

Case Report - Year 2024 - Volume 39 -
Tumor resection and partial skin graft placement on the scalp in a patient with Neurofibromatosis type 1
Ressecção do tumor e colocação de enxerto de pele parcial no couro cabeludo em um paciente com neurofibromatose tipo 1
ABSTRACT
Neurofibromatosis type 1 (NF1) is an inherited neurocutaneous disorder in which tumors form in the nervous system (neurofibromas). Neurofibromas are the most common benign tumors in NF1. The type, size, number, and location of the neurofibromas should be considered for the choice of treatment. We present a case of NF1, in which a wide scalp resection was performed due to the presence of multiple neurofibromas. Associated with this, reconstruction was performed with advancement flaps plus partial skin autograft with favorable results and good coverage of the areas where the tumors were removed.
Keywords: Transplantation, autologous; Neurofibromatosis 1; Neurofibroma; Scalp; Plastic surgery procedures
RESUMO
A neurofibromatose tipo 1 (NF1) é um distúrbio neurocutâneo hereditário no qual se formam tumores no sistema nervoso (neurofibromas). Os neurofibromas são os tumores benignos mais comuns na NF1. O tipo, o tamanho, o número e a localização dos neurofibromas devem ser considerados para a escolha do tratamento. Apresentamos um caso de NF1, no qual foi realizada uma ampla ressecção do couro cabeludo devido à presença de múltiplos neurofibromas. Associado a isso, a reconstrução foi realizada com retalhos de avanço mais autoenxerto de pele parcial, com resultados favoráveis e boa cobertura das áreas onde os tumores foram removidos.
Palavras-chave: Transplante autólogo; Neurofibromatose 1; Neurofibroma; Couro cabeludo; Procedimentos de cirurgia plástica
INTRODUCTION
The scalp is an area of considerable thickness, little elasticity, and abundant vascularization. These characteristics make surgical procedures in the area difficult due to the appearance of complications such as profuse intraoperative bleeding. We present a case of NF1 in which a wide scalp resection was performed due to the presence of multiple neurofibromas and reconstruction with advanced flaps plus partial skin autograft (PSA).
CASE HISTORY
A 44-year-old male patient, with a history of NF1, hypertension, and type 2 diabetes mellitus, came to the Department of Plastic and Reconstructive Surgery due to the presence of multiple tumors of varying shapes and sizes on the scalp, some of them with purulent discharge and pain. Ten years ago, local surgical resection of neurofibromas in the nose was performed. On physical examination, multiple neurofibromas were seen on the scalp and face (Figure 1), café-au-lait spots on the axillary flexure, and Lisch nodules.

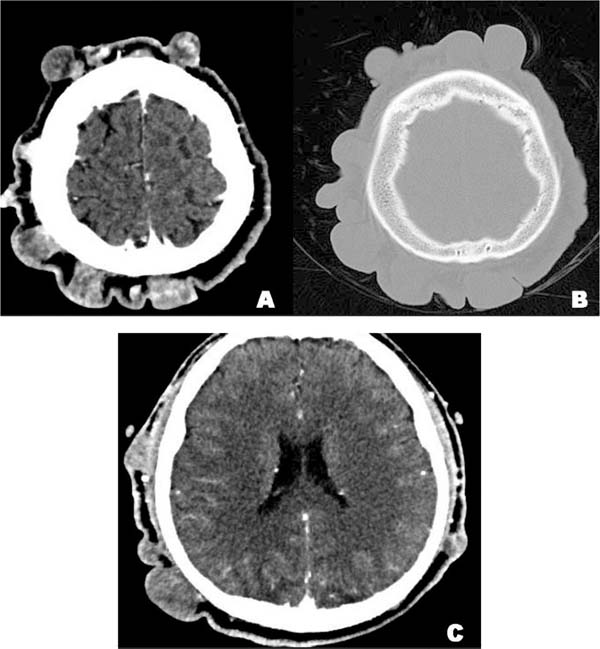
In the Computerized Tomography (CT) of the head and neck, scattered nodular formations of different sizes with a density equivalent to soft tissue are observed in the scalp, and with irregular enhancement in the image after contrast administration, characteristics corresponding to neurofibromas (Figure 2A). The surrounding bone tissue was intact, without the presence of erosions or signs of intracranial extension (Figure 2B/2C).
Due to the clinic, the size, and wide distribution of the neurofibromas, it was decided to perform a partial surgical excision of the scalp. The procedure involved a two-stage approach due to the impracticality of individually excising extensive and progressive neurofibromas on the scalp. The first stage included the radical resection of affected scalp areas, followed by the placement of a PSA for rapid coverage.
This decision considered patient preferences and the explanation of treatment options. Free tissue transfer was chosen over local flaps to address scalp defects, aiming to prevent adherence failure and defect enlargement. The use of a PSA for scalp reconstruction was preferred for its simplicity and functionality.
Regarding the surgical intervention. After administration of general anesthesia with endotracheal intubation, the lesions were marked with methylene blue, then Klein’s tumescent solution was infiltrated in the subperiosteal plane. With a number 15 scalpel, a cut is made perpendicular to the scalp on the pre-marked design. With electrocautery, dissection was performed up to the periosteal plane, removing the scalp with the neurofibromas (Figure 3). Advancement flaps are made with Baroudi sutures (progressive tension sutures) on all edges, achieving the reduction of the resulting defect.
The PSA was harvested with an electrical dermatome, the donor area was the anterolateral aspect of the right thigh. The PSA was prepared by placing it on paraffin gauze, with diffuse micro-openings made with a scalpel 11, and after placement, it was sutured with a tie-over dressing. A hydrocolloid dressing and a compressive bandage were placed on the donor area. The patient had postoperative recovery without complications.
The PSA is discovered on day 10, finding good integration, without the presence of residual ulcers, hematomas, or seromas (Figure 4). In the donor area, it was found in the process of re-epithelialization, so it was decided to place a new hydrocolloid dressing plus an occlusive bandage. The patient was discharged, and he did not require any type of coverage over the donor area and the PSA had a good evolution.
DISCUSSION
NF1 is an autosomal dominant genetic disease with multiorgan involvement and has an approximate global prevalence of 1 case per 3,000 live births1. All cases have a germline mutation of the NF1 gene, however, there is a high variability in the presentation of clinical characteristics1. The main clinical feature of NF1 is neurofibroma, a nerve sheath tumor formed from spinal, peripheral, or cranial nerves.
Neurofibromas are the most frequent benign tumors in NF1 and different types have been described, such as cutaneous, subcutaneous, and plexiform neurofibromas2. Other clinical features include pigmentary lesions (café au lait macule), skeletal abnormalities, behavioral abnormalities, and low-grade gliomas1.
The most common and striking dermatological finding of NF1 is the presence of several cutaneous neurofibromas (cNFs) of different sizes and shapes2. cNFs have several cellular components (Schwann cells, fibroblasts, macrophages, and mast cells) and are supported by an extracellular matrix within the dermis1,3.
cNFs have several stages depending on their clinical appearance: the nascent stage (not clinically observable), the flat stage (thinning or hyperpigmentation of the skin), the sessile stage (raised papule), the globular stage (a base of 20 to 30 mm and height), and the pedunculate stage (dermal contents supported by a visible stalk)4. Common neurological concomitant symptoms of cNFs are pain and itching, and inadequate drying after wetting can cause maceration, skin breakdown, and superficial infections5.
It should be noted that physical disfigurement from multiple neurofibromas is associated with less quality of life due to psychosocial burden, low self-esteem, and interference with daily, social, and economic activities6. This is why treatment is justified, especially with the presence of severe symptoms and/or aesthetic disfigurement4. In our case, the presence of multiple neurofibromas was evidenced, mainly in the scalp, which caused an important aesthetic disfigurement in the head, concomitant pain, and signs of infection such as purulent discharge.
Currently, there is no accepted gold standard for the treatment of cNFs5. For the choice of treatment, the type, size, number, and location of the neurofibroma should be considered4. Surgical excision is still the most effective method, however, it does not prevent the formation of future neurofibromas5. People with NF1 generally have an extensive tumor burden that covers a large area of their body surface and due to the progression of the disease, the surgical procedures that are performed are usually multi-stage4.
In our case, due to the progression, and extensive extension of the neurofibromas in the scalp, individual excision of each neurofibroma was not feasible, so it was decided to perform a more robust surgical approach in 2 stages, first with radical resection of the neurofibroma. Affected scalp area and subsequent placement of the PSA, obtaining favorable results in the short term7. This treatment decision was made taking into account the patient’s preferences and needs, who chose after having all of his treatment options explained to him.
Another therapeutic technique that could have been used is local scalp flaps (advancement or rotation) previously expanded with tissue expanders since they present certain advantages such as a better aesthetic finish in color and texture, resistance, and long-term durability9. However, to cover scalp defects it is advisable to perform free tissue transfer instead of local flaps, since the failure of adherence to the flaps can increase the defect10. For the reconstruction of the scalp a PSA was placed as it was the simplest and most functional form that ensured a rapid coverage of the exposed area10. However, identification and excision of these tumors early in their development would have given better aesthetic results.
Although the use of PSA is a convenient technique for the reconstruction of large scalp defects, these grafts have some disadvantages11. Alopecia would be one of the future consequences of the placement of the PSA12. An autologous hair transplant from preserved areas of the scalp could be an alternative for alopecia, however, this technique is reserved for small areas13. In addition, Schwann cells are considered to be the tumor cells of cNFs,2 and they make up an important cell population in the dermis14, therefore, their presence in the PSA and autologous hair transplant could lead to the future development of cNFs in the area. Furthermore, PSA mobilization is limited and not similar to that of the normal scalp, and they are sometimes quite fragile and susceptible to shear forces.12 In our patient we prioritized a reconstruction that would allow us to cover the entire scalp and easily observe the appearance of tumors in the future.
CONCLUSION
In this report, we describe the surgical management of multiple cNFs on the scalp in a patient with NF1. The resection of the affected scalp and the reconstruction of the resected area with advancement flaps and placement of partial skin autograft gave acceptable results that will have a positive impact on the patient’s quality of life in the future.
REFERENCES
1. Gutmann DH, Ferner RE, Listernick RH, Korf BR, Wolters PL, Johnson KJ. Neurofibromatosis type 1. Nat Rev Dis Primers. 2017;3:17004.
2. Allaway RJ, Gosline SJC, La Rosa S, Knight P, Bakker A, Guinney J, et al. Cutaneous neurofibromas in the genomics era: current understanding and open questions. Br J Cancer. 2018;118(12):1539-48.
3. LE LQ, Kesterson RA, Gutmann DH. Defining the Research Landscape for Dermal Neurofibromas. Oncol Times. 2016;38(18):14-5.
4. Chamseddin BH, Hernandez LN, Solorzano D, Vega J, Le LQ. Robust surgical approach for cutaneous neurofibroma in neurofibromatosis type 1. JCI Insight. 2019;4(11):e128881.
5. Chamseddin BH, Le LQ. Management of cutaneous neurofibroma: current therapy and future directions. Neurooncol Adv. 2019;2(Suppl 1):i107-i116.
6. Taylor LA, Lewis VL Jr. Neurofibromatosis Type 1: Review of Cutaneous and Subcutaneous Tumor Treatment on Quality of Life. Plast Reconstr Surg Glob Open. 2019;7(1):e1982.
7. Park H, Min J, Oh TS, Jeong WS, Choi JW. Scalp Reconstruction Strategy Based on the Etiology of the Scalp Defects. J Craniofac Surg. 2022;33(8):2450-4.
8. Costa DJ, Walen S, Varvares M, Walker R. Scalp Rotation Flap for Reconstruction of Complex Soft Tissue Defects. J Neurol Surg B Skull Base. 2016;77(1):32-7.
9. Bas S, Oner C, Eren HI, Hacikerim Karsidag S, Yilmaz A. Reconstruction of Complex Scalp Defects in Different Locations: Suggestions for Puzzle. Sisli Etfal Hastan Tip Bul. 2021;55(3):349-58.
10. Desai SC, Sand JP, Sharon JD, Branham G, Nussenbaum B. Scalp reconstruction: an algorithmic approach and systematic review. JAMA Facial Plast Surg. 2015;17(1):56-66.
11. Lee KK, Mehrany K, Swanson NA. Scalp Reconstruction. In: Rohrer TE, Cook JL, Kaufmann A, eds. Flaps and Grafts in Dermatologic Surgery. Chapter 10. Edinburgh: Saunders; 2007. p. 117-24.
12. Lane C, Lin A, Goyal N. Scalp and Calvarium Reconstruction. Otolaryngol Clin North Am. 2023;56(4):741-55.
13. Leedy JE, Janis JE, Rohrich RJ. Reconstruction of acquired scalp defects: an algorithmic approach. Plast Reconstr Surg. 2005;116(4):54e-72e.
14. Bray ER, Chéret J, Yosipovitch G, Paus R. Schwann cells as underestimated, major players in human skin physiology and pathology. Schwann cells as underestimated, major players in human skin physiology and pathology. Exp Dermatol. 2020;29(1):93-101.
1. Universidad Nacional De San Agustín de
Arequipa, Peru
Corresponding author: Elizbet Susan Montes-Madariaga Urb. José Luis Bustamante y Rivero, Cerro Colorado, Arequipa, Peru, E-mail: emontesma@unsa.edu.pe









 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter