

Case Report - Year 2023 - Volume 38 -
Nasal reconstruction using ribs in a patient with Binder syndrome: A case report and literature review
Reconstrução nasal com uso de costela em paciente com síndrome de Binder: Um relato de caso e revisão de literatura
ABSTRACT
Introduction: Binder's syndrome can also be known as maxillonasal dysplasia and it is a congenital malformation characterized by nasomaxillary hypoplasia resulting from an underdevelopment of the middle facial skeleton. The current incidence or prevalence is still unknown, but it affects approximately one child in every 10,000 births. The diagnosis can be clinical or associated with prenatal ultrasonography, characterized by a flattened nose and abnormal maxillary convexity. The treatment is surgical to correct aesthetic and functional abnormalities.
Case Report: Patient diagnosed with Binder's syndrome at the age of 14, without other associated malformations, with aesthetic and functional nasal complaints. Surgical correction began with the extraction of a block of the sixth costal cartilage on the left, with a nasal opening on the columellar margin, in the pattern of an open rhinoplasty, and tissue dissection in the sub-SMAS plane. After preparing the nasal receptor area, a block of cartilage was sculpted for reconstruction of the nasal dorsum, alar grafts and septal cartilage grafts. There was an improvement in the projection of the nasal tip and nasal dorsum.
Conclusion: Rhinoplasty can be a challenging surgery in these patients, and the literature indicates that the best option is autologous reconstruction with costal cartilage. It is necessary to individualize each case to schedule nasal grafts and restructuring, and functional improvement in these cases is also essential.
Keywords: Craniofacial dysostosis; Reconstructive surgical procedures; Nose; Cartilage; Costal cartilage.
RESUMO
Introdução: A síndrome de Binder também pode ser conhecida como displasia maxilonasal e é
uma malformação congênita caracterizada por hipoplasia nasomaxilar devido a
um subdesenvolvimento do esqueleto facial médio. A atual incidência ou
prevalência ainda é desconhecida, mas afeta aproximadamente um recém-nascido
vivo em cada 10.000 nascimentos. O diagnóstico pode ser clínico ou associado
a ultrassonografia pré-natal, caracterizada por nariz achatado e convexidade
anormal da maxila. O tratamento é cirúrgico para correção das anormalidades
estéticas e funcionais.
Relato de Caso: Paciente que recebeu diagnóstico de
síndrome de Binder aos 14 anos, sem outras malformações associadas, com
queixa estética e funcional nasal. A correção cirúrgica foi iniciada pela
extração de um bloco da sexta cartilagem costal à esquerda, com abertura
nasal na margem columelar, no padrão de uma rinoplastia aberta, e dissecados
os tecidos no plano subSMAS. Após preparo da área receptora nasal, foram
esculpidos bloco de cartilagem para reconstrução do dorso nasal, enxertos
alares e enxerto de cartilagem septal. Houve melhora de projeção da ponta
nasal e alongamento nasal.
Conclusão: A rinoplastia pode ser uma cirurgia desafiadora nesses pacientes, sendo a
reconstrução autóloga com o uso de cartilagem costal indicada pela
literatura como a melhor opção. É necessário individualizar cada caso para
programação de enxertos e reestruturação nasal, sendo fundamental também a
melhora funcional desses casos.
Palavras-chave: Disostose craniofacial; Procedimentos cirúrgicos reconstrutivos; Nariz; Cartilagem; Cartilagem costal
INTRODUCTION
Binder syndrome can also be known as maxillonasal dysplasia and is a congenital malformation characterized by nasomaxillary hypoplasia due to underdevelopment of the midfacial skeleton1. In 1962, Binder reported three cases and six features: (1) arrhynoid face; (2) abnormal position of the nasal bones; (3) intermaxillary hypoplasia with consecutive malocclusion; (4) reduced or absent anterior nasal spine; (5) atrophy of the nasal mucosa and (6) absence of the frontal sinus (not mandatory)1,2. The phenotypic appearance is characteristic, with the hypoplastic midface profile, the flat nose, the convex upper lip with a wide philtrum, and the typically crescent or semilunar nostrils giving a half-moon appearance1.
The etiology has not yet been completely defined. However, it is known that it may be associated with multiple etiologies, such as maternal ingestion of coumarin-based anticoagulants during pregnancy, systemic lupus erythematosus, and some other monogenic conditions, such as Keutel syndrome or chondrodysplasia punctata3.
The diagnosis can be made on prenatal ultrasound, characterized by a flat nose and abnormal convexity of the maxilla, and, in addition, there may be abnormal epiphyseal ossification centers, short limbs, and brachytelephalangia3. This article reports the case of a patient with Binder syndrome who underwent surgical treatment for aesthetic and functional nasal improvement.
A female patient, 16 years old, seeks the Plastic Surgery outpatient clinic of the University Hospital, Faculty of Medicine of Botucatu, in Botucatu-SP, wanting to improve the projection of the nasal tip, lengthen the nasal dorsum and respiratory functionality. She states that she has had complaints since childhood but previously sought other doctors who chose not to perform surgical intervention. The patient had no comorbidities or use of continuous medications but reported a diagnosis of Binder syndrome at 14 years of age. He had never had any previous surgery. He also had no family history of any genetic abnormalities. The institution’s Research Ethics Committee approved the work.
On nasal physical examination, it is possible to observe shortening of the nasal dorsum, deviation to the left, small diameter nostrils, inadequately projected and high tip, and hypoplastic middle third of the face, as seen in Figures 1 and 2. On physical examination, absence of firm cartilaginous structures on the dorsum and nasal wings, with complete collapse on palpation, absence of nasal spine anterior to palpation, and absence of any nasal support structure. The patient did not present vertebral or limb anomalies or any other changes. She also had no significant orthodontic changes.
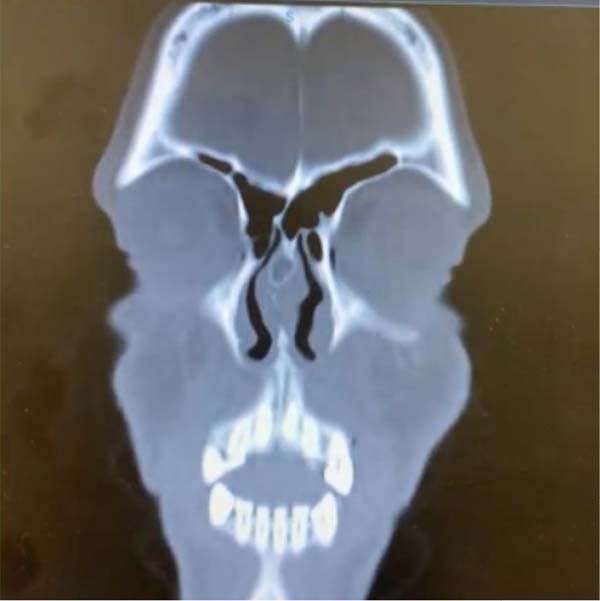
A computed tomography scan of the facial bones was performed, which demonstrated a sinuous deviation of the nasal septum, anterior to the left and posterior to the right, associated with a bone spur to the right and rounded mucous content in the sphenoid sinus to the left, with the absence of the anterior nasal spine, as shown in Figure 3. Maxillary hypoplasia and rounded mucous thickening in the maxillary sinuses were also noted, as shown in Figure 4.
It was proposed to perform nasal reconstruction using costal cartilage grafts, and the procedure’s limitations were explained; however, even after clarification of doubts, the patient chose to undergo the surgery, as she had significant aesthetic and functional discomfort for a long time. The surgical proposal was the reconstruction of the nasal dorsum, wings, and septum.
The surgical correction began with extracting a block of the sixth costal cartilage on the left measuring 5x1.5 cm of extension, respecting gentle manipulation of the tissues to avoid complications, and after removing the material, a tire iron maneuver was performed to exclude the presence of pneumothorax. A nasal opening was made at the columellar margin, in the pattern of open rhinoplasty, and the tissues were dissected in the subSMAS plane.
After preparing the nasal recipient area, a cartilage block was carved to reconstruct the nasal dorsum, alar grafts, and a septal cartilage graft. The graft was fixed cranially to the radix with a titanium screw and caudally to the most anterior portion of the maxilla, considering the presence of an atrophic anterior nasal spine, as seen in Figure 5. A strut-type graft was allocated, and a new domus was created with 5-0 Prolene stitches to improve the projection of the nasal tip. Nasal support can be seen in the intraoperative photo in Figure 6.
The patient was discharged on the first postoperative day, presenting no complications during hospitalization, and attended her first outpatient visit on the sixth postoperative day. The splints and aquaplast were removed, and her nose still showed significant edema. At the consultation after a week, she showed significant improvement in edema and nasal obstruction. The patient has been followed up for three months post-operatively and has had no complications during this period, reporting improved aesthetics and nasal functionality. It was possible to observe nasal lengthening and better projection of the tip, as can be seen in Figures 7 and 8, which indicate the three-month postoperative period.
DISCUSSION
Binder syndrome was initially described in 1962 and can be defined as a congenital malformation characterized by nasomaxillary hypoplasia3. Characteristics of this syndrome include a flat, vertical nose; poor positioning of the nasal bone; intermaxillary hypoplasia with malocclusion; hypoplasia or absence of anterior nasal spine; atrophy of the nasal mucosa; and absence of frontal sinuses2. Similarly, the patient in this report had a short nose, with significant flattening in its dorsal portion, misaligned nasal bone, deviation of the nasal septum, and hypoplasia of the anterior nasal spine.
The current incidence or prevalence is still unknown, but it affects approximately one live newborn in every 10,000 births4. Currently, in addition to physical examination, diagnosis can be performed through prenatal ultrasound, which demonstrates the detection of the Binder phenotype associated with abnormal epiphyseal ossification centers and hypoplasia of the distal phalanges of the hands5. The prenatal diagnosis of the Binder phenotype by ultrasound is based on observing a flat profile in a midsagittal section of the face with a verticalized nasal bone, generally of normal length, and an abnormally increased nasofrontal angle6. Postnatal diagnosis can be made based on usual clinical and radiological findings7.
It can be isolated or associated with multiple etiologies, such as maternal ingestion of coumarin-based anticoagulants during pregnancy, systemic lupus erythematosus, and some other monogenic conditions, such as Keutel syndrome or chondrodysplasia punctata3. In the case of the patient in this case report, there was no medication intake during pregnancy or other conditions already reported. Another important issue is that Binder syndrome may be associated with other malformations, among which vertebral anomalies stand out1. It has been suggested that there is a concomitant induction process common to both the forebrain area and the vertebrae, which would justify the association of these characteristics.
Maxillonasal dysplasia can also be combined with other malformations. The syndrome is associated with true mandibular prognathism in the most severe cases, requiring combined orthodontic and surgical treatment. There may be pseudomandibular or true mandibular prognathism with hypoplastic maxilla1. In the present case, the patient had maxillary hypoplasia with slight mandibular prognathism, but orthognathic surgery was not performed due to the patient’s wishes and her family’s wishes. She wore orthodontic braces during her adolescence for two years, but when she sought care through Plastic Surgery, she was no longer undergoing orthodontic treatment.
Corrective surgery aims to correct the short maxilla with malocclusion, improve perialar flattening, and enlarge the hypoplastic nose8. Planned orthodontic treatment is an integral component of the protocol9. Patients with mild features presenting after completion of facial growth require bone grafting, particularly around the pyriform opening, while those with severe deformities may require orthognathic surgery.10.
The combination of procedures is adapted for each patient. Often, patients also need to undergo secondary surgeries such as refinement procedures, which may include secondary rhinoplasty, genioplasty, and screw removal.11. The treatment schedule in Binder syndrome depends on the progress of facial occlusion symptoms. Surgical treatment may be limited to reconstruction of the nasal dorsum and apex or, additionally, maxillary advancement. Grafting for the osteochondral framework of the nose can be performed from age 14, and osteotomy of the nose or maxilla must be planned after 18.12.
In rhinoseptoplasty, a septoplasty is performed, maintaining an L-strut, and a spreader graft is placed. Lateral osteotomies are initiated with fracture. A caudal septal extension graft is used to allow projection and rotation of the tip13. Domal sutures and an infralobular tip graft create additional tip projection. Finally, alar base and sill excisions are performed to control basilar width and nostril appearance.13.
Different materials have been proposed for surgical treatment to reconstruct the nasal structure, but less evidence concerns which graft may be more stable and appreciated in the nasal contour14.The use of bone and cartilage has been mentioned in the literature according to the surgeon’s needs, between grafts - bone capable of remodeling, but with risk of resorption15. Cartilage has a low infection rate, is easy to shape, and feels natural in situ. However, rib cartilage tends to deform, which alters the configuration of the cartilage graft over time, and graft irregularities may also be visible through the skin15,16.
It was observed that autologous costal cartilage is more favorable for reconstructing the nasal structure and recovering the nasal aesthetics of Binder syndrome14. This was the treatment recommended in the present case, performing resection of the sixth costal cartilage and preparing the grafts before properly positioning them in the nasal structure. Although the use of cartilage grafts surrounded by fascia is an option described in the literature7, it is not yet an established method, and in the present case, we chose to perform a traditional approach using a costal cartilage block to structure the nasal dorsum.
CONCLUSION
Although rare, Binder syndrome results in important changes in the nasal structure, generating aesthetic and functional complaints in patients. Rhinoplasty can be a challenging surgery in these patients, with autologous reconstruction using costal cartilage indicated by the literature as the best option. It is necessary to individualize each case for graft programming and nasal restructuring, and functional improvement in these cases is also essential.
REFERENCES
1. Bhatt YC, Vyas KA, Tandale MS, Panse NS, Bakshi HS, Srivastava RK. Maxillonasal dysplasia (Binder’s syndrome) and its treatment with costal cartilage graft: A follow-up study. Indian J Plast Surg. 2008;41(2):151-9. DOI: https://doi.org/10.4103/0970-0358.44925
2. de Saint Hilaire T, Nguyen DT, Jankowski R, Rumeau C. Is palato-premaxillary subduction a characteristic of Binder’s syndrome? Eur Ann Otorhinolaryngol Head Neck Dis. 2019;136(4):241-5. DOI: https://doi.org/10.1016/j.anorl.2019.03.002
3. Mazzone E, Cos Sanchez T, Persico N, Cannie MM, Jani J. Binder syndrome: a phenotype rather than a definitive diagnosis? Ultrasound Obstet Gynecol. 2019;53(1):131-2. DOI: https://doi.org/10.1002/uog.19198
4. Jawade S, Kantode VV, Wanjari MB, Meghe A, Sharma DR, Wankhede P, et al. A Periodic Case of Maxillo-Nasal Dysplasia or Binder Syndrome Successfully Operated With Bilateral Le Fort II Osteotomy With Distraction Osteogenesis. Cureus. 2022;14(9):e29706.
5. Veduta A, Duta S, Ciobanu AM, Botezatu R, Gica N, Peltecu G, et al. Fetal Skeletal Dysplasias that Involve the Face: Binder Syndrome and Nager Syndrome. Maedica (Bucur). 2021;16(1):140-4.
6. Bosselut H, Panuel M, Sigaudy S, Gorincour G, Chaumoitre K, Bretelle F. The complementary role of imaging modalities in Binder phenotype. Can prognostic factors of neonatal respiratory distress be found? Prenat Diagn. 2019;39(7):549-62. DOI: https://doi.org/10.1002/pd.5469
7. Arroyo HH, Olivetti IP, Santos VGW, Weber R, Jurado JRP. Nasal reconstruction in Binder syndrome. Braz J Otorhinolaryngol. 2017;83(4):488-9. DOI: https://doi.org/10.1016/j.bjorl.2015.08.017
8. Drozdowski PH, Łątkowski I, Zachara MG, Wójcicki P. Binder syndrome: Clinical findings and surgical treatment of 18 patients at the Department of Plastic Surgery in Polanica Zdrój. Adv Clin Exp Med. 2017;26(3):427-37. DOI: https://doi.org/10.17219/acem/62123
9. Cossellu G, Biagi R, Faggioni G, Farronato G. Orthodontic Treatment of Binder Syndrome: A Case Report With 5 Years of Follow-up. Cleft Palate Craniofac J. 2015;52(4):484-8. DOI: https://doi.org/10.1597/14-041
10. Barbera G, Raponi I, Nocini R, Della Monaca M, Priore P, Valentini V. Secondary Rhinoplasty in Binder Syndrome: Considerations and Management of Complex Problem With Heterologous Bone Graft. J Craniofac Surg. 2021;32(1):e5-e8. DOI : https://doi.org/10.1097/SCS.0000000000006789
11. Wang H, Yuan J, Zhang Y, Qi Z, Wei M. Modified nasomaxillary and hard palatine osteotomy combined nasal implantation to correct Binder syndrome. J Craniofac Surg. 2013;24(1):200-3. DOI: https://doi.org/10.1097/SCS.0b013e3182668752
12. Nedev PK. The Binder syndrome: review of the literature and case report. Int J Pediatr Otorhinolaryngol. 2008;72(10):1573-6. DOI: https://doi.org/10.1016/j.ijporl.2008.06.017
13. Veeramani A, Sawh R, Steinbacher DM. Orthognathic Surgery and Rhinoplasty to Address Nasomaxillary Hypoplasia. Plast Reconstr Surg. 2017;140(5):930-2. DOI: https://doi.org/10.1097/PRS.0000000000003789
14. Tian L, You J, Wang H, Zhang B, Xu Y, Lu X, et al. Comparison of Two Different Grafts in Nasal Framework Reconstruction of Binder Syndrome: Cartilage and Silicone. J Craniofac Surg. 2017;28(6):1413-7. DOI: https://doi.org/10.1097/SCS.0000000000003660
15. Dutta PD, Khanna S. Case Report on Binder Syndrome. Acta Scientific Otolaryngology. 2021;3(8):125-8. DOI: https://doi.org/10.31080/asol.2021.03.0312
16. Çerçi Özkan A, Kozanoğlu E. The utilization of diced cartilage-fascia (DC-F) graft in the augmentation rhinoplasty of a case with Binder syndrome. Eur J Plast Surg. 2021;44:393-8. DOI: https://doi.org/10.1007/s00238-020-01714-z
1. Universidade Estadual Paulista, Botucatu, SP,
Brazil
Corresponding author: Oona Tomiê Daronch Rua Prof. Dr. Mauro Rodrigues de Oliveira S/N, Botucatu, SP, Brazil, Zip Code: 18618-688, E-mail: oona.daronch@yahoo.com.br
Article received: February 01, 2023.
Article accepted: August 20, 2023.
Conflicts of interest: none.


















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter