

Original Article - Year 2023 - Volume 38 -
Differences in the profile of postoperative complications in patients undergoing breast augmentation and mastopexy with prosthesis
Diferenças no perfil de complicações pós-operatórias em pacientes submetidas a mamoplastia de aumento e mastopexia com prótese
ABSTRACT
Introduction: Breast augmentation is one of the most performed procedures in Plastic Surgery worldwide. Mastopexy with prosthesis is also a widely performed procedure reserved for other patient profiles. Many complications can be avoided when studying risk factors for unfavorable outcomes.
Method: This is a retrospective study carried out through the analysis of medical records of patients who underwent primary breast augmentation and mastopexy with breast implants from January 2018 to December 2020.
Results: Of the 112 patients who underwent mammoplasty with the implant during the study period, 76 patients underwent primary breast augmentation (67.86%), and 36 underwent mastopexy with breast implant (32.14%). Patients undergoing mastopexy had a higher average age compared to those undergoing breast augmentation (p<0.001) and had smaller volumes of breast implants (p=0.002). The most common complications in both groups include surgical wound dehiscence, more common after mastopexy with prosthesis.
Conclusion: Breast augmentation performed as a single procedure has a higher rate of complications when compared to breast augmentation performed individually. However, the greater number of early complications observed with the combined procedure is the sum of the two distinctly individual procedures and not an exponential increase.
Keywords: Mammaplasty; Intraoperative complications; postoperative complications; Breast; Reconstructive surgical procedures.
RESUMO
Introdução: A mamoplastia de aumento é uma dos procedimentos mais realizados em Cirurgia Plástica em todo o mundo. A mastopexia com prótese também é um procedimento amplamente realizado, reservado para outro perfil de pacientes. Muitas complicações podem ser evitadas quando se estudam os fatores de risco para desfechos desfavoráveis.
Método: Trata-se de um estudo retrospectivo realizado por meio da análise de prontuários de pacientes submetidas a mamoplastia primária de aumento e mastopexia com implantes mamários no período de janeiro de 2018 a dezembro de 2020.
Resultados: Das 112 pacientes submetidas a mamoplastia com implante mamário no período do estudo, 76 foram submetidas a mamoplastia de aumento primária (67,86%) e 36 pacientes a mastopexia com implante mamário (32,14%). As pacientes submetidas a mastopexia apresentaram maior média de idade em relação àquelas submetidas a mamoplastia de aumento (p<0,001) e apresentaram menores volumes de implantes mamários (p=0,002). As complicações mais comuns em ambos os grupos incluem a deiscência da ferida operatória, mais comum após mastopexia com prótese.
Conclusão: A mastopexia de aumento realizada em procedimento único apresenta maior índice de complicações quando comparada à mamoplastia de aumento realizada individualmente. No entanto, o maior número de complicações precoces observadas no procedimento combinado é a soma dos dois procedimentos distintamente individuais e não um aumento exponencial.
Palavras-chave: Mamoplastia; Complicações intraoperatórias; Complicações pós-operatórias; Mama; Procedimentos cirúrgicos reconstrutivos.
INTRODUCTION
Mastopexy with breast implants constitutes the vast majority of aesthetic procedures performed in Plastic Surgery1. In the early days of this surgery, silicone implants were initially placed in one surgical stage, and mastopexy was performed in a second stage, as it was believed that combining the procedures increased the risk of complications. However, there are recognized many advantages to performing these procedures simultaneously, the most obvious being preventing a second operation in many patients2. Several studies have shown that, for the appropriate patient, a single-stage augmentation mastopexy can be a safe and effective procedure to reconstruct the ptotic breast.3.
Currently, mastopexy with implants is a surgery widely performed mainly in patients who presented significant weight changes, in cases after pregnancy and breastfeeding, or in older patients who developed significant breast ptosis4. Multiple techniques for surgical correction of hypomastia and breast ptosis have been described since the first documentation in the literature in the 1960s by Regnault and Ulloa.
Although surgical techniques have evolved, the basic principles for achieving the balance between the parenchymal mass and the skin envelope remain under debate.5.The use of prosthetic implants as an adjunct to mastopexy is considered by many to improve the overall results and longevity of the procedure when compared to mastopexy without implants.5.
On the other hand, the profile of the majority of patients undergoing breast augmentation is young, they want a significant breast contour, and they do not have breast ptosis or, when they do, it is often possible to perform periareolar mastopexy with the placement of breast implants. The biggest complaint is the loss of projection in the upper pole and the bulging of the lower pole; however, around a third of dissatisfied patients have results above the expected standard6.
Therefore, it is essential to understand the differences in these different groups of patients and study the factors related to the incidence of complications to intervene in these factors and reduce unfavorable long-term outcomes, which were investigated in the present study.
OBJECTIVE
The objectives of the study were to carry out an epidemiological assessment of patients undergoing primary breast augmentation and mastopexy with prostheses and to verify the main factors related to the incidence of complications in the early (first 30 days after surgery) and late (after 30 days), considering that the study of risk factors offers an opportunity to make changes in the variables related to the incidence of complications and, consequently, improve the long-term outcome of patients.
METHOD
This is a retrospective study carried out through the analysis of medical records of patients who underwent primary breast augmentation and mastopexy with breast implants between January 2018 and December 2020. All patients registered in the surgical center with the procedure called “Non-aesthetic female breast plastic” registered by Plastic Surgery at the surgical center of the Hospital de Clínicas of the Faculdade de Medicina de Botucatu (UNESP, São Paulo, Brazil) during the mentioned period. Plastic Surgery chief preceptors assist resident surgeons and do not have an assistant to perform both breasts simultaneously; therefore, each breast is performed separately.
The inclusion criteria were patients undergoing primary breast augmentation during the study period, excluding patients undergoing other breast surgical procedures, secondary breast augmentation, concomitant surgeries at the same surgical time, and patients who presented incomplete data in the medical record for the appropriate study. of the data. The standard of the service is to operate on patients who are at the appropriate weight (preferably body mass index - BMI - < 25kg/m2). Patients undergoing secondary breast surgery, patients who underwent surgery at the same surgical time as combined procedures, and incomplete medical records to correctly fill in data at work were excluded.
Furthermore, patients who smoke are not operated on and are advised to stop smoking at least 12 weeks before and 12 weeks after the procedure. In patients undergoing primary breast augmentation without mastopexy in conjunction, the standard is not to place drains postoperatively. There is usually a preference for inframammary access. Generally, it is decided to place a periareolar breast implant in cases where patients have some degree of breast ptosis in the initial phase, and the correction is performed at the same surgical time. In patients undergoing mastopexy, in most cases, suction drains are not placed.
In our institution, axillary implants are not placed due to the lack of materials necessary for this procedure and the lack of trained staff. Transumbilical access is also not performed, as all breast implants used are silicone. All implants were from the same commercial brand. We do not present any conflicts of interest for the brand used in the service, nor do we receive financial or scientific support from it. The routine is to leave prophylactic antibiotics 7 days after the surgical procedure. Patients are also advised to wear a shaping bra for at least three months postoperatively.
The quantitative variables studied were age, length of stay, surgery time, and breast implant volume. The qualitative variables were Fitzpatrick skin type, presence of comorbidities, use of continuous medications, type of access for placing the breast implant, location of the implant (subfascial, subglandular or retromuscular), type of access (periareolar or inframammary), surface the prosthesis used (smooth, textured or polyurethane), presence of complications in the early and late postoperative period.
The patients in the present study were followed for at least 48 months, with the first follow-up being carried out three days after surgery, the second in one week, the third in 1 month, and after 3, 6, and 12 months of surgery traditionally. Patients who presented complications were followed up at shorter intervals, respecting the needs of each condition.
Of the patients included, the medical records were reviewed, and the studied data was entered into Google Docs forms. Statistical analyses were carried out using the SPSS 20.0 program from the Excel spreadsheet generated. As for statistical analysis, the variables were studied and presented in their mean values and standard deviation or frequencies. The Kolmogorov-Smirnov test was used to study the normality of quantitative variables, and as they presented normal distribution, the Student’s t-test was applied for independent samples. The Chi-square or Fisher’s Exact test was used for qualitative variables to study the association between them. Values of p<0.05 were considered statistically significant.
RESULTS
Of the 112 patients who underwent mammoplasty with breast implants during the study period, 76 underwent primary breast augmentation (67.86%), and 36 patients underwent mastopexy with implants (32.14%). Of the patients undergoing primary breast augmentation, 12 (15.79%) had some comorbidity, and in the group of patients who underwent mastopexy with prosthesis, there were 7 patients (19.44%) with comorbidities. The mean preoperative BMI in patients undergoing breast augmentation and mastopexy with prosthesis was similar, 22.23kg/m2 and 22.21kg/m2, respectively. The average size of the breast base was 12.49cm in patients who underwent breast augmentation and 12.66cm in mastopexy patients with prostheses. Figures 1 and 2 show preand postoperative photos of a patient undergoing mastopexy with prosthesis, and Figures 3 and 4 show preand postoperative photos of a patient undergoing primary subfascial breast augmentation.
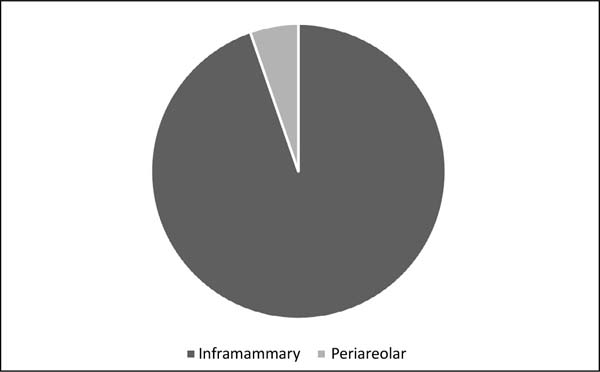
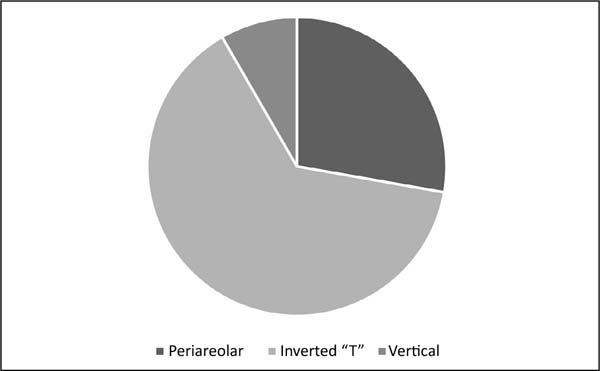
The surgical techniques used in augmentation mammoplasty and mastopexy with prosthesis can be seen in Graphs 1 and 2. All patients were discharged on the first postoperative day.
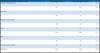
It was observed that the average age of patients was higher in mastopexy with prosthesis compared to patients undergoing primary breast augmentation (p<0.001). On the other hand, the chosen breast volume was greater in patients undergoing breast augmentation compared to mastopexy with prostheses (p=0.002), as seen in Table 1. There were no differences in the presence of comorbidities in patients undergoing these surgical procedures. There were also no differences in the choice of prosthesis placement plan concerning the two groups (p=0.78).
| Breast augmentation | Mastopexy with prostheses |
P | ||
|---|---|---|---|---|
| Age (years) | Average | 28.3 | 34.3 | < 0.001 |
| SD | 7.7 | 7.4 | ||
| Volume (ml) | Average | 329.1 | 304.2 | 0.002 |
| SD | 40.4 | 38.2 |
SD: standard deviation.
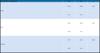
The most common complications in both groups include surgical wound dehiscence, more common after mastopexy with prostheses, as seen in Table 2. Figure 5 illustrates a case of surgical wound dehiscence in a patient undergoing mastopexy with breast implants. In general, there was a higher incidence of postoperative complications in patients undergoing mastopexy compared to the group of patients undergoing breast augmentation alone (p=0.01).
| Complications (in absolute and relative value) | Breast augmentation | Mastopexy with prostheses | |
|---|---|---|---|
| Surgical wound dehiscence | 5 | 8 | 13 |
| % | 6.6 | 22.2 | 11.6 |
| Hematoma | 1 | 1 | |
| % | 0.0 | 2.8 | 0.9 |
| Surgical wound infection | 1 | 1 | |
| % | 0.0 | 2.8 | 0.9 |
| None | 71 | 25 | 96 |
| % | 93.4 | 69.4 | 85.7 |
| PTE | 1 | 1 | |
| % | 0.0 | 2.8 | 0.9 |
| TOTAL (absolute number) | 76 | 36 | 112 |
| TOTAL (%) | 100.0 | 100.0 | 100.0 |
The first line of each complication represents the absolute number of cases, and the second line represents the relative value (in %).
Patients undergoing mastopexy had a higher average age compared to patients undergoing breast augmentation (p<0.001) and had smaller volumes of breast implants (p=0.002). There was no relationship between the largest breast volume chosen and the lower incidence of complications. On the contrary, a statistically significant relationship existed between smaller breast volumes and the incidence of postoperative complications, as shown in Table 3.
| Postoperative complications | No | Yes | p |
|---|---|---|---|
| Early | 324.4 | 300.9 | 0.03 |
| 41.7 | 32.1 | ||
| Late | 324.2 | 296.9 | 0.02 |
| 40.0 | 44.1 | ||
| General | 327.7 | 301.3 | 0.003 |
| 40.8 | 36.1 |
Longer surgical time was not related to a higher incidence of postoperative complications in breast augmentation (p=0.97) or mastopexy with breast implants (p=0.26). In general, there was a higher incidence of general postoperative complications in mastopexy with prostheses compared to breast augmentation (p=0.001). Age was a variable unrelated to the incidence of early (p=0.18) or late (p=0.98) postoperative complications in any of the surgeries.
A higher incidence of early postoperative complications was observed in patients who had at least some comorbidity preoperatively. In those without comorbidities, the percentage of early complications is 8.7%, whereas for those with any comorbidity, this percentage increases to 40.0% (p<0.0001). On the other hand, this relationship was not observed in late postoperative complications (p=0.8).
Of the 76 patients who underwent breast augmentation, 12 (15.8%) had some postoperative complication, and all of them had their prostheses placed in the subfascial plane (p<0.0001). Concerning the 36 patients who underwent mastopexy with prostheses, the subfascial plane was also the one with the highest incidence of complications (30.5%), followed by the subglandular plane (p=0.003), and there were no complications when placed in the dual plane (p=0.003).
DISCUSSION
The combination of breast augmentation with mastopexy is gaining popularity for two main reasons: (1) the limits of subglandular or submuscular placement, individually, to correct skin laxity adequately, and (2) a surgical pexy can only address ptosis through the superior repositioning of pre-existing tissues and is not sufficient to restore to the breast the firmness, shape and skin firmness, volume (especially the fullness of the upper pole) of a young breast7.
The most obvious advantage of a one-stage breast augmentation and mastopexy procedure is that it avoids a second operation, saving you money and reducing the risks related to an additional operation. The goal of single-stage augmentation mastopexy is to convert deflated asymmetrical ptotic breasts into youthful conical symmetrical breasts using a reliable technique that increases volume while restoring nipple position8.
Regarding the profile of patients undergoing breast augmentation, 505 questionnaires answered by Brazilian plastic surgeons were studied, and it was observed that the most common practices included the use of round microtexture implants and polyurethane-coated silicone in the primary procedure, subglandular pocket, inframammary incisions, preoperative sizing with round implant samples, intravenous and oral antibiotics, double antibiotic irrigation, implant size range generally less than 325ml and no drainage9. Similarly, in the present study, the majority of patients received round breast implants and had an inframammary incision, with an average implant volume of 340ml.
In addition to the patient profile, it is imperative to study postoperative results. It was observed that the degree of satisfaction of patients undergoing mastopexy with insertion was excellent, and there was a favorable impact on the quality of life and well-being of the patients evaluated, with the post-surgical result classified as regular or good4. Although round implants are the most used in aesthetic surgery, aesthetic superiority was observed in the anatomical implant group concerning general appearance (standardized mean difference, 0.06; 95% CI, -0.40 to 0.53), naturalness (standardized mean difference, 0.18; 95% IC, -1.51 to 1.15), projection, upper pole contour, and lower pole contour10.
A study carried out with 1,406 patients, 1298 of whom underwent breast augmentation and 108 mastopexies with prostheses1 showed a mean age of 29.6 years and 32.2 years, respectively (p=0.006). The average size of the implants was 340ml and 308ml (p=0.001), respectively. Surgical wound infection was observed in 0.6% of breast augmentation and 3.7% in mastopexy with prostheses. Surgical wound dehiscence was lower in breast augmentation (1.1%) compared to 6.5% in patients undergoing mastopexy with prostheses (p=0.001).
In the present study, the average age was similar, being 28.3 years in the breast augmentation group and 34.3 years in patients undergoing mastopexy with prostheses (p<0.001). The average volume of implants was also smaller in the present study: in the mastopexy group with prostheses (304.2ml) compared to patients who received breast augmentation (329.1ml), with statistically significant differences (p=0.002).
Regarding the incidence of complications, there were no cases of surgical wound infection in breast augmentation, with one case in the mastopexy group with prostheses. There were 8 cases of surgical wound dehiscence (22.22%) in the mastopexy with prostheses group and 5 cases (6.6%) in the case of patients undergoing breast augmentation.
The results confirm that when breast augmentation is performed as a single procedure, it presents a higher rate of complications when compared to breast augmentation performed individually1. However, the greater number of early complications seen in the combination procedure is the addition of the two distinctly individual procedures and not an exponential increase. There were no cases of deep vein thrombosis, pulmonary embolism, or death in the study mentioned above or in the present work. The technique of placing silicone breast implants in the subfascial plane, followed by wide anterior dissection of the fascia of the pectoralis major muscle, completely separating it from the rest of the breast parenchyma, was effective in the treatment of patients with breast ptosis11.
Another study published with 332 cases2 showed that, in mastopexy with prostheses, the complication rate was 22.9% (for primary cases, 20.4%; for secondary cases, 28.9%). The rate of implant-related complications was 7.8%. The number of cases of early complications in the present study was 30.55%, but of late complications, it was 16.66%, obtaining an average similar to the rate of general complications in the already published study.
In a Brazilian study with 64 patients undergoing mastopexy with implants, it was observed that the main complications were 3 cases (4.6%) of residual skin sagging at an 8-month follow-up, two cases (3.1%) of unsightly scars, one case (1.5%) of partial areola necrosis11. There were no cases of infection or seroma. In our study, there was one case of infection and no case of areola necrosis. To prevent subsidence, wound dehiscence, and ultimately for proper implant positioning, it is essential to provide adequate coverage and support of the lower pole of the breast.12.Correct preoperative analysis and the choice of the best technique for augmentation mastopexy are crucial for good results as there is no universal technique for treating all types of breasts.13.
CONCLUSION
The most interesting finding of this study was that not only in mastopexy with implants but also in breast augmentation, also considered low-risk and elective surgery in healthy individuals, and some factors could be identified that were associated with an increased risk of complications. The main difference between both groups is age, with breast augmentation being performed mainly on younger patients. The main complication of both surgeries is surgical wound dehiscence, and controlling comorbidities and body mass index can reduce the risk of complications.
1. Universidade Estadual Paulista, Botucatu, SP, Brazil
Corresponding author: Oona Tomiê Daronch Rua Prof. Dr. Mauro Rodrigues de Oliveira S/N, Botucatu, SP, Brazil, Zip Code: 18618-688, E-mail: oona.daronch@yahoo.com.br
















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter