

Articles - Year 2001 - Volume 16 -
Hemodilution in the Surgical Treatment of Pressure Sores
Hemodiluição Aplicada ao Tratamento Cirúrgico das Escaras de Decúbito
ABSTRACT
The normovolemic hemodilution is one of the various methods available to reduce (or to abolish) the use of homologous blood during elective surgeries. Ten patients with pressure sores had plastic surgery without the need for allogeneic blood transfusion using this autotranfusion modality. After removal of a concentrated blood unit into a common collection bag, a quick infusion of isotonic solution in the proportion 4:1 is carried out up to hematocrit equal to or lower than 30% inducing oligohemia. Consequently, blood lost during surgery has lower erythrocyte concentration, reducing spoliation and getting an improved tissue oxygenation. The blood collected is replaced at the end of intervention. The indications are those of an homologous transfusion or, at least, when it would be judicious to make a preoperative storage. The proposed method was considered equivalent to homologous transfusion in the cases operated, with the advantages of easy performance, no need for refrigeration, and no need for laboratorial tests before transfusion. In additum, the risk of immunological reactions and hematogenic transmission of infectious diseases is abolished.
Keywords: Hemodilution; autotranfusion; homologous transfusion; blood transfusion
RESUMO
A hemodiluição normovolêmica é um dos vários métodos existentes que visam a diminuir ou abolir o uso de sangue homólogo em cirurgias eletivas. Dez pacientes portadores de escaras de decúbito foram submetidos a tratamento de suas feridas com retalhos de vizinhança, sem necessidade de reserva de sangue pré-operatória, ou transfusão homóloga per-operatória, usando essa modalidade de autotransfusão. Após removida uma unidade de sangue concentrado, em uma bolsa usual de coleta, faz-se uma infusão rápida de soluções isotônicas na proporção de 4 por 1, até um hematócrito igualou menor que 30%, induzindo uma oligoemia. Conseqüentemente, o sangue perdido durante a cirgia tem menor concentração de hemácias, reduzindo a espoliação, e obtendo uma melhora da oxigenação tecidual. O sangue coletado é reposto ao final da intervenção. As indicações para a sua realização seriam as mesmas de uma transfusão homóloga, ou pelo menos quando fosse prudente fazer uma reserva pré-operatória. O método proposto foi considerado equivalente à transfusão homóloga nos casos operados, com as vantagens da facilidade de execução, do fato de dispensar refrigeração e exames laboratoriais pré-transfusionais, além de eliminar o risco de reações imunológicas e de transmissão de doenças infecciosas de origem hematogênica.
Palavras-chave: Hemodiluição; autotransfusão; transfusão homóloga; transfusão sangüínea
Blood autotranfusion is an old practice that was almost abandoned when homologous transfusions became simpler and easier to be carried out(1). The increasing freguency of complications related to homologous blood, mainly the risk of viral disease transmission, led to retaking previous methods and stimulated the search for new alternatives.
Hemodilution is an autotranfusion modality introduced by Messmer(2) in 1972. It has gained growing importance as investigators began to deeply study it and its use in diverse medical specialties has increased (general and cardiovascular surgery, gynecology and obstetrics, urology, orthopedics, anesthesia, hematology). The proposed procedure is based upon welldefined pathophysiologic procedures (3). The circulating volume is more important than hematocrit in maintaining hemodynamic stability, as well as the tissue oxygenation up to the limit of 20% hematocrit (4). Compensatory mechanisms are put into action, such as the increased blood flow, the capacity of oxygen extraction, and the decrease of oxygen affinity for hemoglobin, making its release to tissues easier(5,6). The 30% rate was shown to be that with a better level of oxygen transference(7)
The viscosity decrease and the transient volume increase caused by hemodilution lead to an increased cardiac output, venous return, and peripheral vascular resistance, thus increasing blood flow and improving vital organ, skin, and muscle perfusion(5,8,9).
Oligohemia arising from hemodilution decrease preoperative spoliation proportional to the decrease in hematocrit. The final objective is the decreased use of homologous transfusion in patients with pressure sores.
PATIENTS AND METHOD
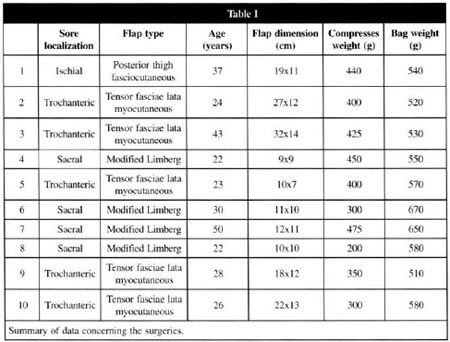
During a 2-year period, 10 pressure sore patients underwent a plastic surgery for their wounds using fascia and microcutaneous (fascia lata tensor muscle) flaps, with no need for preoperative blood storage or homologous transfusion (Table I). In the 6 paraplegic patients only sedation was reguired. The procedure was carried out under general balanced anesthesia in 3 cases and under epidural anesthesia in one case, all patients with normal skin sensitivity.
Blood collection was carried out immediately before or soon after the beginning of anesthesia. We employed the 500-ml bag commonly used by blood banks. After blood collection isotonic solutions (0.9% saline solution, Ringer) were infused in the proportion of 4:1, based on the collection bag weight, aiming to reduce hematocrit to levels between 27% and 30% and only then surgery was started. The remaining fluid replacement followed the usual standards for major surgeries. The collected blood was kept at the operating room up to the transfusion time at the end of surgical procedure.
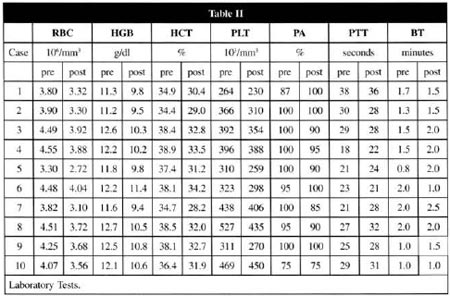
Laboratory assessment of the method included complete blood count (erythrocyte count - HM, hemoglobin - Hgb and hematocrit - Ht) and tests to evaluate coagulation (platelet count- PLT, prothrombin activity - PA, partial thromboplastin time - PTT, bleeding time - BT), performed immediately before and after hemodilution and three days after surgery when hemodynamic stability was established.
The size and type of flaps, the weight of discarded compresses, and clinical parameters (blood pressure, continuous eletrocardiography) as well as the use of indwelling catheter were considered preoperative parameters (Table I). Patients' weight, when required, was estimated by approximation.
All patients received 100 mg of iron daily for 2 months after surgery.
RESULTS
The maximum collection period of time was 15 minutes. The time spent in hemodilution and the time spent in the immediate preoperative preparation were almost the same (approximately 40 minutes). Detectable preoperative blood loss ranged from 300 to 475 ml.
The values of blood pressure, pulse, diuresis, and oxygenation were within the desirable standards. Considering the preset hematocrit range (27% to 30%), clotting factors and platelet count remained within the normal range. In one patient, hemodilution surpassed the planned time, leading to a 22.5% hematocrit with a platelet count variation of 41%, prothrombin activity of 51%, and infinite partial thromboplastin time with no clinically significant changes in clotting or any other disturbance that could interfere in the surgical or anesthetic procedure (case 8).
Laboratorial assessment on Day 3 showed a hemoglobin loss up to 18.9% and normal coagulation tests (Table II).
DISCUSSION
Hemodilution is a widely accepted autotranfusion modality (8,10,11,12). It always aims at avoiding homologous transfusion risks. Among these, one can mention the possibility of hepatitis, AIDS, citomegalic inclusion disease, tripanosomiasis, and malaria transmission, as well as the risk of immunological reactions.
Stored blood has some disadvantages, such as a 2,3- diphosphoglyceric (2,3- DGP) acid loss, which is important for oxygen tissue release, an increase in lactic acid, potassium and ammonia concentration, as well as a loss of coagulation factors V and VIII (5,13,14).
One must remember that the AIDS virus takes 6 months to be detectable by routine tests and also that there is an estimated contamination of one in each 50,000 blood bags(12). Another important data is that approximately 10% transfused people acquire hepatitis(13).
Collected blood for hemodilution may be kept at room temperature for up to 6 hours(15,16) at the operating room, which virtually eliminates the potential risk of loss or container exchange.
The use of colloids or crystalloids is largely discussed. Considering that only 25% of an isotonic solution (crystalloid) volume remain within the intravascular space (3), the volume to be replaced will be 4 times greater than the withdrawn volume if a normovolemic hemodilution is desired. If colloids are used, the volume will be equal to that withdrawn, which requires a larger number of collection bags. Another possibility is the use of both diluents together(15,17).
One must remember that the patient with apressure sore is exposed to the underlying disease, a long hospital stay, previous spoliating surgeries (debridement), and a continuous blood loss through the open wound. For these reasons, this type of patient rarely has a high hemoglobin level and, as a consequence, a preoperative blood storage is desirable. In addition, the receptor graft area preparation generally includes the resection of bone prominences involved in bedsore etiology and this procedure causes a considerable blood loss.
The anemia severity tolerated by an individual has not been established. Levels of 9 g/dl(17), 8 g/dl(4), even 7 g/dl(10,17,18) are accepted by some authors. However, fatigue and morbidity may be considerable in patients with significant acute blood losses, requiring up to 6 weeks for recovery.
The contra-indications for hemodilution are anemia (hemoglobin ≤ 11 g/dl), kidney diseases (because the large volume can not be excreted), severe heart diseases (because the compensatory responses are limited), and low clotting protein concentration(15).
CONCLUSION
Indications of hemotransfusion are multiple and subjective, as well as the desired optimal postoperative hemoglobin levels.
The surgical technique, the use of vasoconstrictors and thermocautery, as well as controlled hypotension are some of the factors that minimize spoliation.
The major objective was the maintenance of a hemoglobin concentration of approximately 10 g/dl on Day 3 after surgery, which was achieved when postdilution hematocrit was between 27% and 30%, with no coagulability change. Even in the case in which the standardized conditions were exceeded, the procedure maintained its efficacy, which shows its safety.
Indications of normovolemic hemodilution are those of a moderate homologous transfusion, or, at least, when a postoperative blood storage is desirable, since both methods are unequivocally similar as for volume replacement with indisputable advantages. It should be used in surgeries for which a hemoglobin reduction below 10 g/dl is expected such as in the treatment of pressure sores.
In conclusion, the procedure is simple and easily performed. It has a favourable cost-benefit ratio and no risk of blood-transmitted diseases or immunological reactions. I can be performed by the surgical team itself and does not require a significant change in the pre-, peri-, and postoperative routine.
REFERENCES
1. BOGOSSIAN L, GONÇALVES MDC, BOGOSSIAN AT. Autotransfusão.J. B. M. 1988; 54: 56-6.
2. MESSMER K, LEWIS L, SUNDER-PLASSMANN L, et al. Acute normovolemic hemodilution. Changes of central hemodynamics and microcirculatory flow in skeletal muscle. Eur. Surg .Res. 1992; 4:55-70.
3. AMARAL JLG, BORDIN JO. Hidratação, reposição volêmica e transfusão. In: AULER JOC. Atualização em Anestesiologia. São Paulo: S.A.E.S.P. 1992; 29: 354-371.
4. HUR SR, HUIZENGA BA, MAJOR M. Acute normovolemic hemodilution combined with Hypotensive anesthesia and other technigues to avoid homologous transfusion in spinal fusion surgery.Spine. 1992; 17: 867-73.
5. MESSMER K. Hemodilurion. Surg. Clin. North America. 1975; 55: 659-78.
6. MESSMER K, GORNANDT L, SINAGOWITZ E. Local tension in tissue of differenr organs during limited hemodilution, Bibliotheca Anat. 1973; 12: 327-32.
7. MARCHIORI C, FEDE A, BASSANO M, et al. Normovolemic hemodilution in head and neck surgery. Arch. Otorhinolaryngol. 1989;246(5):333-5.
8. D'AMBRA MN, KAPLAN DK. Alternatives to allogeneic blood use in surgery: acute normovolemic hemodilution and preoperative aurologous donation. Am.J. Surg.1995; 170: 49S-52S.
9. LAKS H, HANDIN RI, MARTIN V. The effects of acute normovolemic hemodilurion on coagulation and blood utilization in major surgery.J. Surg.Res.1976; 20: 225.
10. NATIONAL INSTITUTES OF HEALTH CONSENSUS CONFERENCE. Perioperative red cell transfusion.JAMA 1988; 260: 2700-3.
11. MANN MC, VOTTO J, KAMBE J, et al. Management of severely anemic patient who refuses transfusion: reasons learned during the care of Jeovah's witness.Ann.lnt.Med.1992; 117: 1042-8.
12. ALMEIDA ME Preoperative normovolemic haemodilution in aesthetic plastic surgery.Aesth. Plast. Surg.1999; 23: 445-9.
13. LAMPE GH. Blood loss and blood transfusion. Acta.Chir. Scand. Suppl. 1989; 550: 89-94.
14. MARTIN E, HANSEN E, PETER K. Acute limited normovolemic hemodilution: a method for avoiding homologous transfusion. World. Surg.1987; 11: 53-9.
15. STEHLIN G L, ZAUD ER HL. Acute normovolemic hemodilution. Transfusion 1991; 31:857-68.
16. BOGOSSIAN L. Autotransfusão programada - pré-depósito. In: BOGOSSIAN L. Manual de Autotransfusão. Rio de Janeiro: Medsi, 1995. v. 3, p.89-116.
17. CAROLI GC, BORGHI B, PAPPALARDO G, et al. Consensus conference. Saving blood: which are still the doubts and the problems? Minerva Anestesiol. 1994; 60: 285-93.
18. KRUSKALL MS. Autologous blood transfusions and plastic surgery Plast. Reconstr Surg.1989; 84: 662-4.
I - Senior Member of Sociedade Brasileira de Cirurgia Plástica.
II - Anesthetist.
III - Associate Member of Sociedade Brasileira de Cirurgia Plástica.
Study performed at Maria de Lourdes Drummond,Mater Dei and Prontocor Hospitals
Address for correspondence:
Marcelo Figueiredo Almeida, MD
Av. do Contorno, 5351 sl. 712
30110-100 - Belo Horizonte - MG
Phone: (55 31) 225-9394


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter