

Original Article - Year 2024 - Volume 39 -
Breast reconstruction with TRAM: abdominal tomographic evaluation
Reconstrução mamária com TRAM: avaliação tomográfica abdominal
ABSTRACT
Introduction: The transverse rectus abdominis muscle flap (TRAM) is a method of breast reconstruction with good aesthetic results and does not require the use of silicone implants for better body contouring. It was originally described by Holmstrom in 1979 as an ellipse of skin and fat based on an isolated muscle on its vascular pedicle. The systematic reconstruction of the wall defect installed after flap transposition using polypropylene mesh was described in a previous study by Cunha. The article aims to evaluate changes in the abdominal wall, after the systematization of polypropylene mesh placement during TRAM reconstruction surgery.
Method: This is a retrospective cohort study that evaluates possible changes in the abdominal wall of patients undergoing the TRAM flap with preand postoperative abdominal computed tomography.
Results: A reduction in the size of the abdominal cavity of, on average, 14.5% and 14.2% in the thickness of the abdominal wall subjected to TRAM was evidenced. The greatest reduction in abdominal wall thickness was in a patient who underwent a bipedicled flap, with 50.7%. The complications presented were umbilical hernia, late seroma, perithellal fibrosis, and thread granuloma.
Conclusion: In this study, tomography after surgery demonstrated a reduction in the volume of the abdominal cavity and thickness of the abdominal wall, which did not statistically influence the appearance of abdominal hernia, bulging, mesh extrusion, or other deformities.
Keywords: Mammaplasty; Abdominal wall; Abdominal cavity. Myocutaneous flap. Abdominal muscles
RESUMO
Introdução: O retalho transverso do músculo reto abdominal (TRAM) é um método de reconstrução mamária com bons resultados estéticos e dispensa o uso de próteses de silicone para melhor contorno corporal. Foi originalmente descrito por Holmstrom em 1979, como uma elipse de pele e gordura com base em um músculo isolado no seu pedículo vascular. A reconstrução sistematizada do defeito da parede instalado após a transposição do retalho com o uso de tela de polipropileno foi descrita em estudo prévio por Cunha. O artigo tem como objetivo avaliar as alterações na parede abdominal, após a sistematização da colocação da tela de polipropileno durante a cirurgia de reconstrução com TRAM.
Método: É um trabalho de coorte retrospectivo que avalia as possíveis alterações da parede abdominal de pacientes submetidos ao retalho TRAM com tomografia computadorizada de abdome pré e pós-operatórias.
Resultados: Foi evidenciada uma redução do tamanho da cavidade abdominal de, em média, 14,5% e 14,2% na espessura da parede abdominal submetidas ao TRAM. A maior redução da espessura da parede abdominal foi de um paciente submetido ao retalho bipediculado, com 50,7%. As complicações apresentadas foram hérnia umbilical, seroma tardio, fibrose peritela e granuloma de fio.
Conclusão: Nesse estudo, a tomografia após a cirurgia demonstrou a redução no volume da cavidade abdominal e espessura da parede abdominal, o que não influenciou estatisticamente no aparecimento de hérnia abdominal, abaulamentos, extrusão da malha ou outras deformidades.
Palavras-chave: Mamoplastia; Parede abdominal; Cavidade abdominal; Retalho miocutâneo; Músculos abdominais
INTRODUCTION
The transverse rectus abdominis muscle flap (TRAM), described by Holmstrom in 19791, is a breast reconstruction method composed of an ellipse of skin and fat based on an isolated muscle in its vascular pedicle1.
The use of autologous tissue allows breast reconstruction with good aesthetic results and eliminates the need for silicone implants for better body contouring2. It is known that bulges and hernias arise mainly in the lower abdomen due to the absence of posterior aponeurosis of the rectus abdominis muscle inferior to the arcuate line of Douglas, making this region with high rates of complications3. TRAM is beneficial for the patient when it can ensure a strong abdominal wall that allows the resumption of work activities4. Given several established techniques, Cunha et al., in 20215, described the technique for systematizing the reconstruction of the abdominal wall with polypropylene mesh, due to its easy reproduction and applicability6, and can be effective in preventing the occurrence of high rates of abdominal hernias and bulges in the postoperative period described in the literature.
Due to different techniques, studies indicate difficulties in comparing hernia and abdominal bulging. For Mizgala et al.6, among 150 patients, none had a hernia, but 3 unipedicled and 8 bipediculated patients had a visible protuberance. Kroll & Marchi7 reported a bulge or hernia in 21% of cases and a reduction to 5% when fascial closure in two layers of the anterior rectus sheath was performed.
Some authors understand that mesh is necessary when primary synthesis is not possible, due to the risk of infection and extrusion8. A suitable synthetic mesh must have the following characteristics: not produce foreign bodies, not be carcinogenic or allergenic, and be able to resist mechanical stress. Furthermore, the thread must be inert, non-absorbable, and monofilament7.
OBJECTIVE
To evaluate tomographically the behavior of the abdominal structure and the incidence of complications in the abdominal wall in patients undergoing the same type of post-TRAM abdominal reconstruction.
METHOD
The cohort and prospective study are based on the selection of patients who underwent TRAM in the plastic surgery service of the Hospital Regional de Sobradinho, DF, from January 2019 to December 2020 and who had preoperative abdominal tomography scans performed 1 year after postoperative. There were 14 patients operated on during this period, but only eight participants met the inclusion factors. The patients underwent a monopedicled or bipedicled TRAM flap, and the donor area was repaired using the technique described and standardized in the previous work by Cunha et al.5.
Among the 14 patients operated on during the period by the same plastic surgery team at the Hospital Regional de Sobradinho, two were excluded due to changes in pre-operative tomography scans; two did not undergo postoperative CT scans, one did not sign the Consent Form and one was lost to follow-up. After the exclusion factors, eight patients remained for the research.
The evaluation of preand postoperative tomography scans was performed by the same radiologist and reviewed by another assistant radiologist. In addition, all patient demographic data were evaluated based on a review of medical records by the responsible researcher, and authorization for research was approved by all patients, through the Informed Consent Form.
The patients underwent the procedure and a minimum follow-up of 12 months with the same surgical team. All of them had computed tomography scans of the abdomen without contrast in the preoperative evaluation, and outpatient follow-up was done 15 days, 1 month, 3 months, 6 months, and 1 year after surgery, and after 12 months new tomographic images were requested.
Assessments of abdominal hernia, bulging, or other deformities in the abdominal wall were analyzed using computed tomography. The parameters evaluated in comparative tomography scans before and after surgery were the presence of hernia, abdominal cavity volume, abdominal wall thickness, bulging, mesh extrusion, and the presence of granuloma.
The reference points used to measure the volume of the abdominal cavity in the CT scans were the following: longitudinal diameter in the midline of the upper limit of the pubic symphysis and units of measurement in centimeters, transverse, and anteroposterior (AP) at the height of L3 (vertebral column) and measurement unit in cm; the final volume in cubic centimeters from the formula:
Longitudinal x transverse x AP x 0.56.
The reference point used to evaluate wall thickness was the paramedian to the right at the height of the navel and measurement unit in millimeters.
The study inclusion factors were patients undergoing polypropylene mesh placement in unilateral or bilateral breast reconstruction with a monopedicled or bipedicled TRAM flap, patients with preoperative tomography, and 12 months after surgery.
RESULTS
During the preoperative consultation, the demographic profile of the patients undergoing surgery was assessed: two patients were hypertensive, and none were diabetic or smokers (Table 1). The average age of the eight patients was 42 years (Table 1).
| Number of patients | 8 (100%) |
|---|---|
| Age range | 32 - 54 |
| Average Age | 42 |
| Smoking | 0 (0%) |
| Hypertension | 2 (25%) |
| Diabetes | 0 (0%) |
| Monopedicled TRAM | 1 (12.5%) |
| Bipedicled TRAM | 7 (87.5%) |
| Immediate reconstruction | 4 (50%) |
| Late reconstruction | 3 (37.5%) |
| Mixed reconstruction | 1 (12.5) |
| Right breast | 3 (37.5%) |
| Left breast | 4 (50%) |
| Right and left breast | 1 (12.5%) |
| Degree of satisfaction | 7 (87.5%) |
TRAM: transverse rectus abdominis muscle flap
Of the eight patients, seven (87.5%) received bipedicled flaps and one (12.5%) received monopedicled flaps (Table 1). The left breast was operated on in four patients (50%), the right breast in three patients (37.5%), and one patient (12.5%) underwent bilateral surgery (Table 1). Furthermore, four patients underwent immediate reconstruction (50%), three patients underwent delayed reconstruction (37.5%) and one patient (12.5%) underwent immediate reconstruction on the left side and delayed reconstruction on the right side (Table 1). When asked about the degree of satisfaction with the aesthetic appearance of the breasts, seven patients responded that they were satisfied and one was dissatisfied.
Patients who underwent delayed reconstruction had a waiting time between mastectomy and breast reconstruction of approximately 18 months. All patients were diagnosed with invasive ductal carcinoma (IDC) on pathological examination and only one patient presented metastasis to the axillary lymph node (Table 2). Furthermore, two patients underwent only adjuvant radiotherapy (25%), one patient (12.5%) underwent adjuvant radiotherapy and neoadjuvant chemotherapy, three patients (37.5%) underwent adjuvant chemotherapy and radiotherapy (Table 2), and two patients did not undergo additional treatments.
| Oncological profile | Patients |
|---|---|
| Adjuvant RT | 2 |
| Adjuvant RT + neoadjuvant CT | 1 |
| Adjuvant QT + adjuvant RT | 3 |
| Anatomopathological (IDC) | 8 |
IDC: invasive ductal carcinoma; QT: chemotherapy; RT: radiotherapy
Furthermore, one patient (12.5%) presented pulmonary thromboembolism (PTE) after the first day of surgery, which was evidenced by chest CT angiography, and was therefore hospitalized for 3 days. Only two patients (25%) required a new operation, and the patient who presented PTE also developed an infection of the flap on the right, requiring successive debridement. The other patient required hematoma drainage.
In general, a reduction in the size of the average abdominal cavity of 14.5% was evidenced in patients undergoing TRAM and 17.9% in patients undergoing monopedicled TRAM (Table 3). Furthermore, an average reduction of 14.2% in the thickness of the abdominal wall overall was demonstrated, and the greatest reduction was in a patient with late bilateral breast reconstruction, using a bipedicled flap, with 50.7% (Table 3). No patient presented bulging.
| Variation | Reduction Average | |
|---|---|---|
| Volume of the abdominal cavity (VAC) | 23.8% - 8.9% (TV) 1165cm3 - 476cm3 | 14.5% (TAR) |
| Thickness of the abdominal wall (TAW) | 50.7% - 5.6% (TV) 7.1mm - 0.4mm |
14.2% (TAR) |
| Monopedicled (VAC) | 6249cm3 - 5125cm3 | 17.9% |
| Monopedicled (TAW) | 7mm - 6.5mm | 7.1% |
| Bipedicled (VAC), (GV) | 4880cm3 - 3715cm3 | 23.8% |
| Bipedicled (TAW), (GV) | 14mm - 6.9mm | 50.7% |
| Bipedicled (VAC), (LV) | 5331cm3-4855cm3 | 8.9% |
| Bipedicled (TAW), (LV) | 7.1mm - 6.7mm | 5.6% |
| Patients | Hernias | Bulging | Extrusion of the mesh | Granuloma wire | Complications | |
|---|---|---|---|---|---|---|
| Bipedicled | 7 | 12.5% | 0% | 0% | 12.5% | 0% |
| Monopedicled | 1 | 0% | 0% | 0% | 0% | 12.5% - Late seroma |
| Total | 8 | 12.5% | 0% | 0% | 12.5% | 12.5% |
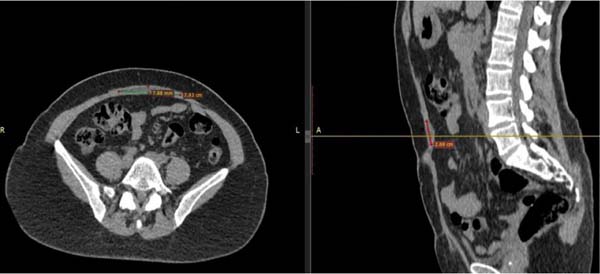
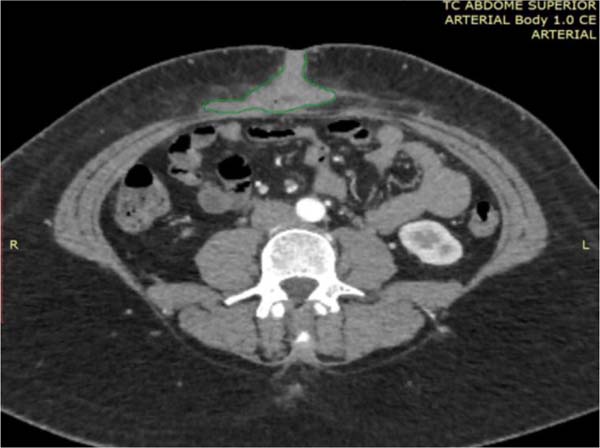
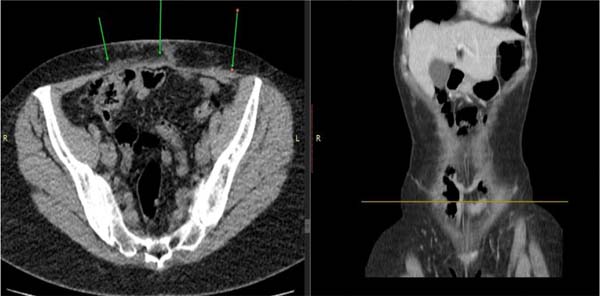
Only one patient had an umbilical hernia measuring 2.04 cm on postoperative tomography (Figure 3). Another patient presented with a seroma 11 months after surgery in the supraumbilical region between the aponeurosis and the mesh, measuring 9.55ml (Figures 1 and 2). Another patient presented fibrosis around the mesh (Figures 5 and 6). Thread granuloma was revealed in one patient (12.5%) by tomography at 6 months, without clinical repercussions (Figure 4).
DISCUSSION
The rectus abdominis muscle originates from the pubis (between the pubic tubercle and the symphysis) and is inserted into the fifth to seventh costal cartilage and the xiphoid process of the sternum9. It has 3 to 4 horizontal tendinous insertions that are adhered to the anterior layer of the rectum10, and its irrigation is classified as type III by Mathes and Nahai (superior and inferior epigastric artery), it has 6 to 10 perforators11,12.
Although breast reconstructions with TRAM are generally successful, there is some concern among surgeons when using TRAM, due to the need to maintain the competence of the abdominal wall postoperatively. In 1976, D. Ralph Millard pioneered the idea of reconstructing the female breast from a vertically oriented island of abdominal skin, that is, with a vertical musculocutaneous flap from the rectus abdominis13.
The patients participating in this study are heterogeneous and, ideally, were compared with the same type of pedicle, reconstruction time, and no changes in the abdominal wall preoperatively. Only one patient had a small umbilical hernia and only one had thread granuloma with inflammatory signs. Complications were not evaluated in another study due to the systematization of the technique used having been first applied to these groups of patients after 20195.
In monopedicled flaps, the smaller defect in the donor area and the preservation of the contralateral rectus abdominis muscle influence the lower incidence of hernias and bulging14. In this study, 1 patient had a late seroma on computed tomography, while another had perithellal fibrosis, but none of the radiological images in this group showed bulging or large deformities in the abdominal wall. The first studies appeared in 1987 with Hartrampf et al.4, who evaluated complications in 335 patients undergoing breast reconstruction with TRAM. The general rate of abdominal wall complications was 1.5%, with 0.3% referring to abdominal hernia, 0.6% to abdominal bulging, and 0.6% to a defect in the upper sheath of the rectus abdominis muscle4.
The use of polypropylene mesh with systematization of fixation points, corroborated in another study with the same surgical team, provided a low rate of hernia and no bulging or extrusion of the mesh5.
This work was innovative, as it analyzed differences in the volume of the abdominal cavity and the thickness of the abdominal wall, before and after surgery. The average reduction in the volume of the abdominal cavity ranged from 8.9% to 23.8%, and the thickness of the abdominal wall ranged from 5.6% to 50.7%.
Due to the inflammatory reaction caused by the mesh, perithellal fibrosis is triggered, which may justify, in some cases, the low rate of average reduction in the thickness of the abdominal wall. The most significant change in the reduction of abdominal wall thickness (50.7%) occurred in one patient, who underwent a bipedicled flap, but there were no complications. However, the patient with an umbilical hernia in the postoperative period presented a variation of 9.2% of the abdominal wall.
Even with these data, there was no correlation between this reduction and changes such as hernias, bulges, mesh extrusions, thread granulomas, or other abnormalities.
Unlike previous published studies, in which they were evaluated primarily by physical examination and, only in cases of doubt about whether to perform an abdominal ultrasound post-operatively, the present study considered it relevant to perform a pre-operative tomography examination, to analyze the existence of previous deformities15,16.
Only two patients showed changes in postoperative CT scans compatible with late seroma and perithellal fibrosis. According to Baroudi & Ferreira17, abdominal surgeries result in seroma due to the dead space resulting from detachment and resulting in incidences ranging from 2.1 to 9.4%7. According to Scevola et al.18, analyzing 769 breast reconstructions with TRAM, the use of two drains in the abdomen reduces the incidence of seroma. And it has already been shown in several studies that the use of polypropylene mesh to correct any defects in the abdominal wall induces an intense inflammatory reaction, with the formation of fibrosis, and a decrease in the elasticity of the wall19,20.
CONCLUSION
In this study, tomography after surgery demonstrated an average reduction of 14.5% in the volume of the abdominal cavity and 14.2% in the thickness of the abdominal wall. There was no evidence of an abdominal hernia, bulging, mesh extrusion, or other deformities. Furthermore, although bipedicled flaps present greater variation in abdominal wall thickness, there was no correlation in the abdominal wall or complications.
Despite the evaluation of a small number of cases, satisfactory tomographic results were found, avoiding the appearance of complications in the reconstructive technique applied.
REFERENCES
1. Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982;69(2):216-25.
2. Brasil. Ministério da Saúde. Instituto Nacional de Câncer José Alencar Gomes da Silva (INCA). Coordenação de Prevenção e Vigilância. Estimativa 2018: incidência de câncer no Brasil. Rio de Janeiro: Ministério da Saúde/INCA; 2017.
3. Holmström H. The free abdominoplasty flap and its use in breast reconstruction. In: Seventh International Congress of Plastic and Reconstructive Surgery; 1979; Rio de Janeiro, RJ, Brazil.
4. Hartrampf CR Jr. Breast reconstruction with a transverse abdominal island flap: A retrospective evaluation of 355 patients. Plast Reconstr Surg. 1987;1(1):123-35.
5. Cunha AS, Costa RSC, Daher JC, Silva SV, Castro COP, Damasio AA, et al. Sistematização de reconstrução da parede abdominal pósreconstrução com TRAM. Rev Bras Cir Plást. 2021;36(1):15-20.
6. Mizgala CL, Hartrampf CR Jr, Bennett GK. Assessment of the abdominal wall after pedicled TRAM flap surgery: 5- to 7-year followup of 150 consecutive patients. Plast Reconstr Surg. 1994;93(5):988-1002; discussion 1003-4.
7. Kroll SS, Marchi M. Comparison of strategies for preventing abdominal-wall weakness after TRAM flap breast reconstruction. Plast Reconstr Surg. 1992;89(6):1045-51; discussion 1052-3.
8. Roxo CP, Carvalho TM, Borba MA, Silva LRB, Roxo ACW. Reconstrução de parede abdominal com tela aloplástica após infecção por micobactéria. Rev Bras Cir Plást. 2012;27(2):340-3.
9. Neligan PC. Mama. In: Neligan PC. Cirurgia plástica. 3ª ed. Volume 5. Rio de Janeiro: Elsevier; 2015.
10. Drever JM. Total breast reconstruction. Ann Plast Surg. 1981;7(1):54-61.
11. Watterson PA, Bostwick J 3rd, Hester Junior TR, Bried JT, Taylor GI. TRAM flap anatomy correlated with a 10-year clinical experience with 556 patients. Plast Reconstr Surg. 1995;95(7):1185-94.
12. Moore KL, Dalley AF, Agur AMR. Moore Anatomia orientada para a clínica. 7ª ed. Rio de Janeiro: Guanabara Koogan; 2014.
13. Millard DR Jr. Breast reconstruction after a radical mastectomy. Plast Reconstr Surg. 1976;58(3):283-91.
14. Rossetto LA, Abla LE, Vidal R, Garcia EB, Gonzalez RJ, Gebrim LH, et al. Factors associated with hernia and bulge formation at the donor site of the pedicled TRAM flap. Eur J Plast Surg. 2010;33(4):203-8.
15. Marques EGSC, Jorge JLG, Andrade CZN, Silva MF, Farina Junior JA. Reparação da parede abdominal com tela dupla de polipropileno e poliglecaprone pós-retalho TRAM em reconstrução mamária. Rev Bras Cir Plást. 2014;29(4):544-9.
16. Miranda RE, Pereira JB, Gragnani Filho A. Uso de duas telas de polipropileno na área doadora do TRAM para reconstrução mamária: avaliação na incidência de hérnia e abaulamento abdominal. Rev Bras Cir Plást. 2015;30(4):560-6.
17. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41.
18. Scevola S, Youssef A, Kroll SS, Langstein H. Drains and seromas in TRAM flap breast reconstruction. Ann Plast Surg. 2002;48(5):511-4.
19. D`Acampora JA, Kestering DM, Soldi MS, Rossi LF. Experimental study comparing the tensile strength of different surgical meshes following aponeurotic-muscle deformity synthesis on Wistar rats. Acta Cir Bras. 2007;22(1):47-52.
20. Pascual G, Rodríguez M, Sotomayor S, Pérez-Köhler B, Bellón JM. Inflammatory reaction and neotissue maturation in the early host tissue incorporation of polypropylene prostheses. Hernia. 2012;16(6):697-707.
1. Hospital Daher Lago Sul, Brasília, DF,
Brazil
Corresponding author: Igor Moura Soares Hospital Daher Lago Sul SHIS QI 07 conj. F, Brasília, DF, Brazil. Zip code: 71615-310, E-mail: igormoura739@gmail.com








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter