

Review Article - Year 2023 - Volume 38 -
Treatment of keloids and hypertrophic scars: A descriptive review
Tratamento de queloides e cicatrizes hipertróficas: Uma revisão descritiva
ABSTRACT
Keloids and hypertrophic scars are lesions formed from the abnormal fibroproliferative response to the wound healing process, generating excessive collagen proliferation in the lesions. They generally predominate in female patients and individuals with darker skin tones. The therapeutic approach to these scars can be indicated according to criteria such as functional deficit, size, and wound healing time. In this sense, the present study aimed to conduct a descriptive review of the literature, seeking evidence of treatment over the last five years. The review was carried out based on the PRISMA guideline, using the databases PubMed, LILACS, Cochrane Library, SCOPUS, Web of Science, and Grey Literature between 2018 and 2022. Seven hundred forty articles were found, of which 16 randomized clinical trials were selected. It was demonstrated that keloid management presents a multimodal approach, with no gold standard of treatment with a low recurrence rate. Furthermore, combined therapy with different agents appeared superior to the isolated therapeutic methods in treating these injuries.
Keywords: Keloid; Cicatrix, hypertrophic; Therapeutics; Plastic surgery procedures; Review.
RESUMO
Queloides e cicatrizes hipertróficas são lesões formadas a partir da resposta
fibroproliferativa anormal ao processo de cicatrização de feridas, gerando uma
proliferação excessiva do colágeno nas lesões. Geralmente, predominam em
pacientes do sexo feminino e em indivíduos com tons de pele mais escuros. A
abordagem terapêutica dessas cicatrizes pode ser indicada de acordo com alguns
critérios, como déficit funcional, tamanho e tempo de cicatrização da ferida. Nesse
sentido, o presente estudo objetivou realizar uma revisão descritiva da literatura,
buscando as evidências de tratamento dos últimos cinco anos neste tema. A revisão
foi realizada com base no guideline PRISMA, utilizando as bases de dados PubMed,
LILACS, Cochrane Library, SCOPUS, Web of Science e Grey Literature, entre os
anos de 2018 e 2022. Foram encontrados 740 artigos, dos quais 16 ensaios clínicos
randomizados foram selecionados. Foi evidenciado que manejo do queloide apresenta
abordagem multimodal, não havendo um padrão-ouro de tratamento, com taxa de
recorrência baixa. Além disso, a terapia combinada de diferentes agentes pareceu
ser superior ao uso isolado de métodos terapêuticos no tratamento dessas lesões.
Palavras-chave: Queloide; Cicatriz hipertrófica; Terapêutica; Procedimentos de cirurgia plástica; Revisão
INTRODUCTION
Keloids and hypertrophic scars are formed from the excessive proliferation of collagen in lesions, which accidents, insect bites, burns, vaccinations, use of piercing jewelry, acne and infections, with an exaggerated recruitment of fibroblasts and excessive deposition of extracellular matrix1 can cause. Such injuries predominate in females, as estrogen is associated with more serious conditions, and tend to be located in joints and body folds due to the constant distension of these locations during daily body movements2.
Regarding its epidemiology, it can be stated that these lesions are more frequent in darker skin tones. Hochman et al.3 indicated Fitzpatrick phototype III as the most common among patients with fibroproliferative scars. Furthermore, in people aged 25 years or older, the majority of injuries are traumatic in origin4. It is also known that Caucasians are less susceptible to developing keloids and hypertrophic scars when compared to African Americans, suggesting that genetic mechanisms may be involved in the pathogenesis of these lesions5,6.
Although it is known that both constitute an abnormal fibroproliferative response to the healing process, it is possible to highlight some differences between them. The keloid invades beyond the original edges of the wound and does not regress after its formation. The hypertrophic scar, in turn, respects the previous limits of the injury, forms and regresses in a shorter time, and is associated with subsequent wound contracture7,8.
The formation process of pathological scars is not fully understood, and some studies suggest the participation of cells such as fibroblasts, myofibroblasts, mast cells, and other cytokines such as tumor necrosis factor α and TGF-β29,10. The abnormal growth of these scars is enhanced by chronic inflammation in the reticular dermis, and, generally, the hypertrophic scar presents a loss of this dermal inflammation, and the keloid develops long-lasting inflammation11. Such inflammation is a triggering factor for a cascade of interleukins that are deeply involved in the mechanism of development of these wounds, which can be the target of specific treatments12.
Therefore, the basis of treatment is based on the pathogenesis of hypertrophic scars and keloids, and different approaches can be used, such as surgery, cryotherapy, radiotherapy, intralesional injection (which can be done with corticosteroids, 5-fluorouracil, and verapamil) and laser therapy13. There is also a subdivision into non-invasive therapies, such as pressure garments, physiotherapy, silicone plates, and onion extract14.
Different approaches can be indicated according to some criteria, such as wound healing time, functional deficit, size, presence and amount of adjacent tissue, and presence of vascularized muscle or fascia beneath the tissue15. Treating these injuries, in addition to the aesthetic issue, can improve the patient’s quality of life, as such scars are associated with pain, hyperesthesia, and itching, especially when it comes to keloids16.
OBJECTIVE
In this scenario, the objective was to conduct a descriptive review of the literature seeking evidence from the last five years in treating keloids and hypertrophic scars, carefully analyzing the data found in different databases regarding the approach to these pathologies.
METHOD
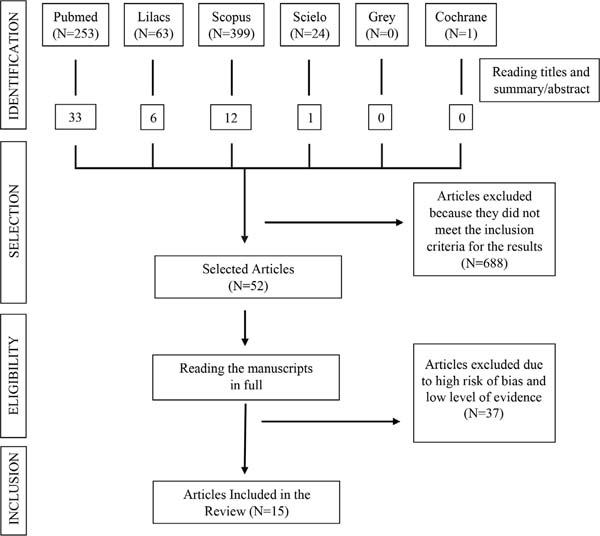
This is a descriptive literature review based on the search for accessible studies, using the PRISMA17 guideline, adopting the following strategy:
1) Preparation of a research question guiding the search strategy; 2) Variety of sources for locating studies; 3) Definition of inclusion and exclusion criteria; and 4) Assessment of the methodological quality of the included articles.
The survey of articles was carried out in February 2022, using the databases PubMed (US National Library of Medicine/National Institute of Health), LILACS (Latin American and Caribbean Center for Health Sciences Information), Cochrane Library, SCOPUS, Web of Science and Grey Literature, published between 2018 and 2022. The PICO strategy was used, which represents an acronym for Patient, Intervention, Comparison, and “Outcomes” (outcome), and the following question was created advisor: “What is the evidence for treatment for keloids and hypertrophic scars?”
The descriptors related to the themes investigated were crossed after searching for synonyms using the tools MeSH (Medical Subject Headings) and DeCS (Descriptors in Health Sciences); therefore, the descriptors were defined: (“Cicatrix, Hypertrophic” OR “Cicatrices, Hypertrophic” OR “Hypertrophic Cicatrices” OR “Hypertrophic Cicatrix” OR “Scars, Hypertrophic” OR “Hypertrophic Scar” OR “Hypertrophic Scars” OR “Scar, Hypertrophic” OR “Keloid” OR “Keloids”) AND (“Therapeutics” OR “Therapeutic” OR “Therapy” OR “Therapies” OR “Treatment” OR “Treatments”).
At this point in the search, broader terms were intentionally used to identify more productions, preventing any important studies from being excluded from the survey. After this, the title and abstract were analyzed to select studies that evaluated the population and intervention of interest. Case reports, case series, cross-sectional studies, and cohorts were removed as they presented low evidence. In addition, duplicate articles and studies not written in English, Spanish, or Portuguese were excluded.
Therefore, concerning eligibility, the articles were read in full, and studies with a high risk of methodological bias were excluded, using the Risk Of Bias 2 (RoB 2) tool, a revised tool to assess the risk of bias in randomized studies (Table 1); articles classified as literature reviews were not included in the results; however, they were used in the discussion. The outcomes defined for this research were the effectiveness of isolated and combined treatments for keloids and hypertrophic scars.
| Author/Year | D1 | D2 | D3 | D4 | D5 | Final | ||
|---|---|---|---|---|---|---|---|---|
| Hietanen et al., 2019 | + | + | + | + | ! | + | + | Low risk |
| Hietanen et al., 2020 | + | + | + | + | + | + | ! | Some Risk |
| Khalid et al., 2019 | + | + | + | ! | + | + | - | High risk |
| Abedini et al., 2018 | + | + | + | + | + | + | ||
| Kim et al., 2020 | + | ! | + | + | + | ! | D1 | Randomization process |
| Aggarwal et al., 2018 | + | + | + | + | + | + | D2 | Deviations from intended interventions |
| Neinaa et al., 2021 | + | + | + | ! | + | + | D3 | Missing result data |
| Hewedy et al., 2022 | + | + | + | + | + | + | D4 | Measuring results |
| Rasaii et al., 2019 | + | + | + | + | + | + | D5 | Selection of results |
| Khalid et al., 2018 | + | + | + | ! | + | + | ||
| Tawfic et al., 2020 | + | + | + | + | + | + | ||
| Ismail et al., 2021 | + | + | + | + | + | + | ||
| Hedayatyanfard et al., 2018 | + | ! | + | + | + | ! | ||
| Babu et al., 2019 | + | + | + | + | + | + | ||
| Güngör et al., 2020 | + | + | + | ! | + | ! |
The tools that showed the effectiveness levels of treatments were the Vancouver Scar Scale (VSS), Visual Analog Scale (VAS), Verbal Assessment Scale (VRS), and Patient and Observer Scar Assessment Scale (POSAS) with assessment of the patient and the responsible professional; in some studies, histopathological analyzes were carried out on preand post-treatment microstructural changes.
RESULTS
Types of study
Seven hundred forty articles were found in the searched databases, of which 15 were selected, with their interpretation and synthesis. All 15 studies were randomized controlled trials (Figure 1).
Furthermore, regarding the treatment modalities of the studies included in the review, there are surgical options with clinical adjuvant:
Intralesional injectable modalities:
• Triamcinolone Acetonide (TAC);
• 5-Fluorouracil (5-FU);
• Verapamil;
• Hyaluronidase;
• Botulinum Toxin Type A (BTX-A);
• Platelet Rich Plasma (PRP).
Scar coverage options:
TAC vs. 5-FU
The study by Hietanen et al.18 on 50 keloids, treated in 2 equal groups, randomly divided, with intralesional injections at 3-week intervals, indicated that treatment efficacy did not differ significantly between the groups treated with TAC and 5-FU. An experienced plastic surgeon clinically defined keloid remission as flattening the lesion to the point where no further treatment or injections were indicated, and the remission rate was 46% in the 5-FU group and 60% in the TAC group at 6 months of follow-up. In addition to this analysis concerning the POSAS index, both therapies positively evaluated the patient and the surgeon.
On another occasion, the same group of researchers analyzed the histopathological response to this treatment19. The most biologically relevant difference was in baseline myofibroblast values: the response group had more myofibroblasts at baseline than non-responders, but the difference was not statistically significant. However, it was indicated that the loss of myofibroblasts occurs in the group of keloids that respond to injection therapies but not in the keloids that do not respond, denoting that the response to therapy is, in fact, associated with the reduction of myofibroblasts in these lesions.
In addition, the study by Khalid et al.20 compared the TAC groups (group A=51) with TAC + 5-FU (group B=75) in keloids and hypertrophic scars, with one injection weekly for 8 weeks. The outcomes were evaluated at 4, 8, and 12 weeks regarding the average reduction in scar height and lesion recurrence, with a 50% reduction in lesion height as a reference for success.
Of the 108 patients who completed the study, both treatment modalities were effective; however, the average reduction in scar height in group B (5-FU + TAC) was markedly better than in group A (TAC), with a lower recurrence rate at 22-month follow-up. Furthermore, individualizing the analysis concerning keloids, group B showed 78% treatment efficacy, a statistically significant result superior to group A; The results related to hypertrophic scar did not demonstrate a statistically significant difference between the two groups20.
TAC vs. verapamil
In 50 patients conducted in the study by Abedini et al.21, 21 with two or more lesions (keloids and/or hypertrophic scars), treated with intralesional injections of TAC or verapamil, with applications every 3 weeks on up to 6 occasions, aimed -compare therapy using the VSS (Vancouver Scar Scale), a clinical analysis concerning vascularization, pigmentation and recurrence of lesions for up to 1 year. There was a significant difference between therapies; the findings revealed that verapamil was ineffective in reducing VSS parameters (height, pigmentation, flexibility, and vascularity). In lesions treated with TAC, the effectiveness of the therapy was observed in all VSS parameters from week 3 onwards, and the average time of decrease in height and flexibility parameters was 15 weeks, indicating that verapamil cannot be considered an alternative adequate and effective treatment to the detriment of TAC, which has a faster therapeutic response with fewer side effects.
TAC vs. ESWT
The study by Kim et al.22 compared intralesional TAC injections with Extracorporeal ShockWave Therapy (ESWT) in 40 patients with keloids, who were allocated into two groups. One group received isolated intralesional injection of TAC, and the other, TAC+ESWT. After 12 weeks of starting treatment, it was evident that both groups showed acceptable improvements in most of the dimensions assessed. However, such improvements were statistically more significant in the second group, presenting a greater average percentage reduction in the lesion’s length, width, and height and a better VSS score than the first (p<0.05). Furthermore, in the Patient and Investigator Global Assessment, more scores ≥4 were evidenced, indicating good or excellent grades, in the TAC+ESWT group, without serious adverse events occurring, suggesting that ESWT may be a new form of adjuvant treatment in keloids.
TAC vs. TAC + hyaluronidase vs. verapamil vs. radio frequency vs. CT + radiofrequency
In this study carried out by Aggarwal et al.23, 80 patients with keloids completed the study and were allocated into five therapeutic groups, treated with 1-TAC alone; 2-Hyaluronidase associated with TAC; 3-Verapamil; 4- Radiofrequency and 5-TAC combined with radiofrequency. The result of the treatment was evaluated using the VSS scale. In this scenario, it was evident that the first, second, and fifth groups obtained similar results regarding scar removal, in which the clearance rate was 75%, 69%, and 75% effective treatments for keloids. Therefore, the study suggests that TAC, TAC with hyaluronidase, and radiofrequency with TAC are equally effective and that verapamil and radiofrequency alone are not good therapeutic methods for keloids.
TAC vs. BTX-A vs. PRP
Furthermore, the research carried out by Neinaa et al.24, involving 60 patients with keloids, compared 3 isolated intralesional injection therapies: Group I: Botulinum Toxin Type A (BTX-A); Group II: Platelet Rich Plasma (PRP) and Group III: TAC. This randomized clinical trial evaluated scars, VSS, and VRS before and after treatment without specifying an exact period. A significant improvement was seen, as well as lower expression of the pro-fibrotic gene CTGF by immunohistochemistry in groups I and II, compared to III. There was no significant difference between groups I and II. Therefore, the study concluded that intralesional injection of BTX-A and PRP generated better outcomes in keloid treatments when compared to injection with TAC.
TAC vs. CT + PRP
In another study25, the therapeutic modalities compared were TAC alone or combined with PRP. A randomized clinical trial was carried out with 40 patients randomly distributed into two equal groups (A and B). Both received intralesional TAC 20 mg/ml for 4 sessions, 3 weeks apart. Group A patients received additional intralesional PRP 1 week after TAC injections. After 3 months of follow-up, both groups showed significant improvement in the parameters of the VSS and VRS scales. Furthermore, group A significantly improved height, pigmentation, flexibility, and general VSS, while group B evolved with a significant incidence of post-TAC atrophy and hypopigmentation.
TAC vs. TAC + BTX-A
In turn, Rasaii et al.26 compared intralesional injection of TAC with BTX-A in a double-masked randomized clinical trial. Twenty-three patients with at least 2 keloids were allocated into 2 groups, with participants in group A receiving only TAC and those in group B, TAC associated with BTX-A. Each keloid underwent the designated therapy every four weeks for three sessions, evaluating the symptoms of pain and itching, using the visual analog scale, the height of the scars using calipers, and scoring them on the VSS. Both modalities generated a decrease in height, vascularity, and flexibility scores, with no significant difference between them. However, group B significantly reduced pain and itching compared to A. Therefore, bimodal therapy indicated greater efficacy in the adjuvant setting.
Surgical excision + TAC + 5-FU vs. surgical excision + radiation
Khalid et al.27 carried out a randomized clinical trial with 60 patients with ear keloids, who were randomly allocated into 2 groups. Group A received treatment with surgical excision and intralesional injection of TAC + 5-FU. Group B, in turn, was treated with surgical excision and radiotherapy. Efficacy in group A was 73.33%, and 43.33% in group B (p=0.01), showing a statistically significant difference between therapeutic modalities at a 6-month follow-up. Therefore, it was concluded that excision associated with TAC + 5-FU injection is an effective modality for treating keloids.
Fractional CO2 laser vs. ND-YAG laser vs. both
A study28 compared Nd-YAG and fractionated CO2 lasers with each other and combined therapy 2 modalities on clinical, histopathological, and biochemical bases. Thirty patients with at least 3 pathological scars (keloids or hypertrophic scars) participated in the study, each scar from the same patient being assigned to different treatment modalities. Participants underwent 4 sessions, with intervals of 4-6 weeks between them, and the assessment was carried out using the VSS and the Observer Scar Assessment Scale (POSAS). Histopathology quantitatively evaluated the presence of collagen and elastic fibers and biochemistry, the levels of transforming growth factor β I (TGF-β I) and TGF-β III through immunoenzymatic assay studies. As an outcome, hypertrophic scars improved more clearly with fractionated CO2, with keloids showing no significant difference between therapies. Collagen fibers substantially improved appearance and pattern, and TGF-β I levels were considerably reduced, while TGF-β III levels showed an insignificant increase in all treatment modalities. The therapeutic combination in the same session did not show substantial additional benefit and presented a greater side effect profile.
Intralesional botulinum toxin A (IL BTX-A) vs. 5-FU
In this study29, a clinical comparison was proposed between intralesional botulinum toxin A (IL BTX-A) and IL 5-fluorouracil (IL 5-FU) in treating keloids in 50 patients. Twenty-two patients (with 26 keloids) were treated with IL BTX-A monthly for up to 6 months, and another 22 patients (with 27 keloids) were treated with IL 5-FU weekly for up to 6 weeks; the remaining 6 patients, each with multiple keloids, were treated with IL BTX-A for some lesions (8 keloids) and IL 5-FU for their remaining lesions (8 keloids), the main outcome for clinical improvement was flattening of the lesions. A significantly better therapeutic response of keloids was detected after IL BTX-A than IL 5-FU (p=0.041). IL BTX-A achieved excellent and good flattening of lesions (58.8% and 20.6%) compared to (31.4% and 17.1%) after IL 5-FU. Therefore, IL BTX-A proved to be more effective, especially for large keloids, with fewer side effects than IL 5-FU, less pain, itching, and no hyperpigmentation.
Losartan ointment
Hedayatyanfard et al.30 carried out a study to examine losartan ointment’s clinical effects in reducing hypertrophic scarring and keloids. A randomized, single-masked clinical trial was carried out with 37 patients who received 5% losartan or placebo for the treatment of keloids and hypertrophic scars. Of these, 30 patients completed the study, 20 receiving losartan and 10 placebo, being evaluated for 6 months according to the VSS regarding the criteria vascularity, flexibility, pigmentation and height, and pain and itching in scar tissue. In both hypertrophic scars and keloids, VSS scores were significantly reduced in the stipulated treatment (p<0.01) and relief of pain and itching. No recurrence of scars was observed 6 months after using losartan.
Intense pulsatile light (LIP) vs. silicone gel sheet
In a clinical trial31, 28 patients with 65 hypertrophic scars participated. Each scar was divided into 2 equal parts. Half of the scar was treated with 4 sessions of 29J/cm2 of LIP at 3 weekly intervals. A silicone gel (SGS) sheet was applied to the other half and changed at 3-week intervals. The Vancouver Scar Scale was used to grade both halves of the scar before treatment, at each visit, and 3 weeks after completion of treatment. The results showed that scars treated with LIP significantly reduced flexibility (p=0.002) and hyperpigmentation (p=0.0001) compared to scars treated with SGS. Although the percentage reduction in scar height was greater in the IPL group (15.4% compared to 4.6% in the SGS group), the result was not statistically significant (p<0.065).
Onion Extract
A 202032 study evaluated the effectiveness of Allium cepa L onion extract, allantoin, and heparin combined in a topical gel in reducing scars after the second cesarean section in 120 women who had hypertrophic scars after the first cesarean section. The groups using gel and the control group were divided into equal numbers, with topical healing gel postoperatively applied for 6 months, and the outcome was evaluated according to the VSS. Therefore, significant reductions were observed in the vascularity, pigmentation, and VSS height subgroups for those who continued treatment for 24 weeks.
DISCUSSION
The scar development process is complex and requires understanding the molecular mechanisms that cause its development and recurrences. Multimodal therapies showed better aesthetic and functional results when correctly indicated.
It can be stated that the decision for therapies used to aesthetically and functionally improve pathological scars must be individualized, considering the peculiarities of each case. To facilitate decision-making, there is an attempt to create algorithms, such as APAS, which systematize the choices for different therapeutic methods, combining them when necessary. This divides the treatment into the first assessment, softening of scars; approach with technologies and injections; and treat pigmentation and skin quality33,34.
In the present study, the most frequently discussed clinical therapy was intralesional injection, performed with TAC or 5-FU alone or combined with other measures. In general, combined therapies obtained more significant results concerning aesthetic and symptomatic aspects than isolated measures, which aligns with the study of a large literature review from 202135.
Regarding surgical therapies for pathological scar excision, several previous studies indicate that isolated excision does not generate good results, with a recurrence rate greater than 50%36. For this reason, in this review, studies that combined surgical excision with clinical intralesional injection therapies demonstrated positive results, reiterating meta-analyses on the topic. In another meta-analysis that examined the use of TAC after excision of ear keloids, the recurrence rate was 15.4% (95% CI, 9.4 to 24.1%; p<0.001), proving to have similar efficacy to radiotherapy after excision37,38.
Regarding therapy mediated by fractional CO2 laser, it can be seen in this study that it was superior to other laser modalities. Correlating with the literature, it is known that this laser is associated with improving clinical signs and symptoms of pathological scars, such as color, thickness, and itching of the lesions. It also acts on the pathophysiology of these injuries, interfering with the orientation of collagen fibers, promoting results in the flexibility and height of scars39. Furthermore, laser therapy had fewer side effects and better aesthetic outcomes when associated with intralesional triamcinolone40.
Some limitations must be considered. We can observe different outcome assessment scales: clinical analyses, topographics, and opinions of the patient and the responsible doctor, among others. Therefore, studies evaluate results in a heterogeneous way. Therefore, according to the analyzed methodologies, there are different follow-up methods in the studies, considering counting the outcome with different temporalities. Furthermore, a meta-analysis could not be conducted due to heterogeneity among studies to meet all interest criteria. It is worth noting that more research is needed to identify additional biochemical, histological, and genetic mechanisms that drive the development and recurrence of keloid and hypertrophic scarring.
CONCLUSION
The management of keloids and hypertrophic scars continues to be approached in a multimodal way, without there being a gold standard of treatment that provides symptomatic and aesthetic reduction and with consistently low recurrence rates. However, today, combined clinical and surgical treatments, such as intralesional injections of 5-fluorouracil or triamcinolone, radiotherapy, and excision of the lesion, are more effective than isolated therapies. Therefore, further studies in this field are needed to standardize the treatment of these injuries, aiming for better patient outcomes.
1. Universidade do Estado do Pará, Cirurgia
Plástica, Belém, Pará, Brazil
Corresponding author: Vinicius Fialho Teixeira Tv. Perebebuí, 2623, Marco, Belém, PA, Brazil., Zip code: 66087-662, E-mail: viniciusfialhoteixeira@gmail.com




 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter