

Original Article - Year 2024 - Volume 39 -
Demystifying the deep plane facelift technique with anatomical dissection in fresh cadavers
Desmistificando a técnica de deep plane facelift com dissecção anatômica em cadáveres frescos
ABSTRACT
Introduction: Anatomy studies on cadavers have allowed a better understanding of the structures of the face and, consequently, greater safety when exploring the deep planes of the facial region. A good technique must be safe, reproducible, and respect anatomical points. The objective of this work is to demystify the deep plane facelifting technique through the dissection of cadavers and exposure of facial structures.
Method: The reproduction of the "deep plane facelifting" technique was performed on 14 hemifaces of 7 pieces of fresh cadavers at the Instituto de Treinamento de Cadáver (Cadaver Training Institute) in Curitiba in 2021. The surgical technique was performed according to our clinical practice and reproduced on the cadaver. After the procedure, the facial anatomical structures were dissected to correlate their positioning with the anatomical spaces of the face. The positioning of the facial ligaments, vascularization, and branches of the facial nerve were evaluated.
Results: The anatomical spaces relevant to the deep plane facelifting technique were identified, such as the inferior and superior masseteric spaces, prezygomatic space, buccal space, and cervical space. The facial nerve branches were identified in the sub-SMAS plane and correlated with the anatomical spaces and planes.
Conclusion: The deep plane facelift technique can be reproduced safely as long as two parameters are respected. The first is the correct entry into spaces to respect the anatomy. The second is the use of blunt detachers for dissection in the deep planes of the face to avoid nerve damage to the branches of the facial nerve.
Keywords: Face; Rhytidoplasty; Facial nerve; Superficial musculoaponeurotic system; Skin aging
RESUMO
Introdução: Os estudos de anatomia em cadáveres permitiram um melhor entendimento das estruturas da face e, consequentemente, mais segurança ao explorar os planos profundos da região facial. Uma boa técnica deve ser segura, reprodutível e respeitar os pontos anatômicos. O objetivo deste trabalho é desmistificar a técnica de deep plane facelifting por meio da dissecção de cadáveres e exposição das estruturas faciais.
Método: A reprodução da técnica de "deep plane facelifting" foi realizada em 14 hemifaces de 7 peças de cadáveres frescos no Instituto de Treinamento de Cadáver em Curitiba no ano de 2021. A técnica cirúrgica foi realizada conforme nossa prática clínica e reproduzida no cadáver. Após o procedimento, as estruturas anatômicas faciais foram dissecadas para correlacionar seu posicionamento junto aos espaços anatômicos da face. Foram avaliados os posicionamentos dos ligamentos da face, vascularização e os ramos do nervo facial.
Resultados: Foram identificados os espaços anatômicos relevantes à técnica de deep plane facelifting, como os espaços massetéricos inferior e superior, espaço pré-zigomático, espaço bucal e espaço cervical. Os ramos do nervo facial foram identificados no plano subSMAS e correlacionados com os espaços e planos anatômicos.
Conclusão: A técnica de deep plane facelift pode ser reproduzida com segurança desde que sejam respeitados dois parâmetros. O primeiro é a entrada correta nos espaços a fim de respeitar a anatomia. O segundo é o uso de descoladores rombos para dissecção nos planos profundos da face a fim de evitar lesão nervosa dos ramos do nervo facial.
Palavras-chave: Face; Ritidoplastia; Nervo facial; Sistema musculoaponeurótico superficial; Envelhecimento da pele
INTRODUCTION
Medical schools in Brazil carry out anatomy studies on anatomical specimens preserved in formaldehyde and studying fresh specimens has never been a Brazilian reality. After legislative changes, some private companies, with no ties to Brazilian universities, began to import fresh cadaver parts for the study of anatomy, a very common practice in several countries around the world. This enabled us, despite the high costs, to study the anatomy of the face in a completely innovative way for us, plastic surgeons. Facial surgery delights everyone, but it is also frightening due to the risks of nerve damage. At the same time, we always seek the best techniques to deliver good results to patients. It is not only the patients who demand it, but we also want to have postoperative results that are satisfactory and rewarding.
Facial rejuvenation surgery in deep planes has been widely publicized in recent years, with very good results, showing naturalness of the face postoperatively and faster recovery, however, it accesses planes and vascular and nervous structures that have always aroused temerity. Changing this reality made us return to the study of anatomy, and currently in fresh cadaver pieces, to discover whether the technique is safe and reproducible.
Concerning anatomy, we consider topography, stratigraphy, vascularization, innervation, and anatomical spaces to be important. About topography, the face is divided into thirds: upper third, middle third, and lower third. The midface is delimited by an upper horizontal line located over the zygomatic arch, which runs from the upper insertion of the helix to the lateral corner of the eye, and a lower horizontal line, which runs from the lower edge of the tragus to the lateral oral commissure. The upper third of the face is above and the lower third is below this lower horizontal line.
From a functional point of view, the face has an anterior aspect and a lateral aspect. The anterior surface is mobile and contains the muscles of facial expression, while the lateral surface is fixed and contains the muscles of mastication. A descending vertical line separates the front face from the side. This line contains the retaining ligaments of the face, such as temporal adhesion, lateral orbital thickening, masseteric ligaments, zygomatic ligament, and mandibular ligament.
Concerning stratigraphy, the face is subdivided into 5 layers. Layer 1 is the skin, layer 2 corresponds to the subcutaneous tissue, layer 3 is the SMAS, layer 4 is made up of deep fat, and layer 5 corresponds to the periosteum or deep fascia. Studies have shown that these layers change depending on the region of the face.
The anatomical spaces described by Mendelson are well-defined spaces, with determined limits, with loose tissue inside. Many spaces do not have vital structures. Retaining nerves and ligaments delimit the ends of the spaces. These spaces are avascular and allow access to the movable face. Basically, the existing spaces are as follows: temporal space, preseptal space, pre-zygomatic space, pre-maxillary space, superior and inferior pre-masseteric space, and buccal space1-3.
OBJECTIVE
The objective of this work is to demystify the deep plane facelifting technique through the dissection of cadavers and exposure of facial structures.
METHOD
The reproduction of the deep plane facelifting technique was carried out on 14 hemifaces of 7 pieces of fresh cadavers at the Instituto de Treinamento de Cadáver (Cadaver Training Institute) in Curitiba, PR, between March and June 2021. The authorization of the Ethics and Research Committee was number 65763122.8 .0000.5688. The first step was to identify topographic points in each anatomical piece of a fresh cadaver, such as the angle of the mandible, zygoma and zygomatic arch, lateral oral commissure, tragus, and sternocleidomastoid muscle. The skin marking of the incision was pre-tragal and the sub-SMAS entry site was precisely marked on the skin, according to the topographic points. This same marking was passed on to the SMAS after skin detachment, ensuring the correct entry point into the sub-SMAS.
For the initial skin marking, we located the angle of the mandible and defined it as the Point X of the zygoma. We mark a point 1.5cm above Point X and draw a line parallel to Line 1, which we call Line 3 (Figure 1).

To mark the entry point into the Sub-SMAS plane, we draw the access points to the sub-SMAS plane on lines 1, 2, and 3. In Line 1, we mark a point 3 cm from the skin incision; in Line 2, we mark a point 4cm from the skin incision and; in Line 3, we mark a point 3cm from the skin incision (Figures 2A, 2B e 2C).
We join these points, forming Line 4, the entry point of the sub-SMAS space. We marked a dotted line parallel to 1cm from the vertical line, corresponding to the advancement of the skin detachment, beyond the entry of the sub-SMAS plane. We draw an oblique line above Line 2, which corresponds to the entrance to the pre-zygomatic space, located below the orbicularis oculi muscle and above the zygomaticus major muscle (Figure 3).

Infiltration with saline was performed in the pretragal incision and in the subcutaneous area of detachment and deep infiltration for dissection of the sub-SMAS, to facilitate detachment. We use a total volume of approximately 10 to 15 ml on each side. The subcutaneous dissection extended to the dotted line. The subcutaneous flap was thick enough to contain fatty tissue. We maintained a homogeneous thickness throughout the entire length of the flap. The cervical skin dissection extended anteriorly to the sternocleidomastoid muscle.
The same marking made on the skin was passed on to the SMAS, with the reference lines and the entry line in the Sub-SMAS plane. We checked whether the markings made on the skin were identical to the internal markings in the SMAS. The pre-masseteric spaces accessed during the anatomical dissection were the inferior pre-masseteric space and the superior premasseteric space. The pre-zygomatic space begins at the lateral border of the orbicularis oculi muscle and was also dissected (Figure 4).
The entry into the sub-SMAS plane was initiated through the inferior pre-masseteric space, located between Line 3 and the previous marking line. We located the vertical line and pulled on both sides of the vertical line. We incised gently with a scalpel blade number 15, obliquely. We use Metzenbaum scissors and gently open the scissors vertically to further enlarge the space, then visualize the loose areolar tissue. The space is accessed when we visualize the presence of loose areolar tissue. Once the correct space has been confirmed, we use a Trepsat detacher to expand the dissection of the space to its limits, even reaching close to the mandibular ligament (Figures 5A, 5B e 5C).
To access the superior pre-masseteric space, between lines 1 and 2, we incised the SMAS with a scalpel blade number 15 and with the tip of Metzenbaum scissors below the SMAS entrance. The tip of the scissors was directed to the upper lip, with gentle vertical opening movements opening the upper space. We used the same entry technique with the tip of scissors, dissecting vertically and gently, with short, repeated movements. The area of the space is small, hence the need for short movements, with short opening amplitudes of the scissors. We use Trepsat to open up this space further.
We access the pre-zygomatic space with visualization of the orbicularis oculi muscle in its lateral part, elevate the muscle with forceps, and position the tip of the scissors vertically. We make gentle opening movements with the tip of the scissors and enter with a medium third peeler with a blunt and delicate tip. We perform gentle movements and release the orbicularis retaining ligament. We continued with the dissection towards the zygomaticus major muscle, over this muscle (Figure 6).
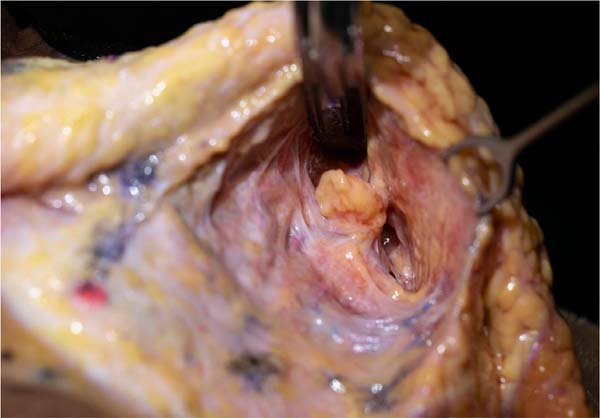
Access to the cervical region was achieved by locating the anterior edge of the sternocleidomastoid muscle on the anatomical specimen. We ensure a distance of 2cm below the angle and mandibular line. The platysma was incised in its lateral portion and used a blunt detacher to advance into the subplatysmal space to the anterior part of the neck (Figure 7).
After completing the steps of the deep plane facelift surgical technique, we dissect the anatomical piece considering the need to locate the retaining ligaments, important vessels, and the facial nerve and its branches.
Between the superior and inferior pre-masseteric spaces, we have the masseteric ligaments, which were sectioned until we found the inferior buccal branch of the facial nerve, present on the floor of the inferior pre-masseteric space. Between the pre-zygomatic and superior pre-masseteric spaces, we have the zygomatic ligaments, superior buccal nerve, and zygomatic nerves. In this location, we first released the zygomatic ligaments, which were close to the insertion of the zygomaticus major muscle into the zygoma. The zygomatic nerves, in most cases, are found below the zygomaticus major muscle, however, they can also be above.
The platysma muscle presented several ligaments to its posterior fascia. These ligaments were released easily with the repetitive movements of the Trepsat. The section of the platysma inferiorly, approximately 3 to 4cm, helped with its elevation and its suturing at the angle of the mandible.
We elevate the orbicularis oculi muscle, SMAS, and platysma in their entire extension, as a unit. The suture was placed close to the temporal fascia, the fixed SMAS, the angle of the mandible, and the mastoid fascia. After removing the excess skin flap, we observed that the area detached from the face was very small, 1 to 2 cm.
RESULTS
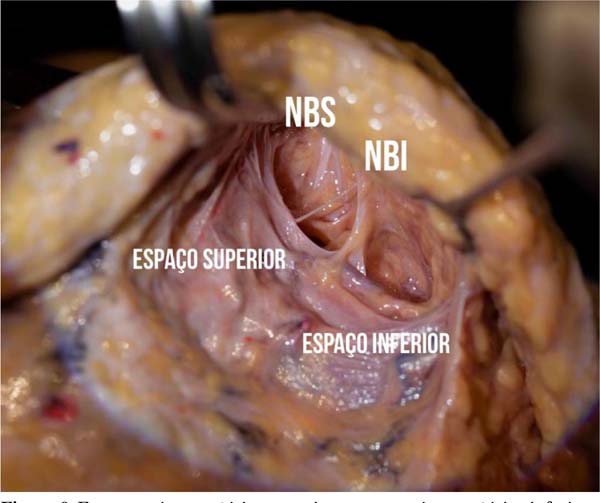
Concerning the anatomical spaces dissected in cadaver specimens, the inferior pre-masseteric space was located over the masseter muscle, considered the floor, and the platysma muscle considered the roof of the space. The posterior part of the space is formed by the platysmal auricular fascia (PAF). The masseteric ligament was in the anterior and superior part of the space and the mandibular ligament was in the anterior lower part. The superior and inferior branches of the mandibular nerve were below the masseter fascia, considered outside the space. The inferior trunk of the buccal nerve traveled along the floor of the space, in a superior direction, below the masseter fascia.
The superior pre-masseteric space was located anterior to the parotid, over the masseter, and superior to the inferior space, between lines 1 and 2. The floor was the masseter muscle and the roof was the SMAS. In this space, the buccal branches of the facial nerve were located, which ran along the floor of the space, below the translucent fascia of the masseter. The upper and lower limits have membranes, where the masseteric ligaments and the upper and lower buccal nerves are located.
The use of Metzembaum scissors in vertical dissection facilitated the rupture of membranes and ligaments, preserving the most posterior nerve branches. The parotid duct was present in all specimens, at the upper limit of the space. The Bichat ball was located in the anatomical parts, anterior to the middle premasseteric space. We noticed the presence of a membrane around the Bichat fat, corresponding to the limits that make up the oral space. The trunks of the superior and inferior buccal nerves were deep, below the masseteric fascia, in the most posterior part of the space.
The nerves move away from the floor in their respective dividing membranes between the spaces, that is, at the upper and lower limits. Once the most anterior part of the space has been reached, both buccal nerve trunks approach the roof of the space (below the SMAS). Each trunk immediately headed towards the innermost part of the respective superior and inferior masseteric ligaments. Each trunk contributed to the interconnection of its various branches immediately below the SMAS, while the upper and lower main trunks continued forward over Bichat’s ball. The superior pre-masseteric space was the space where we found the most diverse anatomical structures, such as ligaments, various nerves, parotid ducts, and accessory parotid lobes (Figures 8, 9 e 10).
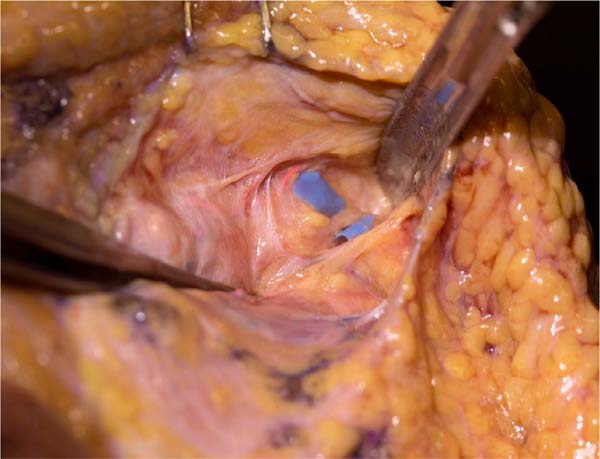
The pre-zygomatic space was shown to be a triangular space, located on the body of the zygoma, narrowing in the medial part, and was accessed by the orbicularis muscle in its lateral part. The roof of the space is the SOOF and orbicularis muscle and the floor contains deep supraperiosteal fat and the origin of the zygomaticus major, zygomaticus minor, and levator labii superioris and nasal ala muscles. The upper limit is the orbicularis retaining ligament and the lower limit is the zygomatic ligaments. In this space, we find the zygomatic branches of the facial nerve and its orbital branches.
Between the pre-zygomatic space and the superior premasseteric space, the zygomatic ligaments were located, strongly adhered to the zygomatic bone. We also found the zygomatic trunk of the facial nerve, with several zygomatic branches. We found the parotid accessory lobe in 3 pieces. The zygomatic trunk was located between the lower border of the zygoma and the accessory lobe of the parotid.
Access to the platysma in the cervical region was made 2cm below the jaw line and 2 to 3cm in front of the anterior border of the sternocleidomastoid, to avoid injuries to the great auricular nerve, external jugular vein and cervical branches of the facial nerve. We found the platysma strongly adhered to the deep cervical fascia and the detachment progressed to the anterior cervical region. The cervical branches of the facial nerve were dissected and were found to exit the parotid gland in its lowest portion, deep close to the sternocleidomastoid. The mandibular marginal branch in some anatomical specimens was single, but in the majority they were double or triple and exited deep to the parotid and followed close and deep to the jaw bone, heading towards the mandibular depression, together with the facial artery and vein.
DISCUSSION
The facial surgery technique has as its important point the SMAS (superficial musculo-aponeurotic system), located between the subcutaneous adipose tissue, called the superficial fat compartment of the face, and the parotid-masseteric fascia. The SMAS located over the parotid is thicker and firmly adhered, through strong ligaments, to the parotid capsule, called fixed SMAS, and difficult to mobilize. The SMAS in the anterior part of the parotid is thinner, poorly adherent, and extends to the medial edge of the zygomaticus major muscle. This SMAS is easily mobilized and considered mobile SMAS. The SMAS continues inferiorly with the platysma and superiorly with the superficial temporal fascia and orbicularis oculi muscle. The most central part of the face does not contain SMAS.
The different facelifting techniques access the SMAS through SMAS flaps, High SMAS, SMAS plication, SMAScectomy, sub-SMAS dissection, or composite flap creations. Each technique accesses the anatomy differently, mobilizing structures in a unique way and promoting satisfactory aesthetic results. However, the mobilization of more central regions of the face was achieved by sub-SMAS or deep plane access techniques, in which the tissues are more easily pulled and repositioned. The safety of preserving structures such as facial motor nerves has become a concern when performing sub-SMAS techniques.
The anatomical spaces of the face are welldefined spaces, with well-defined limits and with loose tissue inside. Each space is defined as a threedimensional structure, with a floor, ceiling, front and back edges, and upper and lower limits, and may or may not have anatomical structures inside. Retaining ligaments such as the zygomatic, mandibular, orbicular, and temporal retaining ligaments, among others, are reference points for the spaces.
The first spaces described by Mendelson were the inferior, middle, and superior premasseteric spaces4. They are avascular and allow access to the movable face. Over the years, other spaces were discussed such as temporal space, preseptal space, prezygomatic space, premaxillary space, and buccal space. The use of these spaces is key to sub-SMAS dissection, however, the need to standardize entry points in the sub-SMAS plane is important to avoid nerve injury. The inferior pre-masseteric space has the masseter muscle as its floor and the roof of the space is made up of the platysma muscle5,6. To make sure we were in the right space, we looked at the masseter muscle fibers, which were vertical, while the platysma muscle fibers were transverse.
Access to the deep plane in cadaver specimens was performed according to our surgical practice and following important steps described by Mendelson7,8. It is important to avoid common mistakes such as entering the parotid, dissecting above the platysma on the face, or opening the masseter fascia and exposing the nerves. Securing the right location prevents nerve damage. Jacono marks the entry incision in the sub- SMAS plane between a straight line from the lateral corner of the eye to the angle of the mandible, extending to the platysma, which in practice is in a location very similar to the technique described by Mendelson1,2,7,8.
The pre-zygomatic space is accessed during our surgeries to treat the middle third of the face and suspend deep fat compartments, such as the SOOF (sub-orbicularis oculi fat) and medial malar (malar fat pad). This space is located on the zygoma bone, below the SOOF and the orbicularis oculi muscle, and progresses to the lateral nasal ala, preserving the zygomaticus major muscle.
Some authors prefer the dissection plane above the orbicularis oculi muscle and below the skin to avoid injury to the zygomatic nerves9,10. However, with cadaver dissection, we noticed that the zygomatic nerves are numerous and most are located deep below the zygomaticus major muscle, where we preserved them. We believe that subcutaneous dissection alone does not release the ligaments and does not correspond to the deep planes.
The concept of facial retaining ligaments and their release for tissue mobilization is mandatory, as some ligaments are extremely firm between the periosteum and the dermis, such as, for example, the zygomatic ligaments. The masseteric, zygomatic, and orbicularis retaining ligaments, including the tear trough ligament, are released to facilitate flap elevation during SMAS plication.
The buccal space, with Bichat’s ball, is medial to the masseter in young patients and is located anterior to the superior pre-masseteric space. However, as already reported by other authors, we noticed that the Bichat ball was found more inferiorly in older patients. The same occurred in some cadaver dissection pieces in our study7,8.
Dissection of the cervical platysma was performed 2cm below the margin of the mandible to avoid damaging the mandibular branches of the facial nerve, which are 5mm from the inferior aspect of the angle of the mandible. However, after dissection of the anatomical parts, we found that the nerves are deeply located below the deep cervical fascia, at the level of the angle of the mandible. The parotid-masseteric fascia is contiguous with the superficial layer of the deep cervical fascia and the mandibular nerves were below this structure11.
The superficialization of the mandibular branches occurred more anteriorly, close to the mandibular ligament, facial artery, and facial vein. In this location on the face, the mandibular nerves are more superficial and are not visualized. This is in line with the safety of the extended cervical plane advocated by Jacono, in which the nerves are deep to the deep cervical fascia9,10.
The subplatysmal detachment occurred up to the anterior part of the neck, but we did not perform the medial opening of the neck on the anatomical specimens. Platysma detachment and traction were performed only through the lateral approach. During surgery, lateral platysmal myotomy and traction were performed with fixation of the platysma to the fascia of the sternocleidomastoid muscle, as we agree with authors who report that medial plication of the platysma reduces the lateral traction force of this muscle by 40%9.
The safety of using blunt detachers and Trepsat confirmed that the nerves were not severed during deep detachment of the face in all spaces accessed during the dissection of anatomical specimens from fresh cadavers. This is in line with articles that evaluate different forms of nerve injuries, such as direct transection of the nerve with a scalpel, nerve injury through the use of cautery and the use of blunt detachers, and analysis of the use of different facelifting techniques, using SMAS flaps or deep planes, demonstrating that the use of blunt detachers presents a minimum chance of nerve transection, as does the sub-SMAS12 technique.
CONCLUSION
The deep plane facelifting or sub-SMAS dissection technique accesses deep planes of the face in well-defined anatomical spaces. Nerve structures and retaining ligaments are closely related to anatomical spaces and
knowledge of this anatomy is essential to avoid nerve injuries. The technique can be reproduced safely, as long as the entry measures into the correct spaces and the use of blunt detachers for dissection in the deep planes of the face are respected.
REFERENCES
1. Mendelson BC, Freeman ME, Wu W, Huggings RJ. Surgical anatomy of the lower face: the premasseter space, the jowl and the labiomandibular fold. Aesthic Plast Surg. 2008;32(2):185-95.
2. Mendelson BC, Wong CH. Surgical anatomy of the middle premasseter space and its application in the sub-SMAS face lift surgery. Plast Reconstr Surg. 2013;132(1):57-64.
3. Wong CH, Hsieh MKH, Mendelson B. The tear trough ligament: an anatomical basis for the tear trough deformity. Plastic Recontr Surg. 2012;129(6):1392-402.
4. Mendelson B, Wong CH. Facelift: Facial anatomy and aging. In: Rubin JP, Neligan PC, eds. Plastic Surgery 4th ed. Volume 2. New York: Elsevier; 2017.
5. O’ Brien JX, Rozen WM, Whitaker IS, Ashton MW. Lore’s fascia and the platysma-auricular ligament are distinct structures. J Plast Reconstr Aesthet Surg. 2012;65(9):e241-5.
6. Mendelson BC, Jacobson SR. Surgical anatomy of the midcheek: facial layers, spaces, and the midcheek segments. Clin Plast Surg. 2008;35(3):395-404; discussion 393.
7. Mendelson BC. Advances in understanding the surgical anatomy of the face. In: Eisenmann-Klein M, Neuhann- Lorenz C, eds. Innovations in Plastic and Aesthetic Surgery. Chapter 18. New York: Springer Verlag; 2007. p. 141-5.
8. Mendelson BC. Surgery of the superficial musculoaponeurotic system: principles of release, vectors, and fixation. Plast Reconstr Surg. 2002;89(3):441-9; discussion 450-1.
9. Jacono AA, Malone MH. The effect of Midline Corset Platysmaplasty on Degree of Face Lift Flap Elevation During Concomitant Deep-Plane Face-lift: A cadaveric study. JAMA Facial Plast Surg. 2016;18(3):183-7.
10. Stuzin JM, Baker TJ, Gordon HL. The relationship of the superficial and deep facial fascias: relevance to rhytidectomy and aging. Plast Reconstr Surg. 1992;89(3):441-9; discussion 450-1.
11. Furnas DW. The retaining ligaments of the cheek. Plast Reconstr Surg. 1989;83(1):11-6.
12. Viterbo F. Improved blunt dissectors for greater safety in face lift surgery. Plast Reconstr Surg. 2013;131(5):858e-859e.
1. Consultório particular, Curitiba, PR,
Brazil
Corresponding author: Daniele Pace Rua Albino Silva, 80, Bom Retiro, Curitiba, PR, Brazil. Zip code: 80520-210, E-mail: danielepace@hotmail.com


















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter