

Case Reports - Year 2001 - Volume 16 -
Giant Lipoma of the Thigh: Case Report
Lipoma Gigante de Coxa - Relato de Caso
ABSTRACT
This paper reports the case of a 77-year-old patient who had a giant thigh lipoma for 20 years, emphasizing its location, size, and the surgical management.t.
Keywords: Lipoma; lower limbs; surgical treatment
RESUMO
É relatado um caso de lipoma gigante de coxa com 20 anos de evolução, enfatizando-se sua localização, dimensões e o tratamento cirúrgico empregado.
Palavras-chave: Lipomas; membros inferiores; tratamento cirúrgico
Lipomas are the most frequent soft tissue rumors, and may occur wherever there is fat tissue(l). They affect mostly women, particularly in their trunks, upper limbs, and cervical regions; large rumors are rare(2).
They are usually identified as visible soft tumors, and they do not cause serious symptoms. Depending on their size and location, they may cause functional, impairment, or pressure-associated symptoms, as when they occur, for example, in lower limbs or next to viscera (l,2) .
This paper presents the case report of a 77 year-old patient who had a giant thigh lipoma, focusing on its location, size, surgical management, and postoperative course.
CASE REPORT
M.E.S.D., a 77-year-old white retired nurse, widowed born and living in São Paulo, reported that 20 years before, a 3-cm-wide node appeared on the anterior region of her left thigh. It was soft, mobile, painless, did not produce secretion, and did not affect walking.
She reported that her lesion and left thigh had grown progressively over the years, though she experienced no pain. Six months before, however, the patient had sought medical care because she felt moderate to intense pain in her lower left limb, especially while walking, and difficulties during flexion, adduction and abduction of the thigh. She had a history of hypertension, which had been controlled with medication, and had undergone a hysterectomy 30 years before.
Physical examination revealed a marked enlargement of the lower left limb: her thigh was 60 cm in diameter (Figs. 1a-c). The tumor presented a slightly hardened consistency to touch, had a smooth surface, moved in relation to deeper tissues, was painless, and located in the anterior surface of the thigh. The patient presented difficulties in the passive and active abduction, adduction and flexion of the thigh. Laboratory and complementary tests (electrocardiogram and thoracic X-ray) were normal. A simple x-ray of the affected limb showed an extensive tumorous mass of low radiological density, free of calcifications. Nuclear magnetic resonance revealed an extensive intramuscular tumorous mass in the anterior region of the left thigh and a small portion in the posterior region, around the femur. The tumor had a well-defilled capsule, did not adhere to deep tissues, which suggested an extensive lipoma (Figs. 2a -c).
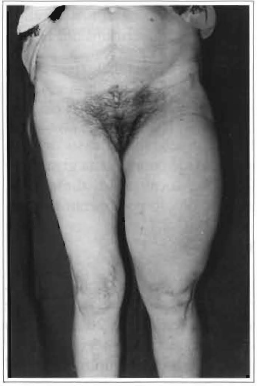
Fig. 1a -Preoperative; anterior view.
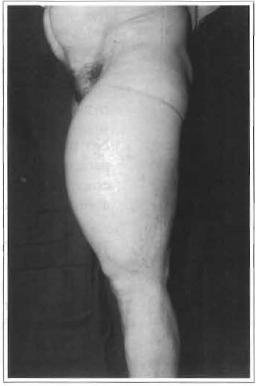
Fig. 1b -Preoperative; posterior view.
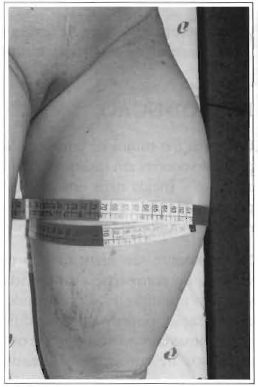
Fig. 1e -Pre-operative; left thigh with 60 cm diameter.
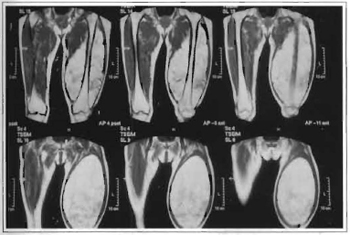
Fig. 2a -Nuclear magnetic resonance image of the tumor. Anterior view.
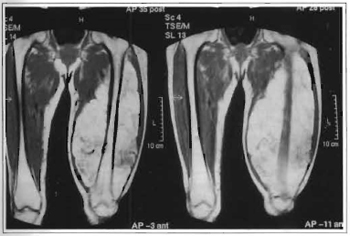
Fig. 2b -Nuclear magnetic resonance image of the tumor. Enlarged anterior view.
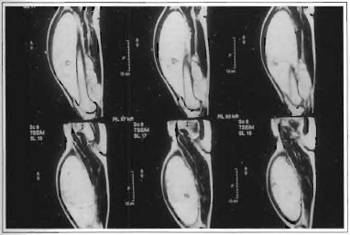
Fig. 2c -Nuclear magnetic resonance image of the tumor. Profile view.
The patient was referred to surgery, which was performed with peridural anesthesia and sedation. An incision in the medial face of the left thigh (Fig. 3), below the cellular subcutaneous tissue, permitted the identification of an extensive encapsulated multilobulated tumorous mass, with benign morphological features - which confirmed the findings of the nuclear magnetic resonance. It was located directly under the sartorius muscle, had displaced the rectus femoris muscle posteriorly, compressed the vastus sideis, vastus medialis, adductor longus and gracilis muscles. The tumor was in an unusual location: intermuscular. The tumorous mass also presented a posterior extension that surrounded the femur.
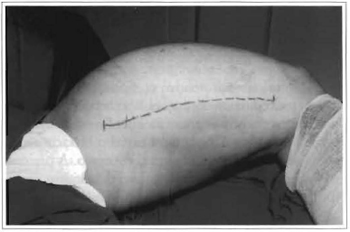
Fig. 3 -Intraoperative period. Marking of the incision on medial face of left thigh.
The tumor was almost fully removed. Only a small portion remained because it was located behind the femur, in the high upper third. This is a site which is difficult to access surgically and removal could offer significant risks to the patient. The decision of the medical team to not extend the surgical resection was based on the benign features of the tumor and on the surgical risk it might have represented for the patient (Figs. 4-7).

Fig. 4 -Presence of extensive tumor (thick arrow), intermuscular location, below sartorius muscle (thin arrow), with displacement of recrus femoralis (asterisc) and gracilis muscles (triangle).

Fig. 5 -Well-encapsulated extensive tumor, multilobulated, with aspect suggesting lipoma (sartorius muscle behindretractors).

Fig. 6 -Intraoperative period showing removal of extensive rumor.

Fig. 7 -Resulting space after removal of tumor (sartorius muscle pulled away). Note the atrophied rectus femoralis muscle (arrow) and exposure of the femur upper third (asterisc).
No muscular tissues had to be removed, as they had neither been affected nor infiltrated by the nunor; they were merely atrophied or had been displaced from their usual anatomical locations.
Excess skin resulting from tumorous growth was and the incision was closed without tension in its subdermal and intradermal layers (Figs. 8-10).

Fig. 8 -Marking of excess skin to be resected due to "tumoral extension".

Fig. 9 -Area resulting from excision for resecting excess skin.

Fig. 10 -Final suture.
The surgical sample was sent for histological study, which confirmed the diagnosis of lipoma. The nunor, mass removed weighed 2,500 g, was 40 cm long and 20 cm wide (Fig. 11).
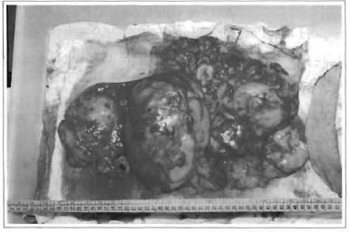
Fig. 11 -Surgical specimen. Note the extension of the giant lipoma and excess skin resected.
The patient did not present any complications during or after the surgical procedure. She was discharged on the third postoperative day. Thirty days after the surgery, it was possible to see significant cosmetic and functional improvements in the affected limb. Six months after surgery, the patient did not present any signs or symptoms indicating recurrence of the tummor (Fig. 12).

Fig. 12 -6 month postoperative period. a) Anterior view. b) Profile view.
DISCUSSION
Lipomas are common mesenchimal benign tumors, usually single, soft, and well encapsulated They may appear in any region of the body, including internal organs(3,4). They vary in size and do not weigh more than a few grams . They occur more frequently in young adults and in women. They are normally sub cutaneous; they may, however, be intermuscular, intramuscular or in joints(5). They are usually asymptomatic.
Giant lipomas, on the other hand, are rare benign tumors in fat tissue (2,4-7), which occur most frequently in the cervical region, thorax, and lower limbs (inguinal region and thigh). They are usually single, and evolve over many years asymptomatically, except when they compress adjacent tissues such as muscles and nerves(6,8). When they occur in lower limbs, they may affect walking due to their excessive size and weight(7).
When clinical diagnosis indicate their presence, a number of imaging techniques, such as ultrasound, computerized tomography and magnetic resonance, may provide additional information to aid diagnosis and surgical planning. However, only histological studies may provide final diagnostic confirmation (2,5,9,10).
Some authors(6) recommend electromyography, both in the pre-and postoperative periods, to evaluate possible changes in electrical conductivity of the sciatic nerve and in the electrical activity of muscular tissues of the affected limb, considering that, due to their size, these tumors may compress and affect these structures. Electromyography is useful in these cases for surgical planning and postoperative follow-up of the functional recovery of affected limb.
The presence of (inclusion, sebaceous, pilonidal) cysts, xanthomas and other papulonodular lesions (such as neuromas, rheumatoid nodes, etc.) enable the differential diagnosis of lipomas. In the case of giant lipomas, the differential diagnosis is made chiefly with soft tissue tumrs (nerves, vessels, tendons, muscles) and bone nunors. The possibility of malignant tumors, such as sarcomas(5) should always be eliminated.
Soft tissue sarcomas (rhabdomyosarcomas, for instance) are normally asymptomatic (pain is associated to large tumors), poody delimitated, with early metastases; they are irregular and diffuse on nuclear magnetic resonance. In contrast, osteosarcomas are usually painful and accompanied by edema; in conventional radiography, they produce images that are typical of destructive bone lesions, calcifications and periostal reactions; they look hypervascularized in angiographies (11) . Malignant transformations (liposarcoma) are rare and should be investigated when tumors grow fast, are recurrent or when there are skin ulcers(4,5).
The treatment of lipomas varies according to their location. The absence of tumors should always be confirmed, because they would lead to different surgical planning and procedures, depending on each individual case.
As to giant lipomas located in lower limbs, complete surgical exeresis is usually recommended, whenever possible, particularly for the tumors located in the subcutaneous, intermuscular or intramuscular tissues, as they usually cause functional and/or vascular changes(2,5). When muscles are invaded or impaired, in addition to removing the tumor, it may be necessary to remove part of the muscular tissue. When they are intermuscular, it is possible to remove tumors without affecting the adjacent muscular tissues, as in the case herein described.
The amputation of the affected limb is rare, and only indicated when there is a major impairment of the muscles, requiring extensive resections and, consequently, causing functional disability(5).
We have reported a case of extensive lipoma in the lower left limb, which weighed 2,500 g, and which, similarly to other cases described in the literature(2,4-7), led to functional disability and pain in the affected limb. Nuclear magnetic resonance was useful in the diagnosis, because of the unusual location of the tumor (intermuscular) and for surgical planning. The tumor was nearly totally resected, and it was not necessary to resect muscular tissues, as they had not been affected. The patient's walking skills improved significantly during the first postoperative month. There were no signs or symptoms of recurrence of the tumor, six months after the treatment, when significant aesthetic and functional improvements became evident in the affected limb.
Lower limb giant lipomas are rare tumors, which usually cause aesthetic deformities, compress adjacent tissues and lead to functional impairment of the affected limb. Appropriate diagnosis and surgical treatment of these tumors provide aesthetic and functional improvement of the affected limb for the patient.
REFERENCES
1. RYNDHOLM A, BERG HO. Size, site and clinical incidence of lipoma. Acta Orthap. Scand. 1983; 54:929-34.
2. HAKIM E, KOLANDER Y, MELLER Y et al. Gigantic lipomas. Plart. Reconstr. Surg. 1994; 94(2): 369-71.
3. BLOOM RA, GOMORI JM, FIELDS SI et al. Abdominal wall lipoma: CT and MRI appearance. Comput. Med. Imaging Graph. 1991; 15: 37.
4. DAVIS CJR, GRUHN JG. Giant lipoma ofthe thigh. Arch. Surg. 1967; 95: 151.
5. GAUDENZI VM, FRIZZO CJP, BEHAR SG. Lipoma gigante de coxa.R.AMRIGS.1987;31 (2): 138-40.
6. GUERRISSI J, KLERSFELD D, SAMPIETRO G. et al. Limitation of tigh function by a giant lipoma. Plast. Reconstr. Surg. 1994,94(2): 41O-l.
7. GLUSCEK S. Giant lipoma of the tigh. Wiad. Lek. 1987; 40: 845.
8. FLEEGLER EJ. Tumors of the upper extremity. In We. Grabb and J.W. Smith (Eds.), Plastic Surgery. Boston: Little Brown, 1991. p.983-4.
9. DOOMS GC, HRICAK H, SOLLITO RA. et al. Lipomatous tumors and tumors with fatty component: MR imaging potential and comparision of MR and CT results. Radiology. 1985; 157: 479.
10. FORNAGE BD, TASSIN GB. Sonographic appearances of superficial soft tissue lipomas. J. Clin. Ultrasound. 1991; 19: 215.
I - Senior member of the Brazilian Society of Plastic Surgery. Member of the Brazilian College of Surgeons. Member of the International College of Surgeons. Post-graduation degree at Professor Ivo Pitanguy's Plastic Surgery Service.
II - Assistant Professor, São Paulo University. Responsible for the Pregnancy-puerperal Oncology Outpatient Clinic of Perola Byington Hospital. Founder member of Sociedade de Patologia do Trato Genital Inferior e Colposcopia. Member of the Brazilian Federation of Gynecology and Obstetrics. Member of the International College of Surgeons.
Address for correspondence:
Eduardo Mordjikian, MD
Av. Pavao, 955 -Conj. 71
04516-012 -Sao Paulo -SP Brazil
Phone: (55 11) 240-0350 -Fax: (55 11) 5535-1849
e-mail: mordjik@uol.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter