

Review Article - Year 2023 - Volume 38 -
The main complications in plastic surgery in post-bariatric patients: An integrative review of the literature
As principais complicações em cirurgias plásticas em pacientes pós-bariátrica: Uma revisão integrativa da literatura
ABSTRACT
Introduction: Post-bariatric surgical interventions have become increasingly frequent, including abdominoplasty, inner thigh plastic surgery, brachioplasty, and mastopexy. However, due to bariatric patients' malabsorptive and restrictive nature, this study aims to present complications arising from aesthetic procedures performed on these patients, exposing the risk factors most associated with sequelae and raising options for a better outcome.
Method: An integrative qualitative literature review was carried out according to the guiding question: "What are the main complications in plastic surgeries performed on bariatric patients?". The search was conducted on the Biblioteca Virtual de Saúde (BVS) and PubMed platforms. The articles included in the study were analyzed using the content method.
Results: In total, 6 articles were included, in which it was observed that the main complications of body contouring surgeries, such as abdominoplasty and brachioplasty, in bariatric patients were mainly wound dehiscence, seromas and hematomas, complications, these, mainly related to the patient's body mass index (BMI), their comorbidities and smoking.
Conclusion: Today, there is a greater demand for post-bariatric reconstructive plastic surgery, especially abdominoplasty. Consequently, there was also an increase in intraoperative complications, notably seroma and wound dehiscence. To alleviate them, the best solution is to work on controlling the patient's preoperative risk factors, such as high BMI and smoking, as well as comorbidities that lead to poor healing.
Keywords: Bariatric surgery; Postoperative complications; Esthetics; Intraoperative complications; Plastic surgery procedures.
RESUMO
Introdução: As intervenções cirúrgicas pós-bariátricas vêm se tornando cada vez mais
frequentes e englobam a abdominoplastia, a cirurgia plástica interna da
coxa, a braquioplastia e a mastopexia. Porém, devido ao caráter disabsortivo
e restritivo do paciente bariátrico, esse estudo tem como objetivo
apresentar as complicações advindas de procedimentos estéticos realizados
nestes pacientes, expondo os fatores de risco mais associados às sequelas e
levantando opções para um melhor desfecho.
Método: Foi realizada uma revisão integrativa da literatura, de caráter qualitativo,
segundo a pergunta norteadora: "Quais as principais complicações em
cirurgias plásticas realizadas em pacientes bariatricados?". A busca foi
realizada nas plataformas Biblioteca Virtual de Saúde (BVS) e PubMed. Os
artigos incluídos no estudo foram analisados pelo método de conteúdo.
Resultados: No total foram incluídos 6 artigos, nos quais observou-se que as principais
complicações de cirurgias de contorno corporal, tais como a abdominoplastia
e a braquioplastia, em pacientes bariatricados foram, principalmente,
deiscência de feridas, seromas e hematomas, complicações, essas,
relacionadas principalmente ao índice de massa corporal (IMC) do paciente,
às suas comorbidades e ao tabagismo.
Conclusão: Percebe-se, hoje, uma maior demanda pelas cirurgias plásticas reparadoras
pós-bariátrica, principalmente pela abdominoplastia. Consequentemente,
houve, também, um aumento no número de complicações intraoperatórias,
destacando-se o seroma e a deiscência de feridas. Para amenizá-las, a melhor
solução é trabalhar no controle de fatores de risco pré-operatórios do
paciente, tais como o IMC elevado e o tabagismo, além de comorbidades que
levam à deficiência de cicatrização.
Palavras-chave: Cirurgia bariátrica; Complicações pós-operatórias; Estética; Complicações intraoperatórias; Procedimentos de cirurgia plástica
INTRODUCTION
Associated with high morbidity and mortality rates, obesity has been consolidating itself as a disease of epidemic proportions responsible for being an independent risk factor in numerous chronic diseases1. With the advent of bariatric surgery, there was a reduction in the incidence of comorbidities such as diabetes mellitus, acute myocardial infarction, stroke, systemic arterial hypertension, and obstructive sleep apnea, among others; however, like any procedure, it is not free from complications2.
Indicated for patients with morbid obesity (body mass index - BMI>40 or BMI> 35+ comorbidities) who failed to respond to behavioral treatment, bariatric surgery has restrictive and/or malabsorptive mechanisms3,4. This procedure results in rapid and intense weight loss, but it is also the cause of sequelae, mostly aesthetic, due to excess tissue predominantly in the arms, breasts, and abdomen. This fact corroborates these patients’ search for aesthetic post-bariatric plastic surgery, recommended for patients with a BMI<35kg/m2, with a weight loss of more than 30kg and stable weight for 6 months to 1 year, in good nutritional conditions5.
The most common post-bariatric procedures are abdominoplasty, inner thigh plastic surgery, brachioplasty, and mastopexy2,5. A meta-analysis showed a 60-87% higher risk of postoperative complications in patients undergoing bariatric surgery than in patients who lost weight through behavioral measures5. The main explanation raised is malnutrition and malabsorption observed in varying degrees resulting from the surgical procedure used, for example, gastric bypass, which can generate a nutritional deficiency of around 50 to 80% since the absorption of the main nutrients occurs in the duodenum and proximal jejunum, interfering with wound healing and increasing the risk of infections6.
OBJECTIVE
Finally, considering the number of surgical interventions performed after bariatric surgery and the importance of these procedures, this study aims to present the most common complications found in post-bariatric patients undergoing aesthetic surgery and critically analyze the results presented in the research. In this way, it will be possible to expose factors that are related to the higher rate of complications and, consequently, raise alternative actions that seek a lower incidence of complications in the postoperative period of this type of surgery and in situations where the complication is ongoing, there is a permanent resolution without consequences resulting from what happened.
METHOD
This is an integrative review of the literature, carried out through the adoption of seven development stages: I) identification of the topic of interest, II) elaboration of the guiding question, III) choice of inclusion and exclusion criteria, IV) determination of the research sample, V) categorization of studies, VI) sample analysis, VII) interpretation and synthesis of results obtained in the studies. The elaboration of the guiding question was based on the steps of the PICo methodology: population; (I) interest and (Co) context. This methodology considered the following items: Population - Post-bariatric surgery patients, Interest - Main complications, and Context - Performing plastic surgeries. The problem taken as a guide was, “What are the main complications in plastic surgeries performed on bariatric patients?”.
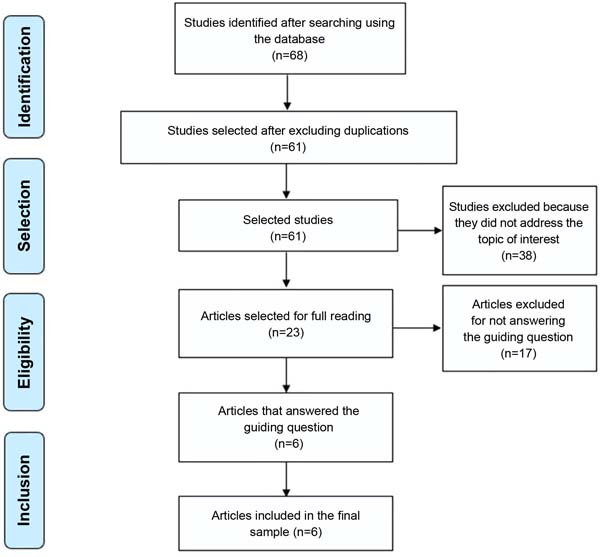
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) recommendation was used to structure and prepare this article. Then, the descriptors were chosen: Complications, Plastic Surgery, and Post bariatric. After defining the descriptors, articles were searched on renowned online platforms such as the Biblioteca Virtual de Saúde (BVS) and PubMed. Firstly, articles were selected by reading abstracts and titles and, later, by reading the complete works.
The selection of articles was conducted in May 2022. The inclusion criteria were original, freely accessible articles published since 2018 in Portuguese and English that answered the guiding question. Reflection articles, editorials, letters, books, case reports, manuals, and other texts that did not specifically address the object of study, paid articles, and duplicate publications were excluded. In each search, Boolean operators were used “AND” to combine the sets of words: Complications AND Plastic Surgery AND Post bariatric. Sixty-eight publications were found, and after applying the exclusion criteria, a sample of 23 articles was obtained: 8 from the MEDLINE database (through the BVS platform), 7 from LILACS (through the BVS platform), 2 from SciELO, and 6 from PubMed Central (PMC). Seventeen articles that did not address the subject of interest or did not answer the study’s guiding question were excluded from the sample. The final sample consisted of six articles (Figure 1).
After obtaining the final sample of articles, a synoptic table was created to organize the information in each publication included in this review. Because this study did not involve research with human beings, approval by the Research Ethics Committee (CEP) was not required.
RESULTS
According to the methodology applied, six articles were selected following the pre-established inclusion criteria. Among the works chosen are publications in English and Portuguese published on the SciELO and PMC platforms. Chart 1 indicates the summary of the articles that make up the sample.
| Title | Authors | Periodical | Summary of conclusions/recommendations |
|---|---|---|---|
| Reducing complicatons in postbariatric plastic surgery: our experience and literature review | Romano et al.5 |
Acta Biomedica: Atenei Parmensis. 2021;90(4):475-81. | The relationship between adverse effects and preoperative BMI was noted. Formerly obese patients are at risk of complications, which encouraged the authors to create a management protocol for these patients. The application of this protocol demonstrated effectiveness in preventing complications. |
| Anthropometric and clinical profiles of post-bariatric patients submitted to procedures in plastic surgery | Rosa et al.2 |
Revista do Colégio Brasileiro de Cirurgiões. 2018;45(2):e1613. | Most operated patients underwent abdominoplasty followed by mammoplasty, rhytidectomy, and brachioplasty. The rate of postoperative complications was approximately 26%. The epidemiological profile of post-bariatric patients who underwent plastic surgery was similar to that reported in the literature, except for the low rate of associated surgeries and postoperative complications. |
| The long-term effect of body contouring procedures on the quality of life in morbidly obese patients after bariatric surgery | Paul et al.7 |
PLoS One. 2021;15(2):e0229138. | Complications
occurred in 5 patients, 1 hematoma, and wound dehiscence in 4
patients. The hematoma required postoperative wound review,
considered a major complication. The remaining patients
with wound dehiscence were classified as minor complications. |
| Comparative analysis on the effect of low-thermal plasma dissection device (PEAK PlasmaBlade) versus conventional electro surgery in post-bariatric body-contouring procedures: A retrospective randomised clinical study | Schlosshauer et al.8 | International Wound Journal. 2019;16(4):932-9. | The PEAK PlasmaBlade appears superior to traditional monopolar electrosurgery for post-bariatric abdominoplasty because it demonstrated significantly less tissue damage, a lower total complication rate, and less postoperative seroma, resulting in faster wound healing. |
| Post-Bariatric Plastic Surgery: Abdominoplasty, the State of the Art in Body Contouring | Sadeghi et al.9 |
Journal of Clinical Medicine. 2022;11(15):4315. | Although abdominoplasty is a safe procedure, it has been associated with a higher complication rate than other body contouring procedures. It is expected that the advancement of knowledge and research in this field will determine the introduction of new technologies and tailored techniques, reducing the rate of complications with rapid reintegration of the patient into the world of work and resumption of daily activities. |
| Cirurgia de contorno corporal pós-bariátrica: análise das complicações em 180 pacientes consecutivos | Cintra Junior et al.3 | Revista do Colégio Brasileiro de Cirurgiões. 2021;48:e20202638. | The increase in bariatric surgeries has provided a greater impact analysis of complications associated with the procedure. Conditions such as BMI and age can be considered as, when combined, they lead to more harmful complications than isolated ones. |
Source: Research data, 2022.
The studies analyzed presented, in general, the complications found in bariatric patients undergoing different body contouring surgeries, including abdominoplasty, brachioplasty, cruroplasty, mastoplasty, lifting in different parts of the body, and rhytidectomy. All studies preferentially presented abdominoplasty as the main surgery performed in post-bariatric patients, which is the procedure with the highest rate of complications. Among the complications cited by the authors, the following stand out: wound dehiscence, seroma, hematoma, tissue necrosis, deep vein thrombosis, pulmonary embolism, umbilical loss, and surgical site infection2,3,5,7-9.
Likewise, the sample analyzed demonstrated that the most common patient complications were seroma and dehiscence. These were mostly correlated to the individual’s BMI, comorbidities, and smoking5,8. In this way, it was possible to identify similar rates of complications in post-bariatric surgery procedures in all studies, without serious complications or death in any population sample studied.
Critically, although the sample of articles presents the main complications found in plastic surgery after massive weight loss, the fact that the studies have relatively small patient samples for a complete analysis of the results obtained within the applied methodology stands out. In this sense, we consider the possible existence of information bias and confounding variables, as there is the possibility of proving new outcomes depending on the time between the procedure and the analysis for the study, given that plastic surgery carries the time factor as an aspect essential when it comes to describing achieved and expected results.
DISCUSSION
Among the options for surgical techniques for performing bariatric surgery, it is possible to mention the gastric band and gastric bypass techniques. The first is an example of an intervention with a dietary restrictive effect, and the second consists of generating a degree of malabsorption through reduction of the stomach and intestinal anastomosis, promoting loss of absorption of nutrients and vitamins10. Therefore, by impairing the absorption of these nutrients by the human body, some functions of the body are impaired, such as healing, collagen synthesis, and epithelialization. Nutrition, therefore, is an extremely crucial factor in preventing postoperative complications11.
According to Zahra et al.11, around 89% of post-bariatric patients desire to undergo some aesthetic intervention to correct sagging skin, causing the performance of these surgeries to increase greatly. Excess skin has been linked to an impact on self-esteem and psychological, sexual, and social well-being, in addition to being responsible for itching, fungal infections, physical discomfort, and restricting physical activity8. In this sense, conducting aesthetic procedures for this population has proven to be a way to regain confidence and satisfaction with their own bodies in these patients8.
Considering the post-bariatric interventions previously mentioned, abdominoplasty was the procedure most performed by individuals2,5,7. Patients had such procedures individually or in combination, and they were performed by most individuals undergoing gastroplasty2. Just like any surgical procedure, plastic surgery can also present adverse effects and, in this context, complications related to external factors stand out, such as smoking, pre-bariatric BMI, infections, large blood loss and longer surgical time, and internal factors, such as problems with healing, nutrient absorption and comorbidities2,8.
Among the risk factors for post-surgical complications, smoking stands out, which increases the risk of adverse events by more than three times, increasing the chance of dehiscence and impairing healing. Other correlations suggested were that in patients who had a BMI <25 preoperatively and in patients who maintained a stable weight for 3 months, the risk of adverse results was lower; however, one of the studies showed that there were no significant correlations between BMI >30 and greater complications3,12. Thus, post-bariatric surgery presents complications of varying degrees, which may require reoperation.
Based on knowledge about the most commonly performed surgical interventions, it is possible to present the most common post-surgical complications found in medical routine, namely: seroma, wound dehiscence, hematoma, surgical site infection, fat necrosis, bleeding, asymmetry, lymphedema, problems involving sensitivity, neuropathy and deep vein thrombosis2,5,7,8,12. Among all these possibilities, the most prevalent adversities were seroma and dehiscence due to healing problems, mostly found in abdominoplasties and combined surgeries13.
Finally, some measures are described in the literature to avoid complications, such as limited dissection towards the intercostal perforators in the case of suture dehiscence and skin necrosis, pre-surgical vitamin supplementation, and the request for a laboratory review, in addition to thromboembolic prophylaxis such as early ambulation and bandaging of the lower limbs14. Other options capable of reducing the chance of postoperative complications in these patients are pre-bariatric weight loss, stopping smoking, and avoiding combined aesthetic surgeries.
CONCLUSION
We conclude that, by demand, abdominoplasty gains emphasis when it comes to post-bariatric plastic procedures and, with it, there is a greater occurrence of seroma formation, as this occupies the first position in the list of main complications after surgery post-bariatric plastic surgery. Therefore, considering the type of approach and the consequences it can bring, it is possible to see that, regardless of the procedure, any complication will have a direct influence on the risk factors presented in the preoperative context, such as smoking, high BMI, healing problems, among other examples. Therefore, for a reduction in complication rates, intervention must be carried out preoperatively, actively acting on factors that trigger intraand post-surgical complications.
On the other hand, this study demonstrated that new analyses of the procedures performed and complications encountered are still necessary, given the inherent time aspect of what is observed as an impact on the result of any aesthetic procedure. Furthermore, there is a lack of studies that demonstrate the impact of risk factors on the results obtained after procedures, as well as a scarcity of analyses that reveal the evolution of complications already witnessed immediately or the appearance of new adverse events dependent on the time.
REFERENCES
1. Nilson EAF, Andrade RCS, Brito DA, Oliveira ML. Custos atribuíveis à obesidade, hipertensão e diabetes no Sistema Único de Saúde, Brasil, 2018. Rev Panam Salud Publica. 2020;44:e32.
2. Rosa SC, Macedo JLS, Casulari LA, Canedo LR, Marques JVA. Anthropometric and clinical profiles of post-bariatric patients submitted to procedures in plastic surgery. Rev Col Bras Cir. 2018;45(2):e1613.
3. Cintra Junior W, Modolin MLA, Colferai DR, Rocha RI, Gemperli R. Cirurgia de contorno corporal pós-bariátrica: análise das complicações em 180 pacientes consecutivos. Rev Col Bras Cir. 2021;48:e20202638.
4. Rosa SC. Perfil antropométrico, comorbidades, fatores preditivos de complicações cirúrgicas e qualidade de vida de pacientes pós-bariátricos submetidos à cirurgia plástica reparadora [Tese de doutorado]. Brasília: Universidade de Brasília, Faculdade de Ciências da Saúde; 2018. 169 p.
5. Romano L, Zoccali G, Orsini G, Giuliani M. Reducing complications in post-bariatric plastic surgery: our experience and literature review. Acta Biomed. 2019;90(4):475-81.
6. Sanches DCB, Pereira AB, Castro GS, Santos SCF, Santos AP, Silva LRB, et al. O aconselhamento nutricional na prevenção das complicações metabólicas em paciente bariátrico. Braz J Health Rev. 2021;4(5):22228-40.
7. Paul MA, Opyrchał J, Knakiewicz M, Jaremków P, Duda-Barcik Ł, Ibrahim MAS, et al. The long-term effect of body contouring procedures on the quality of life in morbidly obese patients after bariatric surgery. PLoS One. 2020;15(2):e0229138.
8. Schlosshauer T, Kiehlmann M, Ramirez P, Riener MO, Djedovic G, Rieger UM. Comparative analysis on the effect of low-thermal plasma dissection device (PEAK PlasmaBlade) versus conventional electro surgery in post-bariatric body-contouring procedures: A retrospective randomised clinical study. Int Wound J. 2019;16(4):932-9.
9. Sadeghi P, Duarte-Bateman D, Ma W, Khalaf R, Fodor R, Pieretti G, et al. Post-Bariatric Plastic Surgery: Abdominoplasty, the State of the Art in Body Contouring. J Clin Med. 2022;11(15):4315. DOI: 10.3390/jcm11154315
10. Lange J, Königsrainer A. Malnutrition as a Complication of Bariatric Surgery - A Clear and Present Danger? Visc Med. 2019;35(5):305-11.
11. Zahra T, Zeina AM, Shebl AM, Khatter AM, Elhadidy MR. Evaluation of the Abdominal Wall Vasculature in Post Bariatric Abdominoplasty: Anatomical and Pathological Study. Egypt J Plast Reconstr Surg. 2020;44(2):245-51.
12. Schlosshauer T, Kiehlmann M, Jung D, Sader R, Rieger UM. Post-Bariatric Abdominoplasty: Analysis of 406 Cases With Focus on Risk Factors and Complications. Aesthet Surg J. 2021;41(1):59-71.
13. Becker JG, Garcia EB, Pedroso JCM, Ferreira LM. Complicações em cirurgias plásticas após perdas ponderais maciças: uma busca sistemática e revisão. Rev Bras Cir Plást. 2019;34(Suppl 2):75-8.
14. Gemperli R, Mendes RRS. Complicações em abdominoplastia. Rev Bras Cir Plást. 2019;34(Suppl 2):53-6.
1. Centro Universitário de Belo Horizonte, Belo
Horizonte, MG, Brazil
2. Universidade de Itaúna, Itaúna, MG,
Brazil
3. Fundação Hospitalar de Minas Gerais, Belo
Horizonte, MG, Brazil
Corresponding author: Elisa Mileni de Sá Gomes Rua Engenheiro Caldas, 348, Bairro Boa Vista, Belo Horizonte, MG, Brazil, Zip Code: 31060-480, E-mail: elisamileni@gmail.com
Article received: June 04, 2022.
Article accepted: March 15, 2023.
Conflicts of interest: none.





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter