

Case Report - Year 2023 - Volume 38 -
Cutaneous traction as a complement to the parascapular flap in major cancer loss: case report
Tração cutânea como complemento ao retalho paraescapular em grande perda oncológica: relato de caso
ABSTRACT
Introduction: Squamous cell carcinoma (SCC) is a malignant epidermal keratinocyte
tumor closely related to sun exposure. When diagnosed, through biopsy, its staging,
tumor resection with oncological safety margins must be performed, and lymph
node dissection and treatment of metastases, if present, may be performed.
Case
Report: Skin traction is reported as a complement to the parascapular flap, used
reconstructively after the excision of a large SCC in the left shoulder.
Conclusion: The
technique used proved effective for the satisfactory correction of large dehiscence
in the postoperative period of the parascapular flap, promoting partial closure of the
defect, reduced time to perform, and correction of the residual defect in a single step.
Keywords: Surgical flaps; Skin neoplasms; Carcinoma, squamous cell; Reconstructive surgical procedures; Surgery, plastic
RESUMO
Introdução: O carcinoma espinocelular (CEC) é um tumor maligno dos queratinócitos
epidérmicos e está intimamente relacionado à exposição solar. Quando
diagnosticado, por meio de biópsia, deve ser realizado seu estadiamento,
ressecção tumoral com margens de segurança oncológica, podendo ser feito
esvaziamento ganglionar e tratamento de metástases, caso presentes.
Relato de Caso: Reporta-se a utilização da tração cutânea como complemento ao retalho
paraescapular, utilizado reconstrutivamente pós excisão de CEC de grande
dimensão em ombro esquerdo.
Conclusão: A técnica utilizada mostrou-se eficaz para correção satisfatória de grandes
deiscências em pós-operatório de retalho paraescapular, promovendo
fechamento parcial do defeito, tempo reduzido para realização e correção do
defeito residual em tempo único.
Palavras-chave: Retalhos cirúrgicos; Neoplasias cutâneas; Carcinoma espinocelular; Procedimentos cirúrgicos reconstrutivos; Cirurgia plástica
INTRODUCTION
Squamous cell carcinoma (SCC) is a malignant tumor of epidermal keratinocytes that invades the dermis and can generate metastases. It has a higher incidence in individuals over 50 years old, with the main etiologies being: sun exposure and carcinogenic agents1.
The most affected sites are the scalp, back of the hands, lower lip, ears, face, buccal mucosa, and external genitalia1.
The clinical characteristics of the lesion range from erythematous papules or plaques with a scaly or crusted surface to hyperkeratous nodules, often with a verrucous appearance1.
A biopsy confirms the diagnosis, and the staging is performed according to the TNM table. In addition to tumor resection, lymph node dissection and treatment of metastases may occur, if necessary2.
This study aims to describe the suture by Góes et al.3 as a complement to the parascapular flap4, used reconstructively after the excision of SCC.
CASE REPORT
The patient, 50 years old male, white civil construction assistant, sought care due to an ulcerated lesion measuring 5.7 x 5.2 cm on the left shoulder, with the appearance of SCC, confirmed by biopsy (Figure 1).
Preoperative tests (laboratory and cardiological) were performed, which were normal and with surgical risk grade 1. After the demarcation of the tumor area with oncological safety margins, the patient underwent general anesthesia and was positioned in the right lateral decubitus position (Figure 2).
The lesion was resected with oncological margins and sent for anatomopathological examination, with the result of invasive squamous cell carcinoma grade 3 of differentiation, invasion to the subcutaneous tissue (Class V), free margins, no angiolymphatic involvement detected, and no perineural invasion.
A parascapular flap4 was demarcated, measuring (21cm x 6.5cm), based on the parascapular artery, a branch of the left axillary artery (Figure 3).
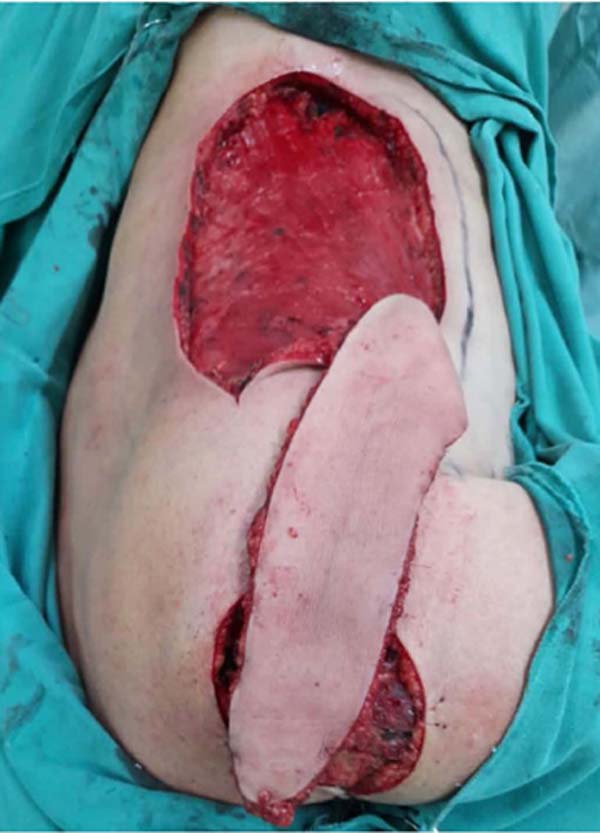
The flap was elevated and rotated to reach the left shoulder region (Figures 4 and 5) and sutured to its new bed with nylon 3-0 and 4-0. This completely covered the tumor resection area.
The donor area of the flap was repaired by advancing the local flaps and suturing with 3-0 and 2-0 nylon (Figure 6).
After 24 hours, there was a suture dehiscence in the distal part of the flap and pain at its extremity due to venous congestion (Figure 7).
Cyclic and continuous traction of the cutaneous margins3 was used to close the bloody area and a small part was partially left for healing by second intention (Figure 8).
The distal end of the parascapular flap4 with venous congestion evolved to dry necrosis of an area larger than the initial one, which did not require debridement (Figure 9).
The patient was followed up, requiring radiotherapy treatment, with good evolution and adequate surgical wound healing (Figures 10 and 11).
DISCUSSION
The literature cites numerous methods for covering the reported defect, including skin graft5, latissimus dorsi myocutaneous flap6, trapezius myocutaneous flap7, and microsurgical flaps8. The preference for the parascapular flap4 is due to its greater ability to cover large areas, in addition to muscle preservation compared to other myocutaneous flaps, which generate great functional loss, requiring long periods for compensation, as is the case with the latissimus dorsi6 and trapezium flaps7.
Treatment with microsurgery8 is highly specialized, and our Service does not have the proper equipment, so we cannot perform it.
Due to the patient’s profession (civil construction assistant), the skin graft5 would inevitably suffer loss with the work activity, causing a poor prognosis.
The parascapular flap4 is described in the literature with a length of up to 30 cm. Considering the patient’s height of 1.82m, the length of the flap was adequate for its use, with the advantage of ensuring thick coverage - resistant to trauma and without muscle mobilization, allowing the patient to return to activities early.
Wound closure by skin traction, recommended in 2004 by Carlos Henrique Fröner S. Góes et al.3, was performed in the ward on the second postoperative day to correct the dehiscence. For this purpose, Prolene 2 thread was used, with insertion in the area posterior to the detachment, exteriorizing it inside the wound, towards the other margin, and the thread is wrapped through the needle with a catheter segment. A “U” was completed bilaterally by returning the thread in reverse. The two threads on each side were pulled simultaneously, bringing the edges together with a certain point of maximum tension. Through repeated traction, greater skin relaxation and the possibility of partial closure were promoted. This avoided performing a new procedure in a surgical center, which would cause great emotional stress to the patient and higher costs to the institution that maintains it.
The suture proved an efficient method, promoting partial closure of the defect (80% of the dehiscence area), ease, and reduced time to perform in addition to one-time residual defect correction.
CONCLUSION
The suture proposed by Góes et al.3 proved to complement the parascapular flap4 in covering the resection of large tumor areas, with the advantages of being low-cost and easy to perform. In addition, skin traction provided satisfactory correction of large postoperative dehiscence using a parascapular flap4.
1. Hospital de Câncer de Campo Grande Alfredo
Abrão, Campo Grande, MS, Brazil
2. Universidade Federal de Mato Grosso do Sul,
Campo Grande, MS, Brazil
3. Associação Beneficente Santa Casa de Campo
Grande, Campo Grande, MS, Brazil
4. Universidade Estadual de Mato Grosso do Sul,
Campo Grande, MS, Brazil
Corresponding author: Franco Silva Martinez Rua Petrópolis, 585, Caiçara, Campo Grande, MS, Brazil Zip Code: 79090-234 E-mail: francosmartinez99@gmail.com
























 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter