

Original Article - Year 2023 - Volume 38 -
Quality of life and body image after bariatric and body contouring surgery
Qualidade de vida e imagem corporal após cirurgia bariátrica e de contorno corporal
ABSTRACT
Introduction: The demand for body contouring surgery after bariatric surgery is largely due to dissatisfaction with body image impaired by sagging and excess skin resulting from massive weight loss. This study aimed to evaluate the quality of life and body image of patients undergoing bariatric surgery and body contouring surgery in a private clinic.
Method: This cross-sectional study compared 4 groups of 21 patients, matched by body mass index and age before undergoing bariatric surgery. They were divided into times before/after bariatric surgery and before/after body contouring surgery, thus forming groups A, B, C, and D, respectively. The SF-36 questionnaire assessed the quality of life, and the Silhouette Scale proposed by Kakeshita to assess body image. For the significance level, p<0.05 was chosen.
Results: There was an improvement in all SF-36 domains after bariatric surgery. Patients who sought body contouring surgery had the lowest mental health component value, with little change after body contouring surgery. Almost all groups overestimated their silhouette, except for the group of 6 months after bariatric surgery, which saw itself as smaller.
Conclusion: Bariatric patients seeking body contouring surgery have lower mental health-related quality of life scores that remain lower after body contouring surgery.
Keywords: Bariatric surgery; Reconstructive surgical procedures; Body image; Quality of life; Feeding and eating disorders
RESUMO
Introdução: A procura pela cirurgia de contorno corporal após a cirurgia bariátrica se
deve em grande parte a uma insatisfação com a imagem corporal prejudicada
pela flacidez e excesso de pele decorrente da grande perda ponderal. O
objetivo deste estudo foi avaliar a qualidade de vida e a imagem corporal de
pacientes submetidos a cirurgia bariátrica e posteriormente a cirurgia de
contorno corporal em uma clínica privada.
Método: Este estudo transversal comparou 4 grupos distintos de 21 pacientes cada,
pareados por índice de massa corporal e idade antes de realizarem a cirurgia
bariátrica. Foram divididos nos tempos antes/depois da cirurgia bariátrica e
antes/depois da cirurgia de contorno corporal, formando assim os grupos A,
B, C e D, respectivamente. Foi utilizado o questionário SF-36 para avaliação
da qualidade de vida e a Escala de Silhuetas proposta por Kakeshita para
avaliação da imagem corporal. Para o nível de significância, foi escolhido
p<0,05.
Resultados: Houve melhora em todos os domínios do SF-36 após a cirurgia bariátrica. Os
pacientes que procuraram a cirurgia de contorno corporal apresentaram o
menor valor do componente de saúde mental, com pouca alteração após a
cirurgia de contorno corporal. Quase todos os grupos superestimaram a sua
silhueta, exceto para o grupo de 6 meses após a cirurgia bariátrica, que se
viu menor.
Conclusão: Pacientes bariátricos que procuram a cirurgia de contorno corporal apresentam
escores inferiores de qualidade de vida relacionada à saúde mental e que
permanecem menores após a cirurgia de contorno corporal. A distorção da
imagem corporal e expectativas irreais podem justificar esse achado.
Palavras-chave: Cirurgia bariátrica; Procedimentos cirúrgicos reconstrutivos; Imagem corporal; Qualidade de vida; Transtorno da alimentação e ingestão de alimentos
INTRODUCTION
Obesity is a major global public health problem. Overweight is present in two-thirds of the world’s population. It is a disease of chronic and multifactorial origin that can trigger various conditions such as diabetes, cardiovascular diseases, osteoarthritis, obstructive sleep apnea, hypertension, and gastroesophageal reflux. The beginning of the treatment must be conservative, through diet, psychotherapy, medication use, and physical exercises, followed by a multidisciplinary team for at least two years1,2.
Patients with initial treatment failure who have a body mass index (BMI) above 35kg/m2 and associated comorbidities or patients with a BMI>40kg/m2 are candidates for bariatric surgery (BS). The effects of BS on health are well established, improving health conditions related to comorbidities and positively impacting the quality of life3,4.
Weight loss after BS causes deformities that can bother the patient, including excess skin, compromising their body image. The desire for body contouring surgery (BCS) in post-bariatric patients is due to aesthetic complaints and functional problems such as difficulty walking and dermatitis5.
Quality of life (QoL) is a broad concept that encompasses an individual’s perception of their position in life in the context of the culture and value system in which they live and about their standard goals, expectations, and concerns. Instruments were created to directly measure the quality of life, capable of recognizing states of physical, mental, and social well-being6.
A surgical procedure that improves appearance or functionality can produce changes that can affect several spheres related to QoL, such as physical behavior, body image, psychological aspect, sexual life, and social health. Body image is a multidimensional construct by which individuals understand their personal representation of body structure and physical appearance concerning themselves and others. We can evaluate it by sizing and comparing it with objective measures of body image. Some patients are unable to recognize themselves properly, presenting body dysmorphism7.
Studies show that post-bariatric patients who undergo BCS after weight stability have improved long-term weight control8. Some studies have shown improvement in self-image but not significant improvement in QoL, which can be attributed to a postoperative period with more complications. However, few studies have evaluated the effect of BCS on quality of life and body image in post-bariatric patients, mainly in developing countries.
OBJECTIVE
This study aims to evaluate and compare the quality of life and body image perception of morbidly obese patients before bariatric surgery (BS), after BS, before body contouring surgery (BCS), and after BCS.
METHOD
The Ethics Committee approved the study for Research with Human Beings of Universidade Franciscana with protocol number 2,591,856.
The patients were over 18 years old and signed the Informed Consent Form. Patients who could not read, interpret and respond to the questionnaires and had inadequate correspondence between the groups were excluded.
Inclusion criteria for Group A consisted of morbidly obese patients immediately before bariatric surgery (BS) at a private clinic; Group B consisted of patients 6 months after BS at the same clinic; Group C consisted of patients after BS with weight stability who sought a private plastic surgery clinic for body contouring surgery (BCS) from April 2018 to April 2019, and Group D was constituted of post-BS and at least one year after BCS surgery from the same clinic. Patients in Group D had one or more previous BCSs. These patients were matched by BMI (± 2 kg/m2) and age (± 2 years) before undergoing the BS.
The self-administered SF-36 questionnaire was used to assess the quality of life (QOL), translated, and validated in Brazil by Ciconelli et al.9. It consists of 36 items, divided into 8 domains: functional capacity, physical aspects, pain, general health, vitality, social aspects, emotional aspects, and mental health. It evaluates both negative (diseases) and positive (well-being) aspects. The score is calculated on a scale of 0 to 100 points, with higher values corresponding to a better perception of QoL. Scores are individually weighted and combined to calculate physical health components (PHC), which include functional capacity, physical functioning, pain limitation, and general health and mental health components (MHC) which includes vitality, social aspects, emotional aspects, and mental health.
For body image assessment, the Brazilian Silhouette Scale Adapted for Adults, proposed by Kakeshita et al.10, was used, in which the patient is asked to choose, among the available silhouettes, the one that best represents him. The difference between the current BMI (from the chosen figure) and the real BMI (measured) is considered a discrepancy in body image because of its overestimation, underestimation, or lack of distortion.
Data were analyzed for normality using the Shapiro-Wilk test. The ANOVA test of repeated measures was performed for cases after normality, followed by the post hoc Tukey HSD test. The Friedman test was used for non-parametric data, followed by the post hoc Wilcoxon test with Bonferroni correction. IBM SPSS Version 25 software was used as a computational tool for statistical data analysis. For the statistical significance level, p<0.05 was used.
RESULTS
Sample characteristics
Twenty-one patients were included in each group (Table 1). A homogeneity test was performed, with no difference between the paired groups. Patients seek body contouring surgery (BCS) an average of 3.4 years after bariatric surgery (BS). Patients in the group after BCS had an average of 2.6 years (± 16 months) postoperatively.
| A | B | C | D | |
|---|---|---|---|---|
| Age before
BS (years - mean SD) |
37.6 (11.4) | 37.6 (11.4) | 36.3 (9.7) | 37.1 (12.0) |
| Current Age (years - mean SD) |
37.6 (11.4) | 38.0 (11.4) | 39.3 (11.3) | 39.6 (11.6) |
| BMI before BS (Kg/m2 average SD) | 42.7 (3.5) | 42.7 (3.5) | 42.7 (3.1) | 43.6 (4.5) |
| current BMI (Kg/m2 average SD) |
42.7 (3.5) | 29.2 (4.3) | 26.9 (3.9) | 25.2 (2.9) |
| Sex Feminine Masculine |
20 1 |
20 1 |
20 1 |
20 1 |
| Marital status (%) Married/SU Single/div. |
70 30 |
70 30 |
33 67 |
38 62 |
| BS time (monthsaverage SD) |
0 | 6 (1) | 41.1 (38.3) | 80.0 (52.7) |
BMI: Body Mass Index. SD: Standard Deviation. SU: Stable Union. Div: Divorced. BS: Bariatric Surgery.
Quality of life
QoL was measured and presented as mean and standard deviation values (Table 2). The values of each of the 8 domains and the domains grouped into CS, M, and PHC are presented.
| A (n=21) | B (n=21) | C (n=21) | D (n=21) | |
|---|---|---|---|---|
| Functional capacity | 38.0 (18.2)** | 90.7 (12.5) | 91.1 (9.0) | 86.1 (13.2) |
| Limitations Physical Aspects | 29.7 (42.2)** | 96.4 (11.9) | 95.2 (16.9) | 91.6 (24.1) |
| Pain limitation | 39.4 (22.1)** | 80.4 (17.5) | 71.1 (24.6) | 70.3 (20.6) |
| General state of health | 37.0 (18.2)** | 77.8 (11.3) | 83.8 (12.3) | 79.0 (16.6) |
| Vitality | 38.3 (21.8)** | 83.3 (11.8) | 70.4 (19.9) | 64.0 (20.1) |
| Social aspects | 49.4 (32.9)** | 87.5 (23.0)** | 82.3 (24.8)* | 81.5 (21.1)* |
| Emotional Aspects | 25.3 (43.3)** | 88.8 (28.5) | 74.2 (17.5)* | 76.1 (35.1) |
| Mental health | 53.1 (24.9)** | 80.7 (16.2) | 84.1 (29.0) | 71.2 (16.1) |
| Physical Health Component | 36.1 (18.7)** | 86.3 (8.5) | 84.3 (14.0) | 81.8 (15.6) |
| Mental Health Component | 41.5 (25.0)** | 85.1 (17.2) | 77.9 (19.9) | 73.2 (19.1) |
| BS time (months) | 0 | 6 (1) | 41 (38.3) | 80.0 (52.7) |
| Not valid (of the list) | 21 | 21 | 21 | 21 |
BS: Bariatric Surgery. Significance level*: p<0.05,**p<0.001.
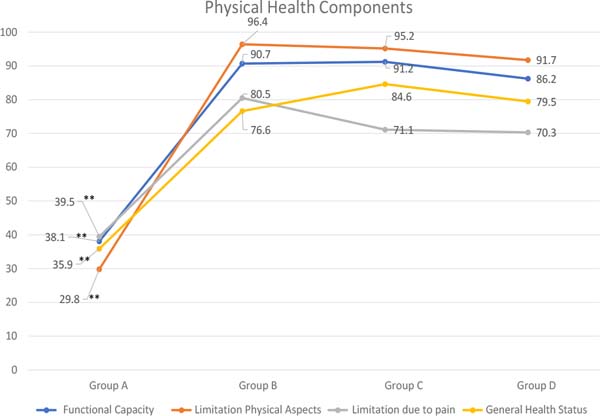
In the domains of physical health components (PHC), such as functional capacity, physical aspects, pain limitation, and general health status, all showed a significant difference between Group A and the others B, C, and D (p<0.001). No significant differences were detected between groups B, C, and D (Figure 1).
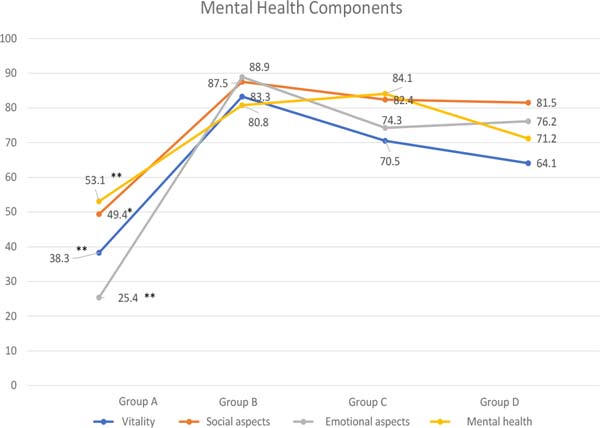
Regarding the domains of mental health components (MHC), we found significant differences in the domains of vitality, and social aspects between Group A and Groups B, C, and D. In the emotional aspects domain, Group
A was significantly different from B and D but not from Group C (Figure 2). In the mental health domain, we found Group A significantly different from Groups B and C but without significant differences from Group D.
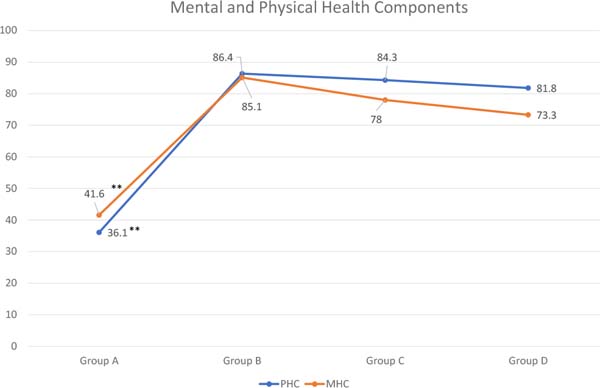
The SF-36 domains were grouped into Physical Health Components (PHC) and Mental Health Components (MHC), showing a significant difference between the group before BS and the others (Figure 3).
Body image
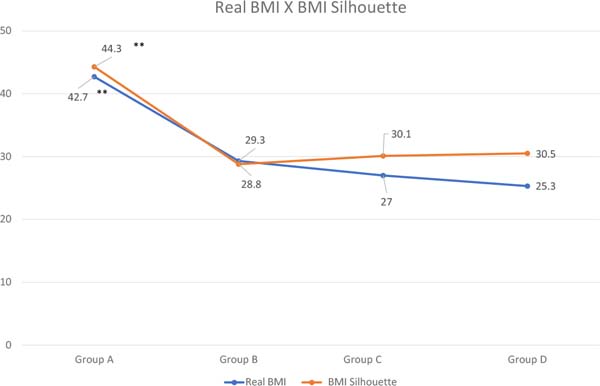
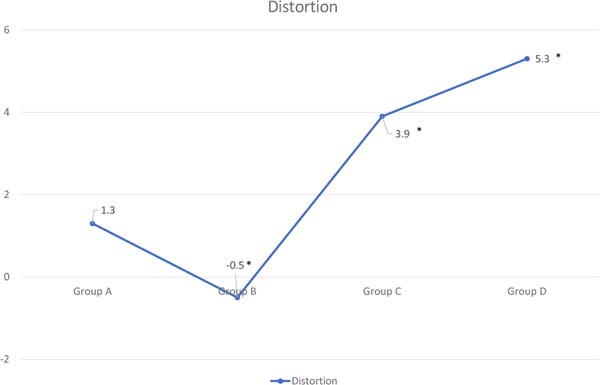
Regarding body image, the mean BMI in Group A was 42.7kg/m2, Group B 29.2kg/m2, Group C 26.98kg/m2, and Group D 25.27 kg/m2. The difference between Group A and the others was significant (Table 3).
| A | B | C | D | |
|---|---|---|---|---|
| Average (SD) | Average (SD) | Average (SD) | Mean (SD) | |
| Real BMI (kg/m2) | 42.7 (3.4)** | 29.2 (4.3) | 26.9 (3.9) | 25.2 (2.9) |
| Silhouette BMI (kg/m2) | 44.2 (3.9)** | 28.7 (3.8) | 30.1 (6.9) | 30.4 (6.2) |
| Average distortion (kg/m2) | 1.5 (5.1) | -0.5 (4.3) | 3.2 (4.4)* | 5.2 (5.3)* |
| BS time (months) | 0 | 6 (1.0) | 41.12 (38.3) | 80.0 (52.7) |
* p<0.05;**p<0.01. BMI: Body Mass Index. BS: Bariatric Surgery.
Regarding the BMI of the perceived silhouette, the average of Group A was 44.28 kg/m2, Group B 28.75 kg/m2, Group C 30.10 kg/m2, Group D30.47 kg/m2, being significant the difference chosen between Group A and the others (Figure 4). Mean distortion is the difference between actual BMI and perceived silhouette BMI.
An average distortion of 1.53 kg/m2 was identified in Group A, and in Group B, it was -0.47 kg/m2, in Group C 3.11 kg/m2, and in Group D 5.20 kg/m2, which means that patients overestimated their real image in groups A, C, and D, with significant differences between Group B with C and D. In Group A, only one patient was considered without distortion, while in Group B 6 (28%), C 1 (4.8) and D 3 (14.4%). Group B had 10 (48%) underestimates, while groups A, C, and D mostly overestimated 13 (62%), 15 (72%), and 16 (76%), respectively (Figure 5).
DISCUSSION
Bariatric surgery (BS) is already well established in the treatment of morbid obesity, reducing mortality and being effective in the treatment of comorbidities4,11. Patients report substantial improvement in obesity-related complaints, but the duration of these changes and weight maintenance or recovery are unknown12.
In this study, the quality of life (QoL) and body image (BI) of morbidly obese subjects undergoing BS and body contouring surgery (BCS) in a private clinic were evaluated, and a significant improvement was found in the physical domains of QOL after BS, with no significant differences over time. The same finding was described by Driscoll et al.13. However, there was a worsening in the QoL scores of domains related to mental health, probably due to problems related to excess skin and sagging. QoL is a construct that includes several domains related to physical and psychological health, such as body image. Patients seeking BCS feel uncomfortable with their body image, which worsens their QoL. Studies regarding QoL after BCS are inconsistent14.
Song et al.5 found lower SF-36 quality of life rates in patients who sought BCS than in patients who never sought BCS, suggesting that post-bariatric patients who did not desire BCS had already achieved BS goals and that flaccidity did not cause any functional or psychological harm.
Patients undergoing BCS continued to have lower QoL scores than the others, with scores similar to those prior to BS. This fact can be explained by some dissatisfaction or frustration after the procedure. Domains such as vitality and social aspects remained stable regardless of BCS. Emotional aspects improved after BCS.
When evaluating the body image chosen by the patients, we noticed a tendency for the groups to overestimate themselves, opting for larger silhouettes, except for the group of 6 months after BS, in which the choice of silhouette was smaller than the actual one. Patients with better quality of life and mental health tend to have a more positive self-image. These patients, at 6 months of BS, were still losing weight and realizing the benefits of BS. The body image distortion did not change after the BS, and the patients who sought the BCS showed an overestimation of the image, which was even greater in the patients who underwent the BCS. They returned to scores on similar mental health scales as before the BS.
Notably, many patients want to perform others after a body contouring procedure, changing only the focus of their complaints. Changes in body image perception may be evidence of body dysmorphic disorder, which may be related to worsening mental health components after BCS15-17.
In 2016, a qualitative study was carried out on the quality of life of post-bariatric patients, finding that their expectations regarding BCS were very high, leading to late frustration. Specific questionnaires for the bariatric population present domains about appearance and expectations, which can capture the main changes promoted by the BCS18.
The samples were matched by BMI and age before performing the BS. Only 30% of patients who undergo BS subsequently seek BCS. Cost can be considered a barrier since 80% report the desire to perform body contouring surgeries after significant weight loss. The comparison made between patients before the BS, regardless of whether they wanted to undergo body surgery or not, may be a bias in the study since the patients who have some discomfort about the image are precisely those who seek the BCS with a higher incidence of image disturbance in this population.
The 36-item Medical Outcome Short Form Health Study Questionnaire (SF-36) is a generic self-administered questionnaire that is easy to interpret and has good reproducibility. He captured changes in mental health patterns throughout morbid obesity treatment. These studies’ findings align with the literature, which identifies the unequivocal benefits of BS on QoL in the physical aspects, but not so clear in the mental health aspects. When combined with the SF-36 and the silhouette scale, it was possible to identify the association between mental health and body perception distortion in these patients.
Preparation for BS should take into account the presence of body dysmorphic disorders in this population since the body changes resulting from significant weight loss can be a source of great anxiety and, in order to be successful in BCS, the expectations of these patients must be adequate and prepared even before the BS.
Paul et al.19 describe results of physical and mental improvement in patients operated on in Poland, using the National Health Fund, in which the preparation of patients with support groups and longer hospitalizations had greater positive effects in patients with worse scores before BS. The improvement was uniform in the perception of other areas, and no patient was dissatisfied with the procedure result.
In Brazil, not all BCS procedures are covered by health plans, and, in some cases, patients even gain weight to meet BMI criteria and undergo BS.
This study had limitations due to the small sample size, which did not detect other differences. Comparisons were made with different patients who, despite the pairing, had socioeconomic variables that could interfere with general health and QoL, making multivariate analysis impossible. In addition, a generic QoL questionnaire was used, which may not capture specific small changes in this population. More studies are necessary to understand the relationship between body image and quality of life in post-bariatric patients.
CONCLUSION
Post-bariatric patients seek body contouring surgeries because they have a worse quality of life after weight stability and the appearance of sagging. With bodily procedures, there is an improvement in emotional aspects, but a worsening in mental health components associated with increased body distortion, suggesting greater dysmorphism in these patients. Better preoperative preparation and adaptation to expectations can improve the satisfaction of these patients.
1. Universidade Franciscana, Programa de
Pós-graduação em Ciências da Saúde e da Vida, Santa Maria, RS,
Brazil
2. Universidade Federal de Santa Maria,
Departamento de Cirurgia, Santa Maria, RS, Brazil
3. Universidade Federal de Santa Maria,
Departamento de Estomatologia, Santa Maria, RS, Brazil
Corresponding author: Giancarlo Cervo Rechia Rua Pinheiro Machado, 2494 Sala 402, Santa Maria, RS, Brazil., Zip Code: 97050-600, E-mail: giancarlorechia@hotmail.com











 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter