempo médio operatório foi de duas horas e cinquenta e quatro minutos. As principais complicações apresentadas foram deiscências superficiais (7,3%), recorrência da ptose (7,3%) e cicatrizes inestéticas (5,7%). Revisões cirúrgicas aconteceram em 13 pacientes (10,5%).
Conclusão: Técnica de mastopexia com implante segura e eficaz no tratamento da ptose mamária leve a moderada, proporcionando mamas bem projetadas com cicatrizes reduzidas em L.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Mamoplastia; Mama; Implantes de mama; Implante mamário
INTRODUCTION
Breast ptosis is characterized by liposubstitution of the parenchyma and loss of elasticity in the skin, the suspensory ligaments of the breasts, and a fall in the nipple-areolar complex. There are several causes of ptosis, such as pregnancy, lactation, variations in body weight, developmental deformities, gravity, aging, and the late effect of silicone implants.
The first publication on the use of prosthesis and mastopexy at the same surgical time was in 1960 by Gonzales-Ulloa1. In 1968, Dempsey & Latham2 presented the technique of implant inclusion in the retromuscular plane. The article on the dual plane technique for positioning the breast implant in a concomitant retroglandular and submuscular space was introduced by Tebetts3 in 2001. Several augmentation mastopexy techniques for correcting ptosis in a single surgical procedure addressing this issue have been reported in the literature.
Skin sagging and sagging breasts can cause low self-esteem and emotional changes in patients. The most used classification for breast ptosis was described by Regnault4 and is based on the position of the nipple concerning the inframammary fold. Augmentation mastopexy elevates the breast tissue and the nipple-areola complex and removes excess skin associated with silicone implants, seeking to correct asymmetries and preserving the sensitivity and physiology of the breasts.
Mastopexy with an implant is a challenge for the plastic surgeon, as in the vast majority of cases, the patient’s aesthetic demands are high in terms of shape, volume, positioning, quality of the scars, and durability of the results.
Women suffering from severe breast ptosis require further removal due to excess skin and consequent extensive scarring in the shape of an inverted T. Several authors have developed techniques with reduced scars, aiming to eliminate the horizontal medial scar, which can become hypertrophic.
We used the marking based on the Chiari Jr mammoplasty technique with a short scar at L5,6, initially described for breast reduction and refined over time by the author7.
For patients with mild and moderate degrees of breast ptosis, mastopexy techniques are used with circumareolar, vertical, or L-shaped scars. Silicone prostheses can be placed in the retroglandular, subfascial, or dual-plane retromuscular space.
OBJECTIVE
This study aims to describe the experience with the L-enlargement mastopexy technique, using implants in an anteromuscular or retromuscular dual plane position, and to analyze the complications.
METHOD
Retrospective study of 123 women with mild to moderate breast ptosis who underwent L-shaped mastopexy from January 2011 to November 2021. Surgeries were performed on patients at the private clinic, and Hospital do Servidor Público Municipal de São Paulo. Paper submitted to the Research Ethics Committee (CEP), with CAAE 54894522.6.0000.5442.
Marking
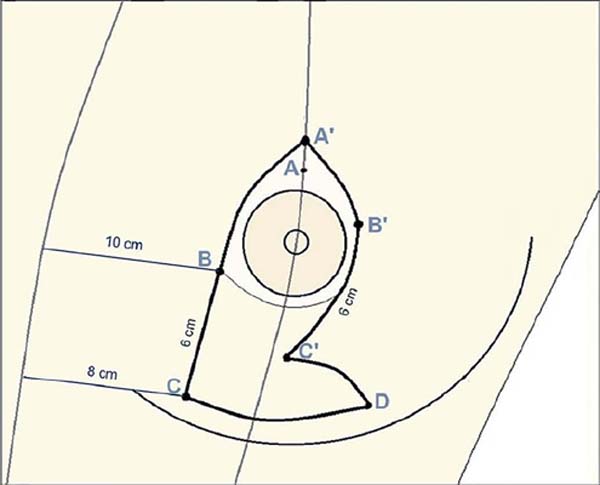
Surgery based on the Chiari Jr technique, whose preoperative marking is shown in Figure 1 and has the following order:
1st Point A’ - the sternal and mid-mammary lines are initially drawn with the patient in an orthostatic position. Point A is placed in the reflection of the inframammary fold, and point A’ is positioned 2cm above, usually 17-18cm from the sternal notch.
2nd Point C - with the patient lying down, the breast is pulled laterally, and point C is defined at a distance of 8cm from the sternal line and 1cm above the inframammary fold.
3rd Point B - positioned 6cm above point C and 10cm from the sternal line, with the skin stretched laterally. The BC line delimits the medial column.
4th Point B’ - defined at the level of the nipple and drawn on the lateral margin of the areola.
5th Point C’ - placed 6cm from point B’ towards C, with the skin stretched medially and superiorly. Line B’C’ forms the lateral column and is positioned higher than line BC.
6th Point D – by bringing lines BC and B’C’ closer together, the vertical of the breast is obtained (6cm), and to remove the inferior cutaneous excess, point D is marked laterally, 2cm above the inframammary fold. The line CD delimits the horizontal of the L.
Surgical technique
Incision made on the CD line, just above the inframammary fold and prepectoral dieresis up to the point A’, for placement of the implant in the retroglandular or subfascial space. For inclusion in the retromuscular plane, a subglandular detachment is performed up to the lower margin of the areola (dual-plane II), followed by an incision and divulsion of the pectoralis major muscle and the creation of an inferolateral loop (Figure 2). Review of hemostasis with luminous valve under direct vision.
The nipple-areolar complex has a pedicle with a superomedial base. Removing excess skin and breast tissue is based on previous marking and bidigital clamping. Construction of the nipple-areolar complex begins with Benelli’s “round block”8 using polyglecrapone 3.0 thread, followed by continuous intradermal synthesis with polyglecrapone 4.0 thread. After reviewing the hemostasis, the vertical and horizontal lines are closed by approximating the subcutaneous tissue with 3.0 nylon thread and suturing the skin with 4.0 polyglecrapone thread. The mastopexy is completed, and the scar is reduced to an L shape, as shown in Figure 3.
RESULTS
In the last ten years, 123 patients were operated on using the augmentation mastopexy technique with the resulting L- shaped scar. Of these, 113 women (91.9%) were from the private clinic, and another 10 patients (8.1%) were from the Hospital do Servidor Público Municipal/SP. The age group ranged from 19 to 64 years, with an average of 35.6 years, and the patients had a body mass index below 30kg/m2 (average body weight 62kg, ranging from 51-83kg).
The breast implants used had a textured surface, round shape, cohesive silicone gel content, high profile (32.4%), and super high profile (67.6%). The average volume of 315ml, with a minimum of 175ml and a maximum of 600ml, and in the latter, the prostheses were exchanged after a previous breast augmentation surgery, according to the medical evaluation and the patient’s wishes. The implant locations occurred in the dual-plane retromuscular space (53.5%) and anteromuscular space (46.5%).
Associated liposuction was performed in 14 patients, and an average volume of 1,800ml of fat was removed. Combined abdominoplasty was performed in 10 patients, with a flap removed weighing an average of 1,200g. The anesthetic techniques used were general anesthesia (72.3%), local anesthesia (19.6%), and epidural anesthesia (8.1%). The average operative time computed was two hours and fifty-four minutes, excluding associated surgeries.
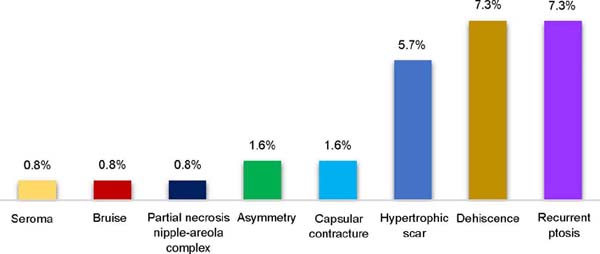
The most frequent complications were superficial dehiscence, which occurred in nine patients (7.3%), seven cases had unsightly scars (5.7%), two patients developed capsular contracture (1.6%), two others had breast asymmetry (1.6%), one case of seroma (0.8%), one case of hematoma (0.8%) and one patient evolved with partial necrosis of the areola (0.8%). Recurrence of ptosis occurred in nine cases (7.3%). There were no cases of infection, rupture, or venous thromboembolism (Graph 1). Unaesthetic scarring and ptosis recurrence were the main reasons for reoperations, which occurred in 12 patients (10.5%). Postoperative follow-up for an average period of two years.
DISCUSSION
There is a considerable rate of dissatisfaction with sagging in the late postoperative period, identified in the reduction of the upper pole and excess tissue in the lower pole, in addition to small dehiscence and cicatricial enlargement. Several authors have published techniques related to the anatomical positioning of the prosthesis, with low rates of complications.
Calobrace et al.9 reported a revision rate of 23.2% in 332 cases of augmentation mastopexy. The most reported complications were capsular contracture (3.9%), scarring (3.3%), and ptosis recurrence (3.3%).
Stevens et al.10 published reoperation rates of 16.9% in 615 patients undergoing mastopexy with an implant. The most common complications were healing (5.7%) and dehiscence (2.9%).
A meta-analysis study in 2014, carried out by Khavanin et al.11, of 4,856 augmentation mastopexies found rates of reoperations (10.6%), recurrent ptosis (5.2%), unsightly scars (3.7 %), capsular contracture (2.9%), asymmetry (2.9%), seroma (1.4%), hematoma (1.4%) and infection (0.9%).
Ono & Karner12, in 2018, published the mastopexy technique and implants in a submuscular pocket and inferolateral loop, superomedial pedicle, and resection of the breast parenchyma. Reoperation rate of 16% in 266 patients but reduced to less than 5% according to the learning curve. Inferolateral muscle support is used to prevent the recurrence of ptosis.
In the article on the submuscular double-pocket implant for augmentation mastopexy, published by Procópio et al.13, of the 80 operated cases, there were reoperations (6.1%), epitheliolysis at the junction of the vertical and horizontal scars (2.5%), hematoma (1.3%), capsular contracture (1.3%) and seroma (1.3%).
Graça Neto & Daniel14 present the original technique of muscle support in the lower pole of the breast, where the implant is placed in a double space, with the lower part of the prosthesis retromuscular and the upper part in the subglandular plane. Out of 640 operated patients, the main complications were excess skin (3%), unsightly scars (3%), and partial necrosis of the areola (2%).
Sgarbi et al.15 reported 21 complications (22.8%) in 192 patients who underwent the mastopexy technique with the splitting of the upper pectoral muscle and lower muscle band, seroma (3.6%), unsightly scars (2.6%), breast asymmetries (2.6%) and suffering from nipple-areola complex (1.5%) were the observed complications.
In the present study, several women had the implants placed in the retroglandular space under an inferior muscular belt, following the approach described by Daniel. There is a current tendency to place the prosthesis in a dual-plane retromuscular space, which offers better coverage and vascularization, provides low rates of capsular contracture, lower rates of visualization or palpation of the implant (“rippling”) together with the elaboration of the inferolateral pectoral loop, the technique disclosed by Ono, which provides muscle support and less implant migration.
To reduce the incidence of postoperative pseudoptosis, complete the length of the vertical scar at 6 cm. The excess skin on the lower pole of the breast is removed, leaving an L-shaped final scar.
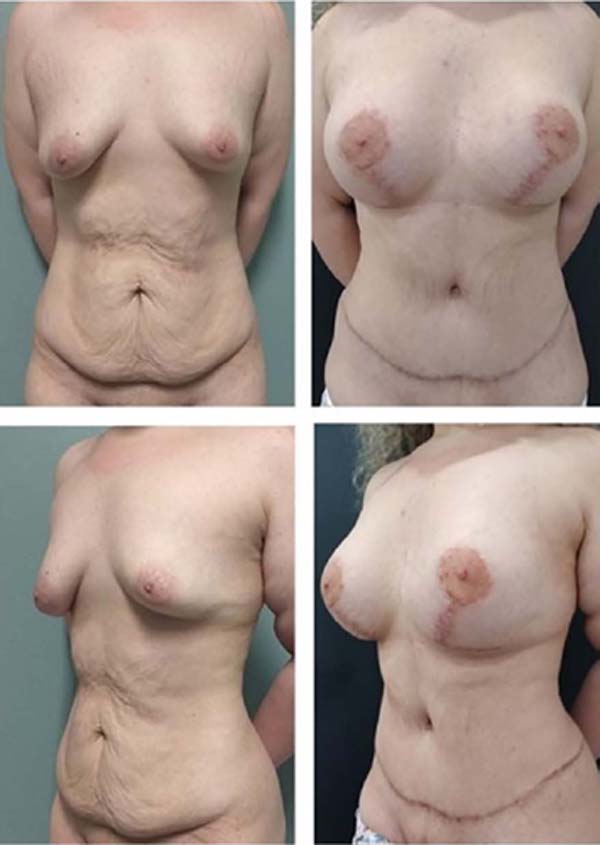
Most of the women in this study had symmetrical breasts with adequate volume and shape (Figures 4, 5, 6, 7, 8, 9). The continuous improvement of technique and the excellence of the surgeon favor the success of the operation16.
CONCLUSION
L-mastopexy is safe and reproducible, with complication rates consistent with the literature. This technique effectively corrected mild to moderate ptosis, promoting projected breasts with well-positioned and reduced scars.
2. Hospital do Servidor Público Municipal, Preceptor de Residência em Cirurgia Plástica,
São Paulo, SP, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, Membro Titular, São Paulo, SP, Brazil
Corresponding author: Roberto Luiz Sodré Rua Antonio Alves Barril, 355/191, J. Anália Franco, São Paulo, S P, Brazil. Zip code: 03338-000 E-mail: roberto.sodre@uol.com.br




















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter