

Original Article - Year 2023 - Volume 38 -
Risk factors resulting from complications in the postoperative period of primary breast augmentation with silicone implants: Retrospective study
Fatores de risco consequentes a complicações no pós-operatório da mastoplastia de aumento primária com implantes de silicone: Estudo retrospectivo
ABSTRACT
Introduction: Breast augmentation is one of the most performed plastic surgeries in the world. Given its high applicability, it is essential to know the risk factors related to the incidence of postoperative complications to reduce them in this type of procedure.
Method: This retrospective study analyzed the medical records of 76 patients who underwent primary breast augmentation with silicone implants from January 2018 to December 2020.
Results: It was observed that the presence of comorbidities increased the incidence of early postoperative complications (p<0.001) but not of late postoperative complications (p=0.8). Longer surgical time also increased the incidence of postoperative complications (p=0.005).
Conclusion: The presence of comorbidities directly influences the incidence of postoperative complications after breast augmentation, and for this reason, adequate preoperative compensation must be carried out before submitting patients to this surgical procedure.
Keywords: Mammaplasty; Breast implants. Postoperative complications; Implant capsular contracture; Silicones.
RESUMO
Introdução: A mamoplastia de aumento é uma das cirurgias plásticas mais realizadas no
mundo. Tendo em vista sua alta aplicabilidade, é fundamental conhecer os
fatores de risco relacionados à incidência de complicações pós-operatórias a
fim de reduzi-las nesse tipo de procedimento.
Método: Este estudo é retrospectivo feito por meio da análise dos prontuários de 76
pacientes que realizaram mamoplastia de aumento primária com implantes de
silicone durante os meses de janeiro de 2018 a dezembro de 2020.
Resultados: Observou-se que a presença de comorbidades aumentou a incidência de
complicações pós-operatórias precoces (p<0,001), mas não
de complicações pós-operatórias tardias (p=0,8). O maior
tempo cirúrgico também aumentou a incidência de complicações pós-operatórias
(p=0,005).
Conclusão: A presença de comorbidades influencia diretamente na incidência de
complicações pós-operatórias da mastoplastia de aumento e por esta razão
deve-se realizar uma adequada compensação pré-operatória antes de submeter
as pacientes a este procedimento cirúrgico.
Palavras-chave: Mamoplastia; Implantes de mama; Complicações pós-operatórias; Contratura capsular em implantes; Silicones
INTRODUCTION
Breast augmentation with implants is the most commonly performed surgery in the world, with 1,621,281 surgeries performed in total in 2020, and of these, 173,420 were performed in Brazil, representing 25% of all aesthetic plastic surgeries performed in the country1. In 2020, Brazil was the second country that performed the most aesthetic plastic surgeries worldwide, behind only the United States, where 371,997 breast augmentation procedures were performed1. Therefore, breast augmentation remains one of the most common aesthetic procedures performed globally.
In the United States, both silicone gel-filled and saline-filled implants are used. On the other hand, in Europe, the vast majority of implants used are silicone because they are generally considered superior in terms of feel and durability2. The most common practices in Brazil included round microtexture implants and polyurethane-coated silicone in the primary procedure3.
Changes in the gel filling of modern implants have led to the development of form-stable gels that are highly cohesive. Even with changes in the composition of implants and the emergence of new technologies, breast augmentation is not surgery-free from complications. The main ones are capsular contracture, seroma, breast ptosis, and infection related to the implant surface4. It is known that a presumed increased risk in the development of capsular contracture is shown for the following variables: longer duration of follow-up, breast reconstructive surgery in patients with a history of breast cancer, subglandular implant placement, postoperative hematoma and textured surface of the implant5.
Despite the relatively low number of complications, the absolute number due to the high number of cases represents an important issue that every plastic surgeon has to face regularly. In addition to complications, there are other factors related to the rate of reoperations, with the biggest complaint being the loss of projection in the upper pole and bulging of the lower pole6. Therefore, it is essential to know the risk factors involved in developing early and late postoperative complications in primary breast augmentation to intervene in modifiable risk factors and positively alter the long-term outcome of these patients.
OBJECTIVE
The objectives of the present study were to carry out an epidemiological assessment of patients undergoing primary breast augmentation and to verify the main factors related to the incidence of complications in the early and late postoperative period.
METHOD
This retrospective study analyzes medical records of patients who underwent primary breast augmentation with silicone implants between January 2018 and December 2020. All patients registered in the surgical center with the procedure called “Augmentation mammoplasty” registered by Plastic Surgery in the surgical center of the Hospital de Clínicas of the Faculdade de Medicina de Botucatu (UNESP, São Paulo, Brazil) during the mentioned period. Chief plastic surgery preceptors assist resident surgeons.
The inclusion criteria were patients who underwent primary breast augmentation during the period studied, excluding patients who underwent mastopexy with implants, secondary breast augmentation, concomitant surgeries at the same surgical time, and patients who presented incomplete data in the medical record for the adequate study of the data.
The standard of the service is to operate on patients who are at the appropriate weight (preferably BMI<25 kg/m2). Furthermore, patients who smoke are not operated on and are advised to stop smoking at least 12 weeks before and 12 weeks after the procedure. The standard in patients undergoing primary breast augmentation is not to place drains postoperatively. All implants placed were used from the same commercial brand. We do not present any conflicts of interest for the brand used in the service, nor do we receive financial or scientific support from it.
The quantitative variables studied were age, length of stay, surgery time, and breast implant volume. The qualitative variables were Fitzpatrick skin type, presence of comorbidities, use of continuous medications, type of access for placing the breast implant, location of the implant (subfascial, subglandular or retromuscular), type of access (periareolar or inframammary), surface the prosthesis used (smooth, textured or polyurethane), presence of complications in the early and late postoperative period.
The patients in the present study were followed for a minimum period of 18 months, with the first follow-up being carried out three days postoperatively, the second in one week, the third in 1 month, and after 3, 6, and 12 months of surgery, traditionally. Patients who presented complications were followed up at shorter intervals, respecting the needs of each condition. Early postoperative complications were considered to occur up to 30 days postoperatively, and late postoperative complications after this period.
Of the patients included, the medical records were reviewed, and the studied data was entered into Google Docs forms. Statistical analyses were conducted using the SPSS 20.0 program from the generated Excel spreadsheet. As for statistical analysis, the variables were studied and presented in their mean values and standard deviation or frequencies. The Kolmogorov-Smirnov test was used to study the normality of quantitative variables, and as they presented a normal distribution, the Student’s t-test was applied for independent samples. The Chi-square or Fisher’s Exact test was used for qualitative variables to study their association. To study the correlation between variables, Pearson’s correlation coefficient was used. Values of p<0.05 were considered statistically significant.
RESULTS
During the study period, 76 patients underwent primary breast augmentation. Only 20% of these surgeries were performed between March and December 2020 during the pandemic due to COVID-19. The mean age of the patients was 30.3 years, with a standard deviation of 8.1 years. The patients’ average BMI was 22.2kg/m2. The majority of patients did not have any comorbidity (82.14%), and of the patients who had comorbidities, the most common was the presence of hypothyroidism (5.36%), followed by anxiety (2.68%).
Of the 76 patients who underwent primary breast augmentation, the average surgery time was 80 minutes, and all patients were discharged on the first postoperative day. Early postoperative complications occurred in 5 patients (6.57%); in all cases, the complication was surgical wound dehiscence. Late postoperative complications occurred in 4 patients (5.26%), two asymmetry cases, one hypertrophic scar, and one grade I capsular contracture.
All patients received round breast implants except for one in whom an anatomical shape was placed due to her preference. The average volume of the implants was 332.5 grams in the right breast and 335 grams in the left breast. Only two patients underwent placement of different breast volumes between one breast and the other, both with significant breast asymmetry, in the first a difference of 50 grams between both breasts and in the second a difference of 45 grams. Both showed improvement in postoperative breast asymmetry.
It was observed that the presence of comorbidities increased the incidence of early postoperative complications. Of the patients who did not present comorbidities, only 8.7% had early complications, and of those who presented at least some comorbidity, 40.0% had early complications (p<0.001), as shown in Table 1. No relationship existed between comorbidities and the incidence of late postoperative complications (Table 2). Of those who did not present comorbidities, 12.0% had late complications, and of those who did, 10.0% had late postoperative complications.
| Early complications | |||
|---|---|---|---|
| Comorbidity | No | Yes | Total |
| No (%) | 91.3% | 8.7% | 100% |
| Yes (%) | 60% | 40% | 100% |
| Late complications | |||
|---|---|---|---|
| Comorbidity | No | Yes | Total |
| No (%) | 88.0% | 12.0% | 100% |
| Yes (%) | 90.0% | 10.0% | 100% |
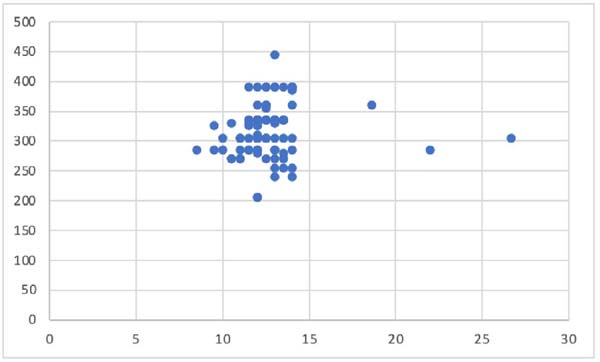
Considering complications in general, of those who did not have comorbidities, 19.6% had complications; of those who had, 50.0% showed a much higher percentage for those with comorbidities. A higher incidence of postoperative complications was observed in patients with longer surgical time (p=0.005). There was no relationship between the type of prosthesis surface and the incidence of complications (p=0.06). There was also no relationship between the access route for placing the prosthesis and the incidence of postoperative complications (p=0.12). The type of prosthesis placement also did not influence the incidence of postoperative complications (p=0.84). There was no relationship between surgical time and the incidence of complications (p=0.03). There was no association between the breast base’s size and the chosen implant’s volume (p=0.43), as shown in Graph 1 below.
DISCUSSION
Regarding silicone breast implants, a Brazilian study published in 2019 showed that round silicone implants are the most prevalent3. Ninety-eight percent use implants filled with 100% silicone. According to the implant coverage surface, more than half of surgeons (52.51%) preferred microtextured implants in the submuscular plane and 45.36% when placed in the subfascial plane, followed by macrotexture in 25.64% of cases3.
In the present study, all patients received round breast implants except for one in whom an anatomical shape was placed due to her preference. In all cases, textured implants were used, considering that they present a lower capsular contracture rate than smooth implants, and the service’s preference is to use polyurethane implants in the case of patients undergoing post-bariatric plastic surgery.
Regarding the access route and the location for placing the implants, it was observed that the inframammary incision was chosen as the favorite by the vast majority of Brazilian surgeons (89.66%), and the subglandular location (54.78%) was the most common approach for implant placement3.
In the current study, the inframammary route was used in all cases, and the subglandular and subfascial pockets were used in 88.15% of patients, possibly being higher due to the routine of our service in placing implants in the subfascial plane, except for patients who present formal indication for implant placement in the submuscular plane. In our institution, the placement of axillary and umbilical implants is also not performed due to the lack of materials necessary for this procedure and the lack of trained staff. There is still no consensus regarding the best access route and breast implant plan, and, at the moment, the best results are still based on a systematized routine, precise surgical dissection, and minimal contamination7.
Regarding the volume of the implant, a Brazilian study showed that the prostheses used varied from 220g to 460g, depending on the need assessed by the doctor and each patient’s preference. The most chosen ones are between 295g and 325g, with an average of 315.5g8. Considering that the present study was also conducted in Brazil and presents a similar patient profile, an average implant volume of 332.5g in the right breast and 335g in the left breast was observed.
It is known that the main complication of breast augmentation is capsular contracture, with almost half of cases occurring in the first two years9. Capsular contracture rates (Baker scale grades III and IV) in 10 years of follow-up were 9.2% for breast augmentation and 14.5% for breast reconstruction9. The confirmed rupture rate was 9.4%, with no report of extracapsular silicone gel migration9. In our study, one grade I capsular contracture case was observed during the minimum follow-up period of 18 months.
Early postoperative complications of breast augmentation include hematoma, seroma, infection, poor positioning of the implant, and pain9. Late postoperative complications include infection, seroma, capsular contracture, implant animation (excessive, unusual, painful) or distortions, implant visibility, poor positioning (descent, double bubble, cascade deformity, etc.), rippling of the implant, wrinkling and palpability, implant rupture, symmastia, poor healing or scar hypertrophy9. One option to reduce complications, such as the feared surgical wound dehiscence and early breast ptosis, would be the tactic of closing a fascial flap in the inframammary fold10.
A Brazilian study published in 2021 observed a late seroma rate of 0.429%8. The presence of a late seroma should always draw attention to the possibility of diagnosing BIA-ALCL. The present study observed no early or late seroma cases, possibly due to the smaller sample size.
The 410 Allergan pivotal study concluded that the most commonly reported complication of breast implant surgery is capsular contracture,9 and the risk of this complication has been increasing over time, with rates of capsular contracture (Baker scale grades III and IV) at 10 years of follow-up of 9.2% for breast augmentation, and 14.5% for breast reconstruction9.
According to other sources, this complication occurs in 2.4-14% of patients undergoing aesthetic breast augmentation, depending on multiple factors11. Almost half of capsular contractures occur within the first 2 years of implantation and 80% within the first 5 years11, with a complication-related reoperation rate of up to 15% within the first year.
In our study, capsular contracture was observed in two patients (2.63%), a lower rate than that found in other articles, since the patients were followed for a shorter period and possibly other patients will develop this complication over time, with rates similar to those found in the literature if followed for at least 10 years after implant placement.
It was also observed that smoking is an important risk factor for capsular contracture and, therefore, a contraindication to surgery2, one of the reasons why surgeries were not performed on smokers. Currently, treatment for capsular contracture after subglandular implant placement is best performed with capsulectomy and conversion to the subpectoral plane.
Data in the literature regarding the frequency of recurrence of capsular contracture are scarce, although it can almost be expected in patients with bilateral capsules2. The decision to get, keep, or remove breast implants is the patient’s choice. Some patients require reintervention due to capsular contracture or implant rupture, in which case reoperation is imperative12. However, in an increasing number of people, the decision to remove the implant is based on the patient’s wishes12. In the case of the two patients who presented capsular contracture in the present study in the initial Baker grades (I and II), it was decided to maintain expectant management.
Regarding factors related to trying to minimize the presence of capsular contracture, the use of nipple shields, pocket irrigation with an antibiotic solution, the “no-touch” technique, and other infection prevention measures can limit the rate of contracture13.
Regarding preoperative BMI and the incidence of complications, it was observed that a recent study with 2,565 patients comparing BMI above/below 21 found no difference in the incidence of capsular contracture after primary breast augmentation11. Other studies did not report any impact of BMI on the rate of complications11. In the present study, it was observed that, of patients without obesity or other comorbidities, only 8.7% had early postoperative complications, and of those with any comorbidity, 40.0% had early postoperative complications. Regarding late postoperative complications, this association was not true (p=0.8).
A study on 906 patients (of which 103 were smokers) who underwent aesthetic breast augmentation showed a significantly higher incidence of seroma when the patient was a smoker11. In the present study, it was impossible to make this correlation since patients with a history of active smoking were not included2. Surgical time must also be considered in planning, as it was directly proportional to the incidence of postoperative complications in the present study.
Another factor associated with the potential risk of capsular contracture is the location of the incision that gives access to the breast pocket. According to a retrospective study on 183 patients by Jacobson et al.14, transaxillary surgery significantly results in the highest number of cases of capsular contracture (6.4%) followed by periareolar (2.4%) and lastly, inframammary approach ( 0.5%). In our study, all breast implants were placed via the inframammary route, as this is the most commonly performed access in our service, and during the follow-up of patients undergoing breast augmentation, two presented capsular contracture, and both underwent placement of inframammary implants. Considering that the capsular contracture was in Baker grades I and II, it was decided to maintain expectant management.
CONCLUSION
The presence of comorbidities and prolonged surgical time directly influence the incidence of postoperative complications after breast augmentation. Adequate compensation for patients preoperatively and a methodical organization of time intraoperatively must be carried out in order to improve patient outcomes in the long term.
1. Universidade Estadual Paulista, Botucatu, SP,
Brazil
Corresponding author: Oona Tomiê Daronch Rua Prof. Dr. Mauro Rodrigues de Oliveira S/N, Botucatu, SP, Brazil, Zip Code: 18618-688, E-mail: oona.daronch@yahoo.com.br






 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter