

Original Article - Year 2023 - Volume 38 -
Surgical treatment of grade III gynecomastia with the horizontal scar technique and transposition of the nipple-areolar complex - "No vertical scar"
Tratamento cirúrgico de ginecomastia grau III com a técnica de cicatriz horizontal e transposição do complexo areolopapilar - "No vertical scar"
ABSTRACT
Introduction: The demand for surgery to correct gynecomastia has increased due to the many patients undergoing bariatric treatments. Most patients require extensive removal of excess skin, and fatty tissue, repositioning the nipple-areolar complex, and adjusting the areola volume. This study aims to describe the correction technique for grade III gynecomastia using a horizontal scar without a vertical scar, with repositioning of the nipple-areolar complex.
Method: Prospective study of 27 male patients diagnosed with Simon grade III gynecomastia, operated in a private clinic between January 2013 and August 2020, using the horizontal scar technique with transposition of the nipple-areola complex and without a vertical scar.
Results: 27 patients underwent surgery over 7.5 years, all ex-obese, previously submitted to weight loss treatment. Age ranged from 17 to 74 years, mean age of 52 years. The weight of the removed parts ranged from 175 to 758 grams, an average of 376 grams. Complications were 1 case of late hematoma (3.7%), 1 case of seroma (3.7%), and 2 cases of hypertrophic scarring (7.4%).
Conclusion: Surgical treatment of grade III gynecomastia using the horizontal scar technique, without a vertical scar and with repositioning of the nippleareolar complex, proved to be effective, with low morbidity and good aesthetic results.
Keywords: Gynecomastia; Obesity; Reconstructive surgical procedures; Men; Breast; Cosmetic techniques
RESUMO
Introdução: A demanda por cirurgia para correção de ginecomastia tem aumentado em função
da grande quantidade de pacientes submetidos a tratamentos bariátricos. A
maioria destes pacientes requerem grande remoção do excesso de pele, tecido
gorduroso e reposicionamento do complexo areolopapilar, assim como adequação
do volume da aréola. O objetivo deste estudo é descrever a técnica de
correção de ginecomastia grau III através de cicatriz horizontal sem
cicatriz vertical, com reposicionamento do complexo areolopapilar.
Método: Estudo prospectivo de 27 pacientes masculinos com diagnóstico de ginecomastia
grau III da classificação de Simon, operados em clínica particular, entre
janeiro de 2013 e agosto de 2020, pela técnica de cicatriz horizontal com
transposição do complexo areolopapilar e sem cicatriz vertical.
Resultados: Foram operados 27 pacientes, num período de 7,5 anos, todos ex-obesos,
submetidos previamente a tratamento de perda de peso. A idade variou de 17 a
74 anos, média etária de 52 anos. O peso das peças removidas variou de 175 a
758 gramas, média de 376 gramas. As complicações foram: 1 caso de hematoma
tardio (3,7%), 1 caso de seroma (3,7%) e 2 casos de cicatriz hipertrófica
(7,4%).
Conclusão: O tratamento cirúrgico da ginecomastia grau III através da técnica de
cicatriz horizontal, sem cicatriz vertical e com reposicionamento do
complexo areolopapilar demonstrou ser efetivo, com baixa morbidade e bons
resultados estéticos.
Palavras-chave: Ginecomastia; Obesidade; Procedimentos cirúrgicos reconstrutivos; Homens; Mama; Técnicas cosméticas
INTRODUCTION
Gynecomastia is defined as pathological breast enlargement in men, which may be associated with the presence of fatty tissue (lipomastia) and/or excess skin1-5. The first surgical description was made by Paulo de Égina (625 AD), and the most common surgical technique is subcutaneous mastectomy via the areolar route, with or without liposuction1,5-7.
The classification used to grade gynecomastia was proposed in 1973 by Simon1:
Grade I - Small, without excess skin;
Grade II a - Moderate, without excess skin;
Grade II b - Moderate, with excess skin;
Grade III - Large, with excess skin.
The demand for surgery to correct gynecomastia has increased due to many patients undergoing bariatric treatments1. Most of these patients are grade III of the classification above and require extensive removal of excess skin, and fatty tissue, repositioning of the nipple-areolar complex (NAC), and adjustment of the areola volume5.
The techniques used for advanced cases of gynecomastia were, in most cases, adapted from reduction mammaplasty techniques in women, which can determine stigmatization of patients with large inverted “T” scars, for example5,8.
OBJECTIVE
This study aims to describe the correction technique for grade III gynecomastia using a horizontal scar without a vertical scar with NAC repositioning and to evaluate its applicability, morbidity, and surgical results.
METHOD
Prospective study of 27 male patients diagnosed with Simon grade III gynecomastia, operated in a private clinic in Curitiba-PR between January 2013 and August 2020, using the horizontal scar technique with NAC repositioning (transposition) and without vertical scar. All patients were seen up to the sixth postoperative month (PO).
Operative technique
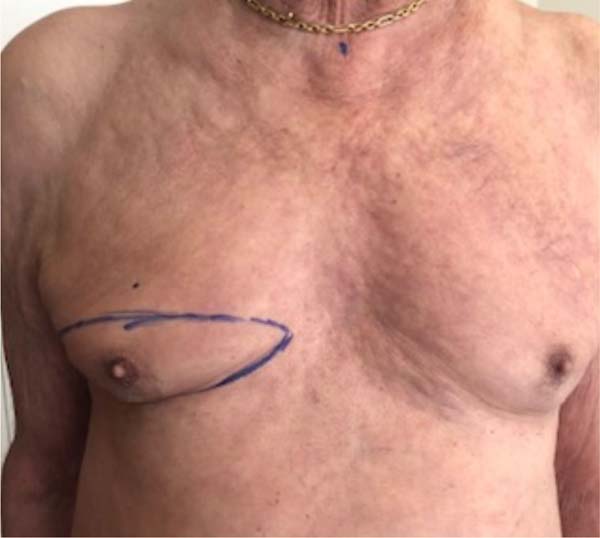
Patient in orthostatic position; marking of point “A” (Pitanguy’s point) 16cm from the sternal notch; submammary fold marking (SFM); bidigital palpation of excess skin (redundant skin) to be resected in the upper portion of the breast in the form of a transverse spindle (Figures 1 and 2) that extends from the lateral edge of the sternum to the anterior axillary line, or posterior, according to the amount of skin to be removed.
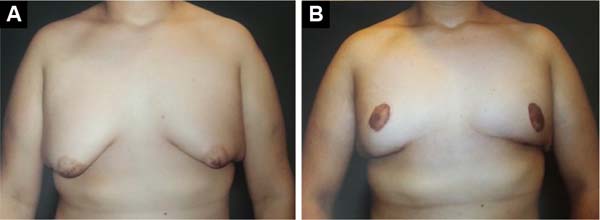
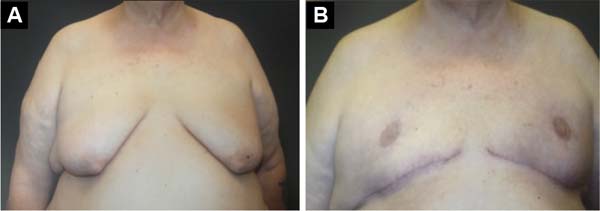
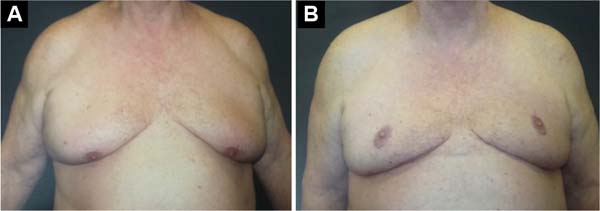
The patient is in dorsal decubitus, 2g of intravenous cefazolin under general and local anesthesia in a 1/230,000UI saline solution, and epinephrine + 20 ml of ropivacaine. Infiltration of the entire previously marked area. Use of a small areolotome, removal of excess areolar skin (Figure 3), maintenance of the NAC in the posterior pedicle based on the fourth intercostal perforating branch (Figure 4), and removal of all excess glandular and fatty tissue in a previously marked area (transverse spindle). The size of the flap is proportional to the NAC volume, 3 x 3cm at the base and length, and can reach up to 9cm. Drainage with a 4.8 suction, suturing the edges in 3 layers (Figure 4); NAC positioning at point “A” (Figures 5, 6, 7, 8, and 9).
RESULTS
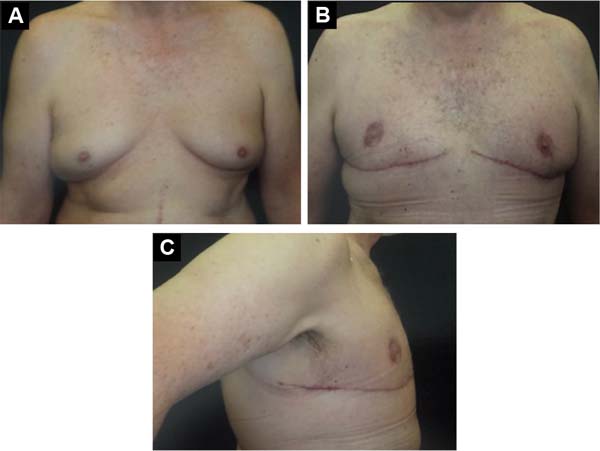
Twenty-seven patients underwent surgery over 7.5 years, all formerly obese previously submitted to weight loss treatment. Age ranged from 17 to 74 years old, mean age of 52. The weight of the removed pieces ranged from 175 to 758 grams, an average of 376 grams (Figures 10, 11, 12, 13 and 14).
The complications were:
DISCUSSION
With the increasing incidence of obesity in Western societies and the development of bariatric surgery, grade III gynecomastia and pseudogynecomastia have also increased. Overweight patients should preferentially be treated with techniques that allow a large amount of tissue to be removed and allow for the repositioning of the NAC8. The first report of the reduction mammoplasty technique without a vertical scar is credited to Passot in 1920. The excess tissue was removed in a wedge only from the pole lower breast9. This technique was used in cases with minimal hypertrophy and moderate ptosis.
The most traditionally proposed techniques would be mastectomy with NAC graft or areolar pedicle flap techniques. Among them, one can choose the superior pedicle, inferior pedicle, or posteroinferior pedicle. NAC grafting is a simple technique, but it has some disadvantages, such as the absence of NAC sensitivity, the chance of non-graft integrity with the risk of pathological scars and even necrosis, and especially the need for dressings and special care in the graft area for at least 10 to 14 PO days. The techniques that use the pedicle have the great advantage of maintaining the vascular nerve bundle; that is, there is the preservation of the tactile sensitivity of the NAC8, repeating that this does not occur in cases of NAC graft.
The Lalonde female breast reduction technique can be applied to treating male breast enlargement in patients at high risk of scarring complications. It offers an alternative to the more widely used concentric skin reduction techniques10. Kazzazi & Malata10 describe this as the first report in the literature on applying the Lalonde surgical technique “without vertical scar” for treating gynecomastia in patients with darkly pigmented skin.
The resulting horizontal scar, used in this study, allows a large resection of redundant and flaccid tissues, as it can extend to the posterior axillary line or the back in cases where it is associated with dorsoplasty, restoring the masculinity of the chest of men with positioning end of the scar in the SFM, in the transition between the thorax and the abdomen, which makes it quite aesthetically acceptable, and also, in a way, disguised next to the SFM.
The study by Resende5 and also by Rocha et al.1 ended with a horizontal scar in the middle of the aesthetic unit of the thorax, a scar that is quite apparent, unlike the one shown in this study. As a positive factor, this study also has the absence of a vertical scar (adapted from traditional reduction mammoplasty techniques) that stigmatizes patients with scars similar to those of women. In our midst, Mansur et al.11 described the extension of the scar to the back, treating the arm, breast, and back concomitantly. As in this study, vertical scars on the breasts are avoided.
The upper part of the thorax, the area close to point “A,” where the NAC will be transposed, must be considerably thinned by removing the fatty tissue in the lamellar layer, leaving the flap very thin with only the areolar layer of fat, thus avoiding form, residual fat in this region.
The lipectomy performed here is performed with electrocautery and scissors. We did not use liposuction as described by Thiénot et al.8, who reported a volume aspirated between 450 and 800ml of fat from each patient. The weight of tissue removed in this study was similar to that of the publication by Thiénot et al., although, in the case of the French study, their flap is larger than the one described here. The inferoposterior flap is larger than the posterior areola flap, based on the “plug flap” described by Daher12 and Carramaschi et al.13 for breast reconstruction based on intercostal perforating vessels. Therefore, since the French flap was larger, one could imagine less tissue removal in the European study.
Concerning complications, this sample showed lower values than those reported in the literature. One case of hematoma (3.7%) had a lower value than that of Varma & Henderson14, which was 6%, Maetz et al.15, 8%, and Colombo-Benkmann et al.16, 11%. The first two studies cited had a sample of 17 and 12 patients14,15, smaller than the one presented here, of 27 patients. On the other hand, Colombo-Benkmann et al.16 conducted a very robust study with 100 patients, a large sample.
The study by Thiénot et al.8 did not have any case of a hematoma; however, it had a casuistry 3 times smaller than the one presented here (27 cases). The authors justify the absence of hematoma by using extensive liposuction before tissue resection, which would preserve the lymphatics and reduce the chance of hematoma and seroma. In this study, 1 case of seroma (3.7%) and 2 cases of hypertrophic scars were observed in the sixth month, which were treated with topical corticosteroid tape 12 hours a day for 4 months, with resolution of the problem.
As previously mentioned, the posterior perforating flap of the fourth intercostal vessel was based on the island flap initially described for breast reconstruction12,13. It is a fixed flap on the chest wall, but with mobility that can easily reach the “A” point. In cases of superolateral quadrantectomies, Daher12 and Carramaschi et al.13 demonstrated its safety and versatility. Comparing its volume with the posteroinferior flap, it is much smaller and does not present the same risks of postoperative ptosis, as described by Thiénot et al.8, since its width is 6 cm, the thickness of the base is 8-10 cm and the thickness retroareolar is 2 to 3 cm.
The flap volume described here is 3 x 3 cm at the base and may extend up to 9 cm in length. It is worth remembering that the inferior pedicle, bordered or not, described by Liacyr Ribeiro in 197315, is similar to the Thiénot flap and had its effectiveness improved with the use of the pectoralis major muscle strap, described by Milton Daniel in 199315, avoiding thus the ptosis of the flap at PO15. That is, this corroborates the concern of Thiénot et al.8 with the possibility of flap ptosis due to its size and weight.
The main limitations of this study are the absence of NAC sensitivity tests, which would demonstrate maintenance of sensory innervation, and preoperative arteriography or intraoperative arterial Doppler that showed the perforating branches of the fourth intercostal artery.
CONCLUSION
Surgical treatment of grade III gynecomastia using the horizontal scar technique, without a vertical scar and with repositioning of the NAC, proved effective, as it allows large and wide tissue resection, with low morbidity and good aesthetic results.
1. Clínica Privada, Curitiba, PR,
Brazil
2. Hospital Universitário Cajuru, Pontifícia
Universidade Católica do Paraná, Curitiba, PR, Brazil
3. Pontifícia Universidade Católica do Paraná,
Escola de Medicina, Curitiba, PR, Brazil
Corresponding author: Lincoln Graça Neto Rua Alferes Angelo Sampaio, 2029, Curitiba, PR, Brazil, Zip Code: 80420-160, E-mail: lgracaneto@hotmail.com


























 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter