

Case Report - Year 2023 - Volume 38 -
Urinary retention after lipoabdominoplasty: case report
Retenção urinária após lipoabdominoplastia: relato de caso
ABSTRACT
Introduction: Postoperative urinary retention may predispose to permanent bladder
damage. Risk factors include type of anesthesia, type of surgery, and use of anticholinergics,
analgesics, and opioids. Once the lesion is established, complementary urodynamic tests
are essential for etiological diagnosis and treatment. The objective of this study is to report
a case of a patient with urinary retention in the postoperative period of lipoabdominoplasty.
Keywords:
Urinary retention; Lipoabdominoplasty; Urinary bladder, underactive; Postoperative complications; Analgesics, opioid
Case Report: 27-year-old female patient, without comorbidities or use of continuous
medication. She underwent lipoabdominoplasty and evolved postoperatively with urinary
retention and bladder distention, diagnosed as detrusor contractility and sensitivity deficit
in the urodynamic study. She was maintained in outpatient follow-up with the surgical
team and Urology, with a progressive reduction in urinary catheter use and complete
removal in eight months of follow-up.
Discussion: The objective of aesthetic plastic
surgery is to improve the physical appearance of the body. It is subject to complications
like other surgical procedures, and pain seems to be the most frequent. Urinary retention
may be secondary to the use of opioids, and its diagnosis in the postoperative period of lipoabdominoplasty still has some obstacles. Plication of the rectus muscle diastasis,
liposuction, and the use of a compressive abdominal belt make it difficult to identify a
possible bladder distention. An episode of bladder overdistention can result in significant
morbidity.
Conclusion: The present report demonstrated the good evolution of a patient
who developed urinary retention in the postoperative period of lipoabdominoplasty.
The main diagnostic hypothesis was that it was secondary to the use of opioids.
RESUMO
Introdução: A retenção urinária pós-operatória pode predispor a danos permanentes à
bexiga. Os fatores de risco incluem tipo de anestesia, tipo de cirurgia e
uso anticolinérgicos, analgésicos e opioides. Uma vez que a lesão está
estabelecida, os exames complementares urodinâmicos são fundamentais para
diagnóstico etiológico e tratamento. O objetivo deste trabalho é relatar
caso de paciente com quadro de retenção urinária no pós-operatório de
lipoabdominoplastia.
Relato de Caso: Paciente de 27 anos, sexo feminino, sem comorbidades ou uso de medicamentos
contínuos. Foi submetida a lipoabdominoplastia, e evoluiu no pós-operatório
com quadro de retenção urinária e bexigoma, diagnosticada como
acontratilidade detrusora e déficit de sensibilidade no estudo urodinâmico.
Manteve acompanhamento ambulatorial com a equipe cirúrgica e a Urologia, com
redução progressiva do uso do cateter vesical e retirada completa em oito
meses de seguimento.
Discussão: O objetivo da cirurgia plástica estética é melhorar o aspecto físico do
corpo. Como os demais procedimentos cirúrgicos, está sujeita a complicações
e a dor parece ser a mais frequente. A retenção urinária pode ser secundária
ao uso de opioides e seu diagnóstico no pós-operatório da
lipoabdominoplastia ainda possui alguns obstáculos. A plicatura da diástase
do músculo reto, a lipoaspiração e o uso de cinta abdominal compressiva
dificultam a identificação do possível bexigoma. Um episódio de
hiperdistensão da bexiga pode resultar em morbidade significativa.
Conclusão: O presente relato demonstrou boa evolução de paciente que desenvolveu
retenção urinária no pós-operatório de lipoabdominoplastia. A principal
hipótese diagnóstica foi de ser secundária ao uso de opioide.
Palavras-chave: Retenção urinária; Lipoabdominoplastia; Bexiga inativa; Complicações pós-operatórias; Analgésicos opioides
INTRODUCTION
Surgical interventions may predispose to complications related to the surgery, the anesthetic procedure, and pharmacological side effects1.
Postoperative urinary retention is frequent in many patients and can permanently damage the bladder since it compromises its anatomy and predisposes it to motility problems and atony2,3,4,5. In addition, this situation favors the occurrence of recurrent urinary infections since incomplete emptying of the bladder and the resulting volume of post-void residual urine facilitates bacterial proliferation1.
Risk factors for its incidence include the type of anesthesia, type of surgery (mainly anorectal), male gender, elderly, intravenous hydration therapy, use of anticholinergic drugs, analgesics, and opioids, and loss of privacy4,6.
Previously, the diagnosis of this condition was suspected by clinical symptoms (inability to urinate and pain) and physical examination (palpable and distended bladder) and confirmed through bladder catheterization. More recently, the use of portable ultrasound to measure the volume of the bladder allowed earlier diagnosis, in addition to being a fast, effective, and non-invasive method5.
Complementary urodynamic tests are essential once the lesion is established to assess bladder disorders and choose the most appropriate treatment objectively7.
OBJECTIVE
This study aims to report the case of a patient with urinary retention in the postoperative period of lipoabdominoplasty.
CASE REPORT
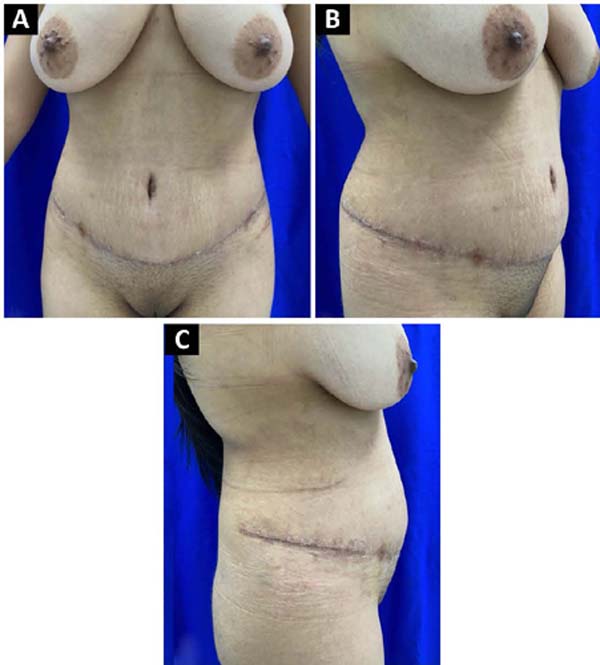
A female, 27-year-old patient without comorbidities or use of continuous medication. Former smoker with a surgical history of cesarean delivery. Preoperatively, she had a body mass index (BMI) of 27.8 kg/m2 and tests within normal parameters, classified as ASA II (Figure 1).
She was admitted to the hospital asymptomatic. She underwent general anesthesia associated with spinal anesthesia and antibiotic prophylaxis with 2g cefazolin. In addition, indwelling bladder catheterization was performed. She underwent lipoabdominoplasty lasting four hours, and there were no surgical or anesthetic complications during this period.
The patient evolved well in the immediate postoperative period, with no complaints. Hydration, antibiotic therapy, analgesics, opioids, antiemetics, and prophylactic measures for venous thromboembolism (VTE) were prescribed.
On the first postoperative day, she urinated spontaneously after removing the indwelling urinary catheter and reported only nausea and mild pain in the liposuctioned region. She had a good surgical evolution, with no evidence of complications. She was discharged with an indication of antibiotic therapy (first-generation cephalosporin) for seven days, analgesics, opioids (500mg of paracetamol associated with 30mg of codeine every eight hours if severe pain), and antithrombotic prophylaxis with subcutaneous enoxaparin 40mg/day for seven days.
On the second postoperative day, she complained of dysuria, urinary frequency, and vesical tenesmus. She underwent a urinalysis1, showing only nitrite and mild hematuria (10,000 red blood cells/ml). Phenazopyridine and 750mg/day levofloxacin antibiotic were prescribed for seven days.
She returned to the office on the fourth postoperative day for medical evaluation. She reported improvement in symptoms after two days of the new therapy, with satisfactory bladder emptying and without dysuria. The dressing was changed on that occasion, and the drain was removed.
On the 10th postoperative day, she went to the hospital complaining of urinary retention. She reported still using 500mg of paracetamol associated with 30mg of codeine every eight hours. On physical examination, she had a palpable and painful bladder in the suprapubic region. An ultrasound of the total abdomen and abdominal wall was performed, showing bladder distention. She underwent a relief urinary catheter, with immediate drainage of 2500ml of urine and immediate pain relief.
In an interconsultation with Urology, she was instructed to keep a long-term urinary catheter with occlusion of the probe every four hours, with a good response. Magnetic resonance imaging of the lumbar spine excluded possible traumatic complications related to spinal anesthesia, and computed tomography of the abdomen excluded possible traumatic complications related to lipoabdominoplasty.
She was discharged the following day with a urological follow-up and request for an outpatient urodynamic study. The study revealed the absence of detrusor contraction, reduced bladder sensitivity, and preserved bladder compliance and capacity. The Urology team then recommended intermittent relief bladder catheterization (every eight hours) and bladder training with physiotherapy.
She maintained outpatient follow-up with the Plastic Surgery (Figure 2) and Urology team, with a progressive reduction in the use of relief bladder catheter and complete removal in eight months of follow-up, after recovery of urination capacity.
The study protocol was approved by the Ethics and Research Committee (Opinion number 5,922,090). Patient images in this publication have informed consent.
DISCUSSION
The objective of aesthetic plastic surgery is to improve the physical aspect of the body of the individual who feels uncomfortable with a certain appearance characteristic. However, like other surgical procedures, it is subject to complications.
Pain seems to be the most frequent among the complaints reported in the postoperative period, according to some authors8,9. The main strategies to control this symptom involve using common analgesics, anticholinergics, anti-inflammatories, and opioids. These medications can occasionally interfere with urination pathways, since this complex mechanism involves many neural connections.
Opioids are major contributors to the development of post-surgical urinary retention. This is due to its side effects, which include relaxation of the detrusor muscle, with a corresponding increase in maximum bladder capacity4. They can also increase the tone and amplitude of urinary sphincter contractions and reduce ureteral contractions10. As already well established in the literature, urinary relief catheterization can be used to prevent permanent complications to the urinary tract since a single episode of bladder overdistension can result in significant morbidity4.
However, the early diagnosis of urinary retention in the postoperative period of lipoabdominoplasty still has some obstacles. The plication of the rectus muscle diastasis, associated with liposuction and using a compressive abdominal belt, make it difficult to identify a possible bladder distention. In addition, in the immediate postoperative period, swelling of the operative area, local pain, or even the occurrence of seroma is expected, further impairing the clinical diagnosis.
Portable ultrasound seems to be an effective method for identifying this complication in the inhospital environment5. After discharge, objective guidelines and the rational use of opioids seem to help with prevention, but these measures are still insufficient in some cases.
The present report demonstrated the good evolution of a patient who developed urinary retention in the postoperative period of lipoabdominoplasty. Given the clinical picture, after an etiological investigation, the main diagnostic hypothesis was that it was secondary to the use of opioids.
CONCLUSION
Urinary retention is a relatively frequent complication in postoperative patients. Some individuals, at first, may be oligosymptomatic, and postoperative symptoms may further mask this condition, which delays diagnosis and predisposes to permanent consequences.
1. Serviço de Cirurgia Plástica Osvaldo Saldanha,
Santos, SP, Brazil
2. Universidade Santo Amaro, São Paulo, SP,
Brazil
Corresponding author: Taisa Szolomicki Av. Ana Costa, 146, Cj 1201-04, Gonzaga, Santos, S P, Brazil Zip Code: 11060-000 E-mail: tszolomicki@hotmail.com






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter