

Review Article - Year 2023 - Volume 38 -
Nasal tip reconstruction: case reports and historical review
Reconstrução da ponta nasal: relatos de casos e revisão histórica
ABSTRACT
Traumatic amputations of the nasal tip are disfiguring injuries, which determine important social rejection, imposing additional suffering on the patient and those already caused by the wound and its functional limitations resulting from the trauma. Such defects represent a challenge for plastic surgeons, and several techniques can be adopted to treat this type of defect. This work shows three cases of traumatic amputation exclusively of the nasal tip with their respective treatments. They present a historical review and discussion of the different techniques used for nasal tip reconstruction, comparatively evaluating and emphasizing the technical evolution in plastic surgery armament.
Keywords: Reconstructive surgical procedures; Nose; Nose deformities, acquired; Wound healing; Facial injuries
RESUMO
As amputações traumáticas da ponta nasal são lesões desfigurantes, que determinam importante rejeição social, impondo ao paciente um sofrimento adicional, além daqueles já causados pela ferida e suas limitações funcionais decorrentes do traumatismo. Tais defeitos representam um desafio para os cirurgiões plásticos, e existem diversas técnicas que poderão ser adotadas para tratar este mesmo tipo de defeito. Neste trabalho são mostrados inicialmente três casos de amputação traumática exclusivamente da ponta nasal com seus respectivos tratamentos, para em seguida apresentar uma revisão histórica e discussão das diversas técnicas utilizadas para reconstrução da ponta nasal, avaliando comparativamente e enfatizando a evolução técnica no armamentário da cirurgia plástica.
Palavras-chave: Procedimentos cirúrgicos reconstrutivos; Nariz; Deformidades adquiridas nasais; Cicatrização; Traumatismos faciais
INTRODUCTION
Traumatic amputations of the nasal tip are disfiguring injuries, which determine important social rejection, imposing additional suffering on the patient and those already caused by the wound and its functional limitations resulting from the trauma.
Such defects represent a challenge for plastic surgeons, and several techniques can be adopted to treat the same type of defect. In this work, three cases of traumatic amputation exclusively of the nasal tip will be shown (without affecting other aesthetic subunits) and their respective treatments to present a historical review and discussion of the techniques used to reconstruct the nasal tip. The procedures were performed at the Federal Hospital of Andaraí, in Rio de Janeiro-RJ, in 2017 (case 1) and 2020 (case 3), and at the Universitary Hospital Pedro Ernesto, Rio de Janeiro-RJ, in 2018 (case 2).
Case 1
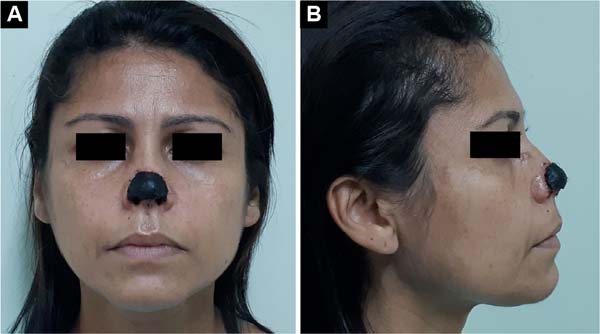
Female patient, 25 years old, sought the plastic surgery service with complaints of nasal deformity and respiratory obstruction. The patient reported an episode of trauma in childhood (preschool age) with loss of full thickness in the region of the nasal tip. The patient did not know how to inform about the trauma mechanism but reported that, at the time, the wound had been treated conservatively, healing by the second intention.
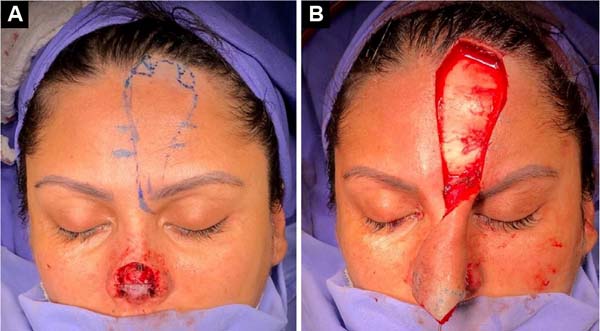
Upon examination, the patient had complete loss of the nasal tip and soft triangles, with scar retraction leading to stenosis of the nasal external valve (Figures 1A and 1B). The patient’s surgical treatment was planned and carried out in 3 stages. In the first surgical procedure, the scarring bands and underlying fibrosis were released, allowing the assessment of the magnitude of the nasal lining deficiency (Figure 2A). A paramedian flap was then made, folded over itself, to cover and line the nasal tip and smooth triangles (Figure 2B).
After 4 weeks, the second surgical procedure was performed, separating the covering and covering, the latter being kept connected to the supratrochlear pedicle. After refinement of both flaps (liner and cover), the tip was structured with auricular conchal cartilage, and the already refined cover flap was then sutured again over the nasal tip. After an interval of another 4 weeks, the supratrochlear pedicle was sectioned with repositioning of the eyebrow, thus achieving the result of the reconstruction (Figures 3A and 3B).
Case 2
Male patient, 35 years old, reports having suffered superficial nasal trauma (blunt injury) complicated with infection during adolescence. On that occasion, after antibiotic treatment to resolve the infectious process, the bloody wound on the nasal tip received skin autograft. Upon examination, the patient had no nasal tip, causing extreme aesthetic dissatisfaction for the patient, but without functional complaints (Figures 4A and 4B). A nasal reconstruction was then performed in three stages, as described in case 1, with recomposition of the aesthetic unit of the nasal tip (Figures 5A and 5B).
Case 3
A 41-year-old female patient sought the plastic surgery service with complete necrosis of the nasal tip. The patient reported being the victim of a canine bite about 3 weeks before, with complete avulsion of the nasal tip. When assisted at emergency service, the nasal tip that suffered avulsion was sutured to the nose as an autologous composite graft. The patient then evolved with complete necrosis of the nasal tip (Figures 6A and 6B). The necrotic tissues were debrided, and the area cleaned, with the reconstruction being postponed to a second time, pending the delimitation of the area of necrosis.
Six months after the initial care, and after the scar retraction had stabilized (Figures 7A and 7B), the patient underwent a 3-step reconstruction of the nasal tip, in the same way as in cases 1 and 2, according to the technique advocated by Menick1,2: elevation of the folded median flap to cover and line the first stage (Figures 8A and 8B); separation and refinement of the lining and covering with cartilaginous structuring and resuture of the covering flap in the second stage (Figures 9A and 9B), and finally section of the vascular pedicle in the third stage, reaching the final result (Figures 10A and 10B).
DISCUSSION
The nasal tip occupies a central position on the human face, determining aesthetic characteristics that make up the patient’s identity. In traumatic amputations, full-thickness losses will require replacement of the lining (under the smooth triangles, at the delicate junction with the nasal columella), as well as the cartilaginous structure and skin coverage, to guarantee an esthetic reconstruction.
Due to its permanent exposure, we know that the nose is extremely susceptible to trauma and photodamage, which contributes to the tumors’ appearance. Throughout its history, plastic surgery has developed several techniques for repairing nasal tip injuries. These techniques, for the most part, include flaps that make it possible to replace the skin in partial-thickness defects, basically promoting the replacement of the skin coverage on the nasal tip.
The bilobed flap, initially described by Esser3, is referred to by several authors4,5 as the flap of choice for covering the tip of the nose and should preferably be laterally pedicled. In 1967, Rieger6 described the lengthening of the classic McGregor7 glabellar flap up to the nasal tip. Two years later, Rintala & Asko-Seljavaara8 presented the rectangular advancement flap with compensation triangles excised on both sides of the base (Burow’s triangles) so that the flap reached from the root to the tip along the nasal midline.
Among other cutaneous flaps to cover the tip, we can mention using nasolabial flaps with a superior pedicle9 or inferior10 and Snow’s horizontal “J” flap11. In the last two decades, some myocutaneous flaps for the nasal tip have also been described, mono or bipedicled in the nasal branch(es) of the angular artery12-16, whose coverage reach can reach the columella17.
In the case of traumatic injuries that lead to full-thickness defects, we know that the nasal tip is the most exposed area of the face when treating patients with facial trauma. Blunt injuries tend to be more frequent due to causes related to traffic accidents. However, lacerations resulting in loss of substance are also common, not only due to traffic accidents but also to bites by domestic animals and injuries from firearms, generating more complex deformities to be reconstructed.
The reconstruction in these cases will involve the total recomposition of the lost segment, guaranteeing the volume and shape necessary to recompose the aesthetic subunit. The flaps described above, which only guarantee skin coverage, will be insufficient, as in these cases, there is a need to replace the lining and cartilaginous structure of the segment amputated by the trauma.
Historically, the oldest technique was described by Sushruta Samhita18 (around 600 BC), who uses the midfrontal flap based on the supratrochlear vessels bilaterally, the so-called Indian flap. The tip of the Indian flap, folded over itself, with the thickness of the frontal aponeurotic galea and the subcutaneous tissue, fulfilled the function of restoring volume to the amputated nose. In the case of defects restricted to the nasal lobe, the tendency towards progressive bulging due to contraction of the soft parts in this very thick flap (a “pin-cushioning” phenomenon) could even contribute to improving the aesthetic result by mimicking a rounded nasal tip. - which certainly does not occur in the more proximal defects.
In Italy at the end of the 15th century, Alessandro Benedetti apud Jewett & Baker19 described the so-called Italian method, using a pedicled flap on the arm, thus allowing the transfer of subcutaneous tissue to replace the loss of volume, in addition to the skin for coverage. This technique was recommended until the beginning of the 20th century, being defended by Nélaton20.
With the advent of the First World War, Gillies-Filatov tubes21 were also used as a volume replacement method, requiring several surgical steps for tissue transfer and subsequent refinement. A modern variant of these old methods of tissue transfer was described by Abbenhaus22, who, claiming to avoid scarring and facial mutilation, described a flap using the abdomen as the initial donor area and the wrist as an intermediate transfer site up to the nose. In the interwar period, Rethi apud Kirshner23 also described sequential tissue transfer techniques for the nasal tip from nasolabial flaps.
After the Second World War, a simpler solution indicated for small losses of nasal tip substance in its convexity (not involving smooth triangles) was described by Cronin24 in 1951, in which the nasal dorsum skin is transferred to the tip. At the same time, the frontotemporal flap by Schmid25 was described, which allows thinner skin to be applied to the nasal tip region, with more aesthetic results involving lining and structuring. However, this last flap is non-axial, less reliable, and requires multiple stages for its preparation.
This is precisely the greatest limitation of these techniques that involve the transfer of non-axial pedicled flaps to replace volume in the nasal tip: the need for multiple surgical stages - first to transfer the tissue and then to make the necessary refinements to obtain a better result. acceptable. The techniques described above serve to mimic the convexity of the nasal tip, in its most superior and anterior portion. However, we know that the anatomy of the nasal tip is delicate, especially in the region surrounding the infratip and the smooth triangles, whose refined design in the nostril rim and transition to the nasal vestibule is difficult to reproduce using these conventional techniques.
In an attempt to circumvent this limitation, Gillies26 described the association of a conch chondrocutaneous composite graft (used for structuring and lining) to the “up-and-down” flap (a variant of the frontal flap) in 1943. However, we know that composite grafts have limitations related to their maximum size. There are reports of successfully grafted large segments27,28, or of techniques that allow greater reliability29 in the “take” of composite grafts, but the vast majority of authors agree that composite grafts are unreliable for repairing defects larger than 15mm30.
At the beginning of the millennium, the systematization of the paramedian flap in three stages, as proposed by Menick1,2, through a technically simple and easily reproducible method, allowed a greater refinement of the surgical result. Adding one more intermediate stage, in which the paramedian flap is refined, allowed for delicate and aesthetic results in the nostril rim of smooth triangles and at the entrance to the nasal vestibule, without the gross convexity that characterizes flaps folded over themselves.
In addition, this additional intermediate stage also makes it possible to reposition and/or add structural grafts, making the results of nasal tip repairs more predictable, ensuring a better result in the long term. Because it uses an axial flap (paramedian flap based on the ipsilateral supratrochlear artery), the technique proved to be very reliable, reproducible, and with a low rate of complications.
CONCLUSION
Despite the various technical possibilities that emerged in the plastic surgery armamentarium with its historical evolution, today, the systematization of nasal reconstruction has made reconstructive plastic surgery more reliable and reproducible techniques, exemplified in the cases above by the paramedian flap in three stages, thus allowing the rehabilitation of these patients through more aesthetic and refined results.
1. Universidade do Estado do Rio de Janeiro,
Faculdade de Ciências Médicas, Rio de Janeiro, RJ, Brazil
2. Hospital Universitário Pedro Ernesto, Serviço
de Cirurgia Plástica, Rio de Janeiro, RJ, Brazil
3. Hospital Federal do Andaraí, Serviço de
Cirurgia Plástica, Rio de Janeiro, RJ, Brazil
Corresponding author: Michel Luciano Holger Toledano Vaena, Av. Prof. Manuel de Abreu, 444, 2º and., Vila Isabel, Rio de Janeiro, RJ, Brazil, Zip Code: 20550-170, E-mail: michel.vaena@hotmail.com





















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter