

Articles - Year 2003 - Volume 18 -
Mastopexy Associated with Inclusion of Mammary Prostheses
Mastopexia Associada à Inclusão de Prótese Mamária
ABSTRACT
The authors describe the association of mastopexy and inclusion of silicone implants in 17 patients. The major indication is for hypoplastic breasts with slight or moderate ptoses, and adequate skin texture. The authors describe the surgical technique emphasizing access routes. They review the advantages and disadvantages of the association and conclude that although periareolar mastopexy scar retouching may be necessary, results are generally gratifying.
Keywords: Hypoplastic breasts; breast ptosis; breast implants; periareolar mastopexy
RESUMO
Os autores descrevem a associação de mastopexia e inclusão de prótese de silicone em 17 pacientes.
A principal indicação reside nas hipomastias com ptoses pequenas ou moderadas, com pele de boa textura.
Descreveram a técnica cirúrgica dando ênfase às vias de acesso. Fizeram uma revisão sobre as vantagens e desvantagens dessa associação e concluíram que, apesar da possibilidade de retoque na cicatriz da mastopexia periareolar, os resultados em geral são muito gratificantes.
Palavras-chave: Hipomastia; ptose mamária; prótese mamária; mastopexia periareolar
Breast implants have generally presented satisfactory results, regardless of the access route, dissection plane and characteristics of the prosthesis. Whenever ptosis accompanies hypoplastic breasts, results are conversel less predictable.
The association of hypoplastic breasts and breast ptosis is quite common, especially after pregnancy, after reduction marrunaplasry, and also in breasts called tuberous by Rees{1). For these cases, breast augmentation with silicone implants alone does not result in favorable aesthetic results and may to the contrary accentuate ptosis, while mastopexy allows for the adequate positioning of the areolar-papillary complex - APC, while keeping the breast cone relatively small.
In 1960, Gonçalves-Ulloa (2) mentioned using aloplastic material in association with mastopexy for the first time. On the other hand, in 1969, Goulian and Conway(3), recommended mastopexy at a first stage and silicone implant afterwards for hypoplastic breasts associated with ptosis.
The objective of the present study is exclusively to show the advantages and disadvantages of mastopexy associated with silicone implants for hypoplastic breasts with slight ptosis.
CASES
From November 1998 to August 2000, 17 patients were submitted to mastopexy and silicone gel breast implants in order to correct hypoplastic breasts associated with breast ptosis. The average evaluation period was 14 months, ranging between 7 and 26 months. Patients' ages ranged from 18 to 51 years, with an average of 35 years.
The most frequent causes of small breast volumes associated with ptosis were: post-pregnancy involution with skin flaccidity, sequelae of reduction mammaplasty and tuberous breasts.
Surgical management basically consisted of mastopexy associated with silicone implants, in a single stage, utilizing the region de-epithelized by mastopexy as the access route (Figs. 1 and 2).

Fig. 1 - Decortication, inclusion of implant and periareolar pouch suture.

Fig. 2 - Inclusion of implant through a vertical incision.
Periareolar mastopexy was the most frequently performed technique, with 10 cases (58.8%), and mastopexy with a vertical or anchor-shape scar was performed in 7 cases (41.2%). For anchor-shape scar cases, the technique utilized was similar to that described by Peixoto(4), except for gland resection.
For the periareolar technique we make a circle, above 3 cm in diameter, around the areola, and then perform periareolar decortication. Detachment of glandular tissue of the lower hemisphere is followed by the implant in the retromuscular or retroglandular plane, according to greater or lesser coverage of the implant. Pexis of glandular tissue is performed with absorbable sutures (vicryl 3.0) and the complex is repositioned, by resection of excess periareolar skin. Once vacuum drainage is finished, exiting through the lateral portion of the inframammary sulcus, closure is performed by means of a pouch suture with absorbable sutures (vicryl 2.0) as to better accommodate excess skin.
Mastopexy with a vertical or anchor-shape scar is left for cases in which skin flaccidity does not allow reasonable periareolar accommodation.
RESULTS
Results were considered satisfactory for 14 cases (Figs. 3 to 12), two in which results were below expectations, due to widening of the areolar-papillary complex diameter. In both cases patients were submitted to surgical correction, resulting in a high level of satisfaction for both the patient and surgeon. However, in 3 cases of periareolar mastopexy, residual ptosis was responsible for patients' dissatisfaction. Results are summarized in the table.
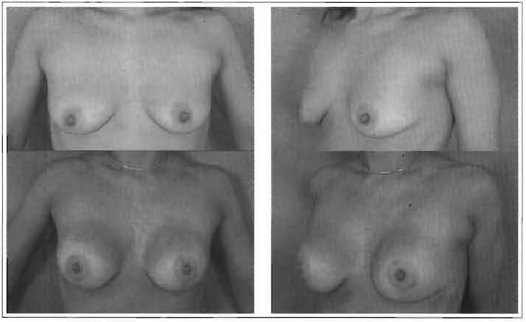
Figs. 3 and 4 -35 years old, 180 ml, retroglandular implant.
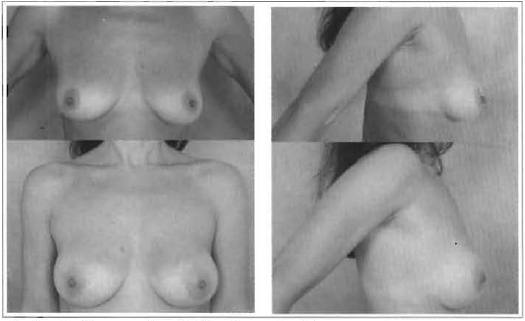
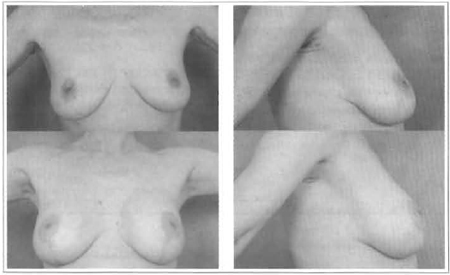
Fig. 5 and 6 - 30 years old, 200 ml, retroglandular implant.
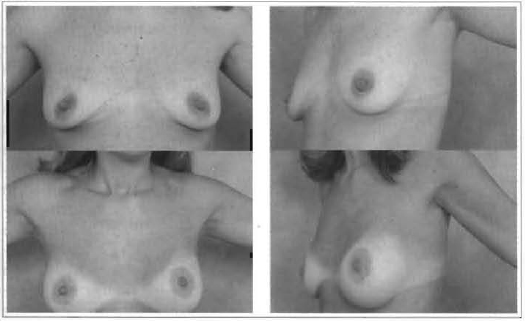
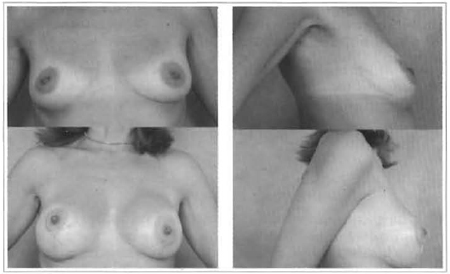
Fig. 7 and 8 - 37 years old, 240 ml, retroglandular implant.
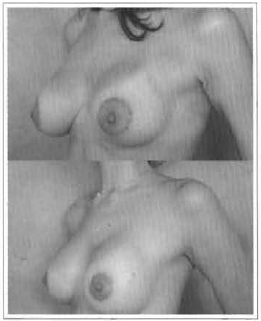
Fig. 9 - APC widening and correction 8 months after implant.
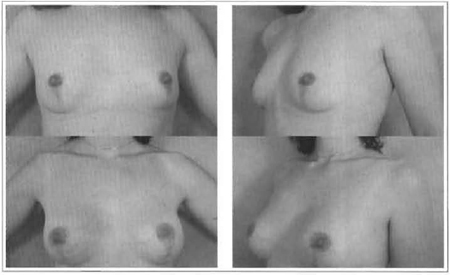
Fig. 10 and 11 - 30 years old, 220 ml, retroglandular implant.
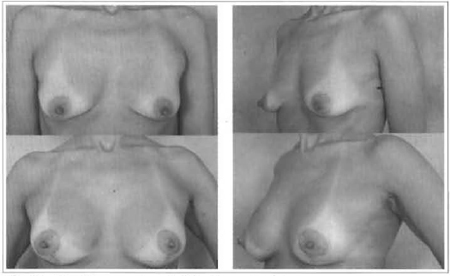
Fig. 12 and 13 - 42 years old, 180 ml, retroglandular implant.
The association of pexis and implants provided adequate volume and shape for treating sequelae of reduction mammaplasty.
The postoperative follow-up of periareolar mastopexy showed progressive improvement of periareolar folding and of breast cone flattening in initial weeks, on average in 4. APC, however, may increase in diameter and sometimes demand re-intervention.
Access through mastopexy with the vertical or anchor-shape scar technique has proved to be the most adequate technique for cases with a more pronounced ptosis, despite the larger than conventional scar for placing the implant.
Persistent ptosis due to excessive skin flaccidity occurred in those cases in which implants were introduced through the periareolar route for patients who refused the vertical or anchor-shape scar mastopexy, making it difficult to correct during the late postoperative period (Figs. 13 and 14).
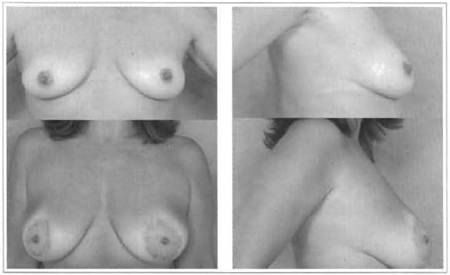
Fig. 14 and 15 - 32 years old, 180 ml, retroglandular implant.
Retouching of areola widening was performed on average, after 8 postoperative months, using the pouch suture performed with non-absorbable sutures. Results have been satisfactory up to 3 months after reintervention (Figs. 15 and 16).
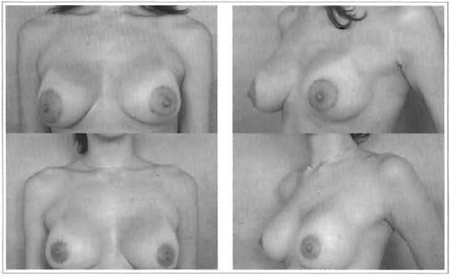
Figs. 16 and 17 - APC widening and correction 8 months after implant.
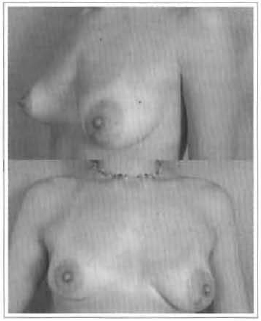
Fig. 18 - 26 years old, to be corrected.
Figs. 19 and 20 - 44 years old, 160 ml, retroglandular implant.
Figs. 21 and 22 - 35 years old, 180 ml, retroglandular implant.
DISCUSSION
As already observed by Chem(5), the excess skin of moderate ptoses needs an inverse T incision. The literature review suggests that ptosis in breasts to be submitted to implants implies the association of some form of pexis, given that the implant alone tends to accentuate ptosis(6,7,8,9) .
We have preferably adopted mastopexy with a vertical or anchorshape scar, or periareolar mastopexy similar to that of Fuente and Martin(10). Both techniques allow for adequate correction of ptosis with vertical or anchor-shape scars that provide an excellent access route for dissection of the logia, especially if assisted by an optic fiber. In cases in which the small volume is due to excessive resection in a previous reduction mammaplasty, the technique of choice for mastopexy should take into account the preexisting scar.
Mastopexy, partially provides the desired shape and projection, thereby allowing for the utilization of a smaller implant (between 160 and 220 ml). Changing absorbable to non-absorbable sutures for the periareolar pouch, as described by Fuente and Martin(10), has solved the widening of APC during the late postoperative period.
CONCLUSION
The disadvantages result from the fact that the definite outcome is later in periareolar mastopexy, due to the flattening of the breast cone and periareolar skin folding in the first weeks, in addition to the possible residual ptosis and increase in the areolar-papillary complex diameter, the last two of which are causes for re-intervention.
Simultaneous implementation of breast augmentation and mastopexy is a rational solution for the hypoplastic and ptotic breast, as it results in a balanced endpoint with less morbidity and lower cost, and a high level of satisfaction and fewer complications.
REFERENCES
1. Rees TD, Aston SJ. The tuberous breast. Clin Plast Surg. 1976; 3:339-40.
2. Gonzales-Ulloa M. Correction of hypotrophy of the breast by means of exogenous material. Plast Reconstr Surg. 1960; 25(1):15-40.
3. Goulian DJr., Conway H. Correction of the moderately ptotic breast. Plast Reconstr Surg. 1969; 43(5):478-80.
4. Peixoto G. Reduction mammaplasty. A personal technique. Plast Reconstr Surg. 1980; 69(2) :21722.
5. Chem RC. Plastica mamaria estetica de aumento com a utiliza utilização de próteses. Rev Soc Bras Cir Plast. 1991; 6(1/2):28-32.
6. Regnault P The hypoplastic and ptotic breast: a combined operation with prosthetic augmentation. PJast Reconstr Surg. 1966; 37(1):31-7.
7. Owaley Jr J. Simultaneous mastopexy and augmentation for correction of the small, ptotic breast. Ann Plastic Surg. 1979; 2(3):195-200.
8. Becker H, van Leeuwen JB. The correction of breast ptosis with the expander mamary prosthesis. Ann Plast Surg. 1990; 24(6):489-97.
9. Chekkoury IA, Roilier C, Leller P, Wilk A. Ann Chir Plast Esthetic. 1991; 36(2):116-9.
10. de la Fuente A, Martin del Yerro JL. Periareolar mastopexy with mammary implants. Aesth Plast Surg. 1992; 16(4):337-41.
I - Professor at Faculdde de Medicina da Universidade de São Paulo (USP) and Senior Member of SBCP.
II - Member of SBCP.
Address for correspondence:
Fabio Rosa Carramaschi, MD
R. Viradouro, 63 Cj. 112
04538-110 -São Paulo -SP Brazil
Phone: (55 11) 3168-3355 -Fax: (55 11) 3168-6583
e-mail: fe.plastic@terra.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter