

Original Article - Year 2023 - Volume 38 -
Supraclavicular flap for head and neck oncological reconstruction: A series of 62 cases
Retalho supraclavicular para reconstrução oncológica em cabeça e pescoço: Uma série de 62 casos
ABSTRACT
Introduction: The oncological reconstruction of extensive defects in the head and neck requires the plastic surgeon to make a difficult decision between the use of free flaps and pedicled flaps. The supraclavicular flap is one of the main examples of a pedicled flap, being versatile, with a thin thickness and similar color to the region to be reconstructed.
Method: A retrospective study was carried out by collecting data from medical records of patients admitted to the Cancer Institute of the State of São Paulo between December 2010 and March 2020.
Results: Among the 62 patients reconstructed with a supraclavicular flap, 37 were male and 25 female. Fifty-eight patients (93.5%) had some associated comorbidity. In total, 27 complications related to the flap (43.5%) were recorded, 5 of which were total necrosis (8%).
Conclusion: The supraclavicular flap plays an important role in head and neck oncological reconstructions and should be considered as an option in patients who are poor candidates for microsurgical flaps.
Keywords: Head and neck neoplasms; Perforator flap; Reconstructive surgical procedures; Case reports; Head; Neck; Patients.
RESUMO
Introdução: A reconstrução oncológica de defeitos extensos em cabeça e pescoço impõe ao cirurgião plástico a difícil decisão entre o uso de retalhos livres e retalhos pediculados. O retalho supraclavicular é um dos principais exemplos de retalho pediculado, sendo versátil, com espessura delgada e cor semelhante à região a ser reconstruída.
Método: Um estudo retrospectivo foi realizado através da coleta de dados de prontuário de pacientes internados no Instituto do Câncer do Estado de São Paulo, entre dezembro de 2010 e março de 2020.
Resultados: Dentre os 62 pacientes reconstruídos com retalho supraclavicular, 37 eram do sexo masculino e 25 do sexo feminino. Cinquenta e oito pacientes (93,5%) possuíam alguma comorbidade associada. Ao todo, 27 complicações relacionadas ao retalho (43,5%) foram registradas, sendo 5 necroses totais (8%).
Conclusão: O retalho supraclavicular possui importante papel nas reconstruções oncológicas de cabeça e pescoço e deve ser considerado como opção em pacientes maus candidatos a retalhos microcirúrgicos.
Palavras-chave: Neoplasias de cabeça e pescoço; Retalho perfurante; Procedimentos cirúrgicos reconstrutivos; Relatos de casos; Cabeça; Pescoço; Pacientes.
INTRODUCTION
The oncological reconstruction of extensive areas in the head and neck requires the plastic surgeon to make a difficult decision between the use of free flaps and pedicled flaps. Free flaps are classically considered the gold standard treatment, but they prolong surgical time, increasing procedure costs and postoperative recovery time. Thus, pedicled flaps have re-emerged in recent years as an option to be considered in elderly patients with advanced cancer and clinically weakened patients who benefit from simpler reconstructive techniques1,2.
Among the pedicled flaps, we can use myocutaneous and fasciocutaneous flaps. The former is usually the choice in deeper areas, which require soft tissue for filling3. On the other hand, fasciocutaneous flaps are excellent options for thinner coverage, adaptable to the contour in the cervicofacial segment.
The supraclavicular flap has been increasingly used to reconstruct defects after head and neck oncological resections. It is versatile, has a thin thickness and a similar color to the region to be reconstructed. Furthermore, it has reliable vascularization and is easy to dissect, making it reproducible in low-complexity services.
OBJECTIVE
To present a series of cases of supraclavicular flap, demonstrating the feasibility of this surgery for oncological reconstruction in the head and neck in tumors of different histological types and different stages.
METHODS
A retrospective study was carried out by collecting data from medical records of patients admitted to the Instituto do Câncer of the State of São Paulo between December 2010 and March 2020. During this period, 62 patients underwent reconstruction with supraclavicular flaps by the plastic surgery team for head and neck oncological reconstructions.
The Ethics Committee approved the study for Analysis of Research Projects of the Hospital das Clínicas of the Faculty of Medicine of the University of São Paulo - HCFMUSP (CAAE Number: 58900522.6.0000.0068).
The following information was collected: epidemiological data, comorbidities, histological type and staging of the treated tumor, type of resection, defect area (calculated by photographic analysis), pathological margins, neoadjuvant or adjuvant complementary therapy, recurrence, and complications. The defect area was calculated by photographic analysis using Adobe Photoshop® software.
RESULTS
Among the 62 patients reconstructed with a supraclavicular flap, 37 were male, and 25 were female. Fifty-eight patients (93.5%) had some associated comorbidity, the most prevalent being systemic arterial hypertension (53.2%), smoking (53.2%), and alcohol consumption (30.6%) (Table 1). The average age was 64.1 years, with a median of 65.5 years.
| Value/Percentage | ||
|---|---|---|
| Sex | Feminine | 21 (41.1%) |
| Masculine | 30 (58.8%) | |
| Comorbidities | Systemic arterial hypertension | 26 (55.3%) |
| Smoking | 25 (53.2%) | |
| Alcoholism | 18 (38.3%) | |
| Diabetes mellitus | 15 (31.9%) | |
| Dyslipidemia | 6 (12.8%) | |
| Obesity | 5 (10.6%) | |
| Histological type | Squamous cell carcinoma | 36 (70.5%) |
| Sarcoma | 5 (9.8%) | |
| Basal cell carcinoma | 5 (9.8%) | |
| Salivary gland tumor | 4 (7.8%) | |
| Neuroendocrine tumor | 1 (1.9%) | |
| Free margins | Yes | 37 (72.5%) |
| No | 13 (25.5%) | |
| Unknown | 1 (1.9%) | |
| Cervical emptying | Selective | 26 (50.9%) |
| Radical | 7 (13.7%) | |
| Unrealized | 18 (35.3%) | |
| Neoadjuvance | Yes | 2 (3.9%) |
| No | 49 (96%) | |
| Adjuvance | Yes | 30 (63.8%) |
| No | 21 (41.2%) | |
| Additional reconstruction |
Yes | 11 (21.6%) |
| No | 40 (78.4%) | |
| Retail complications | Yes | 27 (52.9%) |
| No | 24 (47%) | |
| Donor area complications |
Yes | 4 (7.8%) |
| No | 47 (92.2%) |
The most prevalent histological type was squamous cell carcinoma of the head and neck, present in 45 cases (72.5%), 9 of which were in the larynx. Sarcoma (8%), basal cell carcinoma of the skin (6%), salivary gland tumors (4%), neuroendocrine tumors (1.96%) and melanoma (1.61%) were also treated.
Among squamous cell carcinomas (SCC), stages T2 (33.3%) and T3 (37.8%) were the most prevalent. Only 4 cases of early tumor, T1 (8.9%), and 8 cases of locally advanced tumor, T4 (17.8%), were included.
Clear margins were obtained in 48 resections (77.4%). In 13 patients, compromised margins were maintained due to the morbidity of the required enlargement, but all underwent adjuvant radiotherapy. There was also 1 case of unknown margin, as the resection was performed in an external service without a record in the medical records. The final area to be reconstructed was an average of 40.62 cm2, varying from 0.78cm2 (salivary fistula) to 137.15cm2.
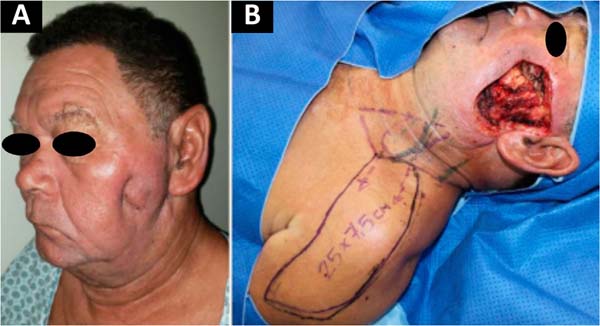
In Figure 1, we have a patient who underwent total parotidectomy extended to the skin due to myxoid liposarcoma. In Figure 2, we see the same patient and his postoperative result of reconstruction with a pedicled supraclavicular flap. In Figure 3, the same patient is during intraoperative planning.
Neck dissection was performed in 41 cases (66.1%), 32 of which were selective dissections (51.6%), and 9 were modified radicals (14.5%). Twenty-one patients (33.9%) did not undergo lymphadenectomy. Only three patients received neoadjuvant chemotherapy before the procedure. Adjuvant therapy was performed in 34 patients, 23 of whom received exclusively radiotherapy and 11 chemoradiotherapy.
For full coverage of the area, some form of additional reconstruction, in addition to the supraclavicular flap, was necessary in 13 patients (21%). The most used were microsurgical fibula flap (4) and skin graft (3). Complementary reconstruction with a microsurgical osteomyocutaneous fibula flap was performed in 4 cases, in addition to a sural nerve graft for reconstruction of the facial nerve in 1 patient.
In total, 37 complications related to the flap (43.5%) were recorded, 16 of which were partial necroses (25.8%), 11 dehiscences (17.7%), 5 total necrosis (8%), 3 salivary fistulas (4.8%), 1 hematoma (1.6%) and 1 bleeding (1.6%). Reoperation was necessary in 15 patients (29.4%), of which 9 were converted to another form of reconstruction.
In all cases, the donor area was closed primarily. Complications in the donor area occurred in 4 patients, 3 of which were dehiscence and 1 seroma. All were treated conservatively.
The average number of surgeries performed per patient until the reconstruction was completed, including the treatment of complications and touch-ups, was 2.92.
The information is gathered in Table 1.
DISCUSSION
Surgeries for head and neck reconstruction are still challenging for plastic surgery. The professional who deals with this area must know how to combine function (speech, facial expression, chewing, and breathing) with aesthetics, as it involves areas in a region that determine appearance and self-esteem4.
Free flaps have gained great prominence and have established themselves as the choice for covering extensive head and neck injuries. However, due to the prolonged surgical time and the common profile of cancer patients - elderly, smoker, and with several comorbidities - not every patient is a candidate for reconstruction with a microsurgical flap2. Therefore, pedicled flaps remain an option. The benefits inherent to faster dissection and transfer reduce morbidity related to prolonged general anesthesia and often eliminate the need for intensive postoperative care1.
The supraclavicular flap is an axial flap based on supraclavicular branches of the transverse cervical vessels, the first reports of which date back to the 19th century. Its use, however, was restricted due to the unreliability of its vascular supply, explained by the lack of anatomical studies at the time when it was performed randomly5.
In 1979, its axial vascularization pattern was initially described by Lamberty6. It was rediscovered as an excellent reconstructive option in 1997 by Pallua et al.3,7-9, being applied in the treatment of cervical retractions due to burns, and in 2009 by Chiu et al. as a reliable alternative in head and neck oncological reconstruction1.
It is a thin, flexible fasciocutaneous flap with skin with a texture similar to that of the face, making it an ideal source of soft tissue for head and neck reconstructions10. In this way, it surpasses the results obtained with other regional flaps, such as pectoralis major and trapezius, which are bulky and poorly adaptable to the contour of the region1,2. It is a flap that allows the maintenance of facial expression and mobility of the cervical region3. Currently, the angiosome of its pedicle is well described, based on recent studies that demonstrate its vascular anatomy10.
The flap dissection technique was standardized and popularized by Pallua et al. in 19972. The flap must be quadrangular in shape; its pedicle must be found within the triangle demarcated between the anterior border of the sternocleidomastoid muscle, the clavicle, and the external jugular vein; its size must be between 4 and 12cm wide and 20 to 30cm long7.
It is a versatile flap, capable of covering lesions located up to the limit between the middle and distal third of the face. Its reach differentiates it from other pedicled flaps in this region, such as the deltopectoral and pectoral flaps, since its rotation point is more proximal, providing a more suitable arc of rotation for the cervicofacial region. Furthermore, as it is hairless, it is suitable for reconstructions in the oral cavity or the rest of the upper aerodigestive tract2.
In our series, eight pharyngeal reconstructions were performed with this flap. We can also mention the possibility of tunneling the flap, which avoids a new approach and reduces scarring in the donor area.
Adequate knowledge of the anatomy of the supraclavicular flap and the improvement of its dissection technique allowed us to use it to reconstruct more extensive and complex defects. In our service, the average area of the defect to be reconstructed is relatively large (40.62cm2), larger than what had previously been described in the literature, demonstrating the possibility of reconstructing larger defects with a relatively simple technique with low morbidity.
The supraclavicular flap can be raised quickly, as its superficial pedicle ensures that the entire dissection is restricted to the subfascial plane. Previous series have demonstrated an average dissection time of 50 minutes2, which is advantageous in patients undergoing long-term oncological surgeries. The donor area is usually closed primarily, without major sequelae3.
In the present study, we observed a relatively high rate of flap-related complications (52.9%). However, some of these were minor complications, such as partial necrosis or small dehiscence (44.4%), at rates similar to those found in the literature9. Two patients undergoing pharyngeal reconstruction presented salivary fistulas, which were treated conservatively without compromising the final swallowing function. Further studies to evaluate the main causes of complications related to the supraclavicular flap should be carried out.
We must emphasize that although this flap is reliable, it still has its limitations. It is not recommended for complex reconstructions resulting from extensive or deep areas due to its smaller volume. It is also not applicable in cases of late reconstructions, in which the integrity of the pedicle is uncertain.12 In these situations, free flaps still play a leading role. Even so, in this series, we were able to successfully reconstruct 4 defects resulting from locally advanced cancers (T4), and there are even studies that demonstrate its application in this type of tumors2.
CONCLUSION
The supraclavicular flap plays an important role in oncological reconstructions of the head and neck. Due to the reliability of its pedicle, shortened surgical time, and low morbidity to the donor area, it should be considered as an option in patients who are poor candidates for microsurgical flaps.
1. Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São
Paulo, SP, Brazil
2. Instituto do Câncer do Estado de São Paulo, Divisão de Cirurgia Plástica, São Paulo,
SP, Brazil
Corresponding author: Giulia Godoy Takahashi Rua Arruda Alvim, 423, apto 51, Pinheiros, São Paulo, SP, Brazil, Zip Code: 05410-020, E-mail: giu.godoy@gmail.com









 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter