

Original Article - Year 2025 - Volume 40Issue 1
Rate of Orthognathic Surgery Indication in Patients with Complete Bilateral Transforaminal Cleft Treated with the Spina Protocol: A Retrospective Study
Taxa de indicação de cirurgia ortognática em pacientes com fissura transforaminal bilateral completa tratados com o Protocolo de Spina: um estudo retrospectivo
ABSTRACT
Introduction Cleft lip and palate (CLP) is the most common congenital facial deformity, which requires a multidisciplinary and interdisciplinary approach for its management. There is no consensus about the ideal surgical approach of patients with CLP, and the search for the best aesthetic and functional resultmotivates comparisons between different surgical techniques. An important variable that must be analyzed is the impact of the surgical technique on maxillary growth. The aim of this study is to evaluate the rate of orthognathic surgery indication in patients treated with the Spina protocol.
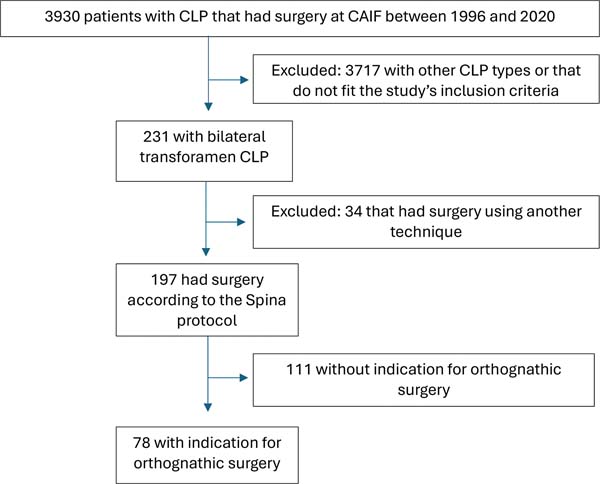
Methods This retrospective study was conducted at an academic tertiary care center in Curitiba, PR, Brazil. A total of 3930 medical records were reviewed from the institution's database, resulting in 231 patients with complete bilateral CLP. Among these, 197 were operated on using the Spina protocol and were included in the study.
Results The literature shows variable rates of orthognathic surgery in patients with complete bilateral transforaminal CLP. In our service, it was observed a 39.59% rate on patients treated according to the Spina protocol. This could be a result ofmany factors, including the surgical technique, since a significant advantage of the Spina protocol is to enable better maxillary growth, because there is less surgical trauma and fewer displacements in the region.
Conclusions The application of the Spina protocol in patients with complete bilateral transforaminal CLP resulted in lower rates of maxillary growth alteration and future need for orthognathic surgery.
Keywords: cleft lip; cleft palate; craniofacial abnormalities; oral and maxillofacial; orthognathic surgery; surgeons
RESUMO
Introdução A fissura labiopalatina (FLP) é a deformidade congênita facial mais comum e seu manejo requer abordagem multidisciplinar e interdisciplinar. Não há consenso sobre a abordagem cirúrgica ideal para pacientes com FLP e a busca pelo melhor resultado estético e funcional motiva comparações entre diferentes técnicas cirúrgicas. Uma variável importante que deve ser analisada é o impacto da técnica cirúrgica no crescimento maxilar. O objetivo deste estudo é avaliar a taxa de indicação de cirurgia ortognática em pacientes tratados com o protocolo de Spina.
Métodos Estudo retrospectivo em um centro acadêmico de atenção terciária em Curitiba, PR, Brasil. Um total de 3.930 prontuários médicos foram revisados no banco de dados da instituição, resultando em 231 pacientes com FLP transforaminal bilateral completa. Dentre estes, 197 foram operados usando o protocolo de Spina e incluídos no estudo.
Resultados A literatura mostra taxas variáveis de cirurgia ortognática em pacientes com FLP transforaminal bilateral completa. Em nosso serviço, foi observada uma taxa de 39,59% em pacientes tratados com o protocolo de Spina. Isso pode ser resultado de diversos fatores, incluindo a técnica cirúrgica, já que uma vantagem significativa do protocolo de Spina é permitir o melhor crescimento maxilar devido ao menor trauma cirúrgico e menos deslocamentos na região.
Conclusões A aplicação do protocolo de Spina em pacientes com FLP transforaminal bilateral completa resultou em menores taxas de alteração do crescimento maxilar e necessidade futura de cirurgia ortognática.
Palavras-chave: anormalidades craniofaciais; cirurgia ortognática; cirurgia plástica; cirurgiões bucomaxilofaciais; fenda labial; fissura palatina; maxila
Introduction
Cleft lip and palate (CLP) is the most common congenital facial deformity, which requires a multidisciplinary and interdisciplinary approach.1 Approximately 1 in every 600-700 live births are affected by CLP, with a higher incidence in males.2 Bilateral CLP occurs in up to 14%3 to 22%4 of cases, with significant variation depending on the reference. Transforaminal clefts, due to complete maxillary disruption, can severely restrict maxillary growth potential, leading to long-term aesthetic repercussions such as the need for orthognathic surgery in adolescence and adulthood.5
Typically, these patients have a compromised maxilla in all three dimensions. It is believed that the alteration in maxillary growth is due to both the initial embryonic defect and the effects of previous surgeries. However, it has been observed that patients with unrepaired CLP can have normal maxillary growth. Therefore, some experts argue that the primary cause of hypoplasia is the formation of scars and contractures resulting from multiple surgeries performed during childhood.6
Patients with bilateral clefts are subjected to various surgical procedures during their treatment, and the extent of scar formation is always a concern regarding maxillary growth. Significant displacements and manipulation of the premaxilla result in deficits in the middle third of the face, leading to hypoplasia and restricted maxillary growth. In cases of bilateral cleft, the maxilla is usually extremely narrow due to medial collapse of the posterior alveolar segments. Clinically, this manifests as a bilateral posterior crossbite. In addition, the premaxilla may be positioned either upward or downward, and often appears protruded.6 This progresses to the need for orthognathic surgery after skeletal maturity.
Various protocols and surgical techniques have been described for treating such patients. Some services advocate for early premaxillary osteotomies, which we believe lead to significant long-term sequelae risks due to the inherent osteotomy induced injury. Many experts agree that disrupting the premaxillary-vomerine suture causes severe midfacial retrusion.7-9 In addition, Bartzela and colleagues10,11 observed in a longitudinal study that premaxillary osteotomy led to unfavorable dental arch patterns.
The Spina Protocol
For over 25 years, our service has utilized the protocol developed in 1966 by a Brazilian surgeon, Professor Victor Spina, for definitive lip treatment and to manage the premaxilla displacement.
This technique advocates for lip adhesion at 6 months old followed by definitive cheiloplasty around the age of 5 years. It is noteworthy that the concept of lip adhesions is not new and dates to Gustav Simon in 1864, who was first to use bilateral labial adhesion to apply posterior traction on the premaxilla.12
Lip adhesion is an initial procedure that brings the edges together without altering the tissue that will be used for the final repair of the cleft lip. The goal is to convert a complete cleft into an incomplete one.13 This procedure helps prepare for the definitive closure, and it applies posterior traction on the premaxilla, which is responsible for its proper positioning. Therefore, lip adhesion substitutes the early premaxillary osteotomies that can lead to restricted maxillary growth, and it is responsible for the management of premaxilla displacement in these patients. This technique is less invasive and, based on our experience, has fewer consequences on the craniofacial growth of these patients. Holdsworth14 also divides the repair of bilateral cleft lip into two stages, although he uses a different technique.
The Spina protocol has two stages, and it is particularly applicable to the bilateral trans-incisive foramen clefts in whom the premaxilla is projecting forward. The first stage converts a complete bilateral CLP into an incomplete bilateral CLP: one side of the cleft is closed in the first few months after birth, while the other side is closed a few months later. The surgery involves a simple incision along the edges of the cleft and the approximation of these edges, preserving the vermilion of the lips margins as much as possible. The orbicularis musculature is not united at this initial stage, and the removal of epithelium from the edges should preserve as much tissue as possible, with minimal displacements and suturing in layers. The aim of this stage is to create optimal conditions for maxillary growth, avoiding excessive pressure on the premaxilla that could result from a tense lip. Between the two stages, the closure of the palate cleft is done. The second stage is the definitive cheiloplasty and it is performed around the age of 5 to 6 years. It involves reopening the lip while preserving the vermilion of the lateral segments. These lateral vermilion flaps are then decorticated and sutured together in the midline, beneath the vermilion of the prolabium, which increases the volume of the prolabial vermilion. Also, the bilateral union of the orbicularis musculature is done.15
Objective
The current study aims to describe the rate of orthognathic surgery indication in patients treated with the Spina protocol at an academic tertiary care center in Curitiba - PR, Brazil, by Dr. Marco Aurélio Gamborgi (in memoriam).
Materials and Methods
This study was performed after obtaining Ethical and Research Committee’s approval. A retrospective analysis was conducted based in medical records of our institution, Centro de Atenção Integral ao Fissurado Labiopalatal (CAIF), located in Curitiba, Brazil. The data was collected between June and August of 2023. The medical records of all 3930 CLP patients in our institution’s database, who underwent surgery by a single surgeon between 1996 and 2020, were evaluated.
Patients diagnosed with complete bilateral transforaminal clefts that were exclusively treated using the Spina protocol were included. Only patients with complete bilateral transforaminal clefts were analyzed, since the Spina protocol is particularly applicable in these patients. Also, variable severity and phenotypical polymorphism make incomplete clefts of the lip and palate impossible to standardize.
Patients who did not initiate treatment at our institution, patients with missing or incomplete medical records and those who were under 15 years old were excluded. This was considered to be a reasonable age to judge the need (or not) for orthognathic surgery since craniofacial growth is complete at this age.
Data regarding the treatment protocol, gender and the need for orthognathic surgery after craniofacial growth completion were collected. The indication or the need for maxillary advancement through orthognathic surgery after craniofacial skeleton maturation was used to indirectly evaluate hypodevelopment of the middle third of the face. Those who had undergone orthognathic surgery or were in the process of presurgical preparation were considered as ’’needing surgery”.
Although we have data from 34 patients who were treated with protocols other than Spina’s, we do not consider it appropriate to gather them into one control group for a comparative statistical study. The reason for this is that the surgical techniques used in these 34 patients were not uniform, which could generate bias. Furthermore, creating subgroups from these 34 patients separating each specific treatment would form very small groups, also making a quality statistical analysis impossible. Therefore, we chose to only describe the rate of orthognathic surgery indication in patients treated with the Spina protocol, which is the technique used in most cases in our service.
However, we must mention some limitations of the study. As it is a retrospective study based on medical record evaluation, some records were worn, incomplete, or even lost, which could compromise a more thorough analysis of the presented data. Due to the long follow-up time of the study, loss to follow-up is inevitable, making it uncertain about the indication of procedures in such patients. Additionally, it is possible that some patients that initially had indication for maxillary advancement for mid-face treatment underwent non-surgical orthodontic compensation.
Results
As can be seen in ►Fig. 1, after reviewing 3930 medical records, 231 patients with complete bilateral transforaminal CLP (5.88%) were identified, already being excluded those who did not meet the study’s inclusion criteria. Among these, 197 patients had surgery using the Spina protocol. Of the 197 patients, 135 (68.53%) were male, and 62 (31.47%) were female. After orthodontic evaluation, 78 (39.58%) of the 197 patients had undergone or had indication for maxillary orthognathic surgery after craniofacial growth completion to correct occlusion and mid-face hypoplasia. Eight of the 197 patients were lost to follow-up, making it not possible to evaluate orthognathic surgery indication.
Based on these data, we present an orthognathic surgery indication rate of 39.59% in patients with complete bilateral transforaminal clefts that underwent surgery using the Spina technique.
Discussion
A significant advantage of the Spina protocol, as described by Professor Victor Spina himself, is to enable better maxillary growth, because there is less surgical trauma and fewer displacements in the region. This causes less scar tissue and avoids excessive pressure on the premaxilla, since there is greater tissue preservation. Furthermore, the Spina technique allows for a more anatomical repair and a deeper gingivolabial sulcus, enabling a more physiological dental rehabilitation and consequently lower rates of maxillary hypoplasia and future need for orthognathic surgery in such patients.
The premaxilla displacement can be managed with the bilateral labial adhesion, which applies posterior traction on the premaxilla. In contrast, performing more invasive procedures, such as setback techniques of the premaxilla characterized by osteotomy and bone resections with posterior repositioning to include the premaxilla in the alveolar arch, poses a significant risk of major sequelae regarding mid-face development due to excessive and traumatic manipulation of the septal area.16
An indirect way to evaluate the interference of surgical treatment on maxillary growth would be to evaluate the need for orthognathic surgery with maxillary advancement. Most studies do not differentiate between types of CLP when publishing their rates of indication for orthognathic surgery, which makes comparative analysis with our rate impossible. Bilateral complete transforaminal fissures are known to be more related to problems concerning the development of the middle third of the face, and it does not make sense to compare such heterogeneous groups. Among those studies that specify the CLP type, the incidence of orthognathic surgery in patients with CLP varies according to the institution and according to the cleft type. For unilateral cleft, a recent study in Canada showed a rate of 48.3% for the need for orthognathic surgery. In the same center, 65% of patients with repaired bilateral cleft underwent orthognathic surgery.17 Another study from Boston Children’s Hospital reported frequencies of Le Fort I osteotomy of 48.5% for patients with complete unilateral CLP and 76.5% for patients with completebilateral CLP.18 Moreover, Vyas et al10 found that 18 of 19 children with bilateral CLP that were treated with their protocol exhibited early occlusal signs of disturbed maxillary growth.
Our study found lower rates, with less than 40% of patients requiring maxillary advancement osteotomies, demonstrating possible benefit from the use of the Spina protocol for patients with complete bilateral CLP. It is important to mention that the Brazilian healthcare system covers the surgery costs, making it accessible to patients regardless of their financial situation. And even with universal access, orthognathic surgery was not necessary in 60% of cases. However, the complexity of the condition and the extent of the variability make it difficult to draw direct inferences regarding maxillary growth.
These data are relevant to the scientific community for several reasons. First, because there is a scarcity of studies in the literature about orthognathic surgery rates in patients with CLP, since, to a certain extent, this rate can lead to judgments about the success or failure of a given institution’s treatment protocol. In addition, the exchange of information about different treatments is essential in the context of still existing divergences regarding the best form of approaching these patients. This does not mean that we want to impose that the Spina protocol is superior to others, but to describe that this technique presented satisfactory outcomes compared with other techniques described in the literature.
Conclusion
The ideal surgical protocol should restore function such as breathing, speech and aesthetics, without jeopardizing growth potential on the involved area. Unfortunately, maxillary hypoplasia and posterior indication for orthognathic surgery are commonly reported worldwide. In our institution, the Spina technique appeared to be a method with lower rates of maxillary growth alterations and future need for orthognathic surgery in patients with complete bilateral transforaminal clefts.
REFERENCES
1. Vieira LVM, Araújo GF, Pinheiro PAL, Albuquerque AFM. Tratamento de paciente com fissura labiopalatina bilateral transforame, utilizando a técnica de setback, associado a técnica de Mulliken: relato de caso. Braz J Case Rep 2022;2(Suppl 2):24. https://doi.org/10.52600/2763-583X.bjcr.2022.2.Suppl.2.24
2. Ribeiro EM, Moreira ASCG. Atualização sobre o tratamento multidisciplinar das fissuras labiais e palatinas. Rev Bras Promoc Saude 2005;18(01):31-40. Recuperado de: https://www.redalyc.org/articulo.oa?id=40818107https://doi.org/10.5020/864
3. World Health Organization. Global strategies to reduce the health care burden of craniofacial anomalies: report of WHO meetings on international collaborative research on craniofacial anomalies. Cleft Palate Craniofac J 2004;41(03):238-243. Doi: 10.1597/03-214.1
4. Sullivan SR, Marrinan EM, LaBrie RA, Rogers GF, Mulliken JB. Palatoplasty outcomes in nonsyndromic patients with cleft palate: a 29-year assessment of one surgeon’s experience. J Craniofac Surg 2009;20(Suppl 1):612-616. Doi: 10.1097/SCS.0b013e318192801b
5. Miachon MD, Leme PLS. Surgical treatment of cleft lip. Rev Col Bras Cir 2014;41(03):208-214. Doi: 10.1590/s0100-69912014000300013
6. Roy AA, Rtshiladze MA, Stevens K, Phillips J. Orthognathic surgery for patients with cleft lip and palate. Clin Plast Surg 2019;46(02): 157-171. Doi: 10.1016/j.cps.2018.11.002
7. Pruzansky S. The growth of the premaxillary-vomerine complex in complete bilateral cleft lip and palate. Tandlaegebladet 1971;75 (12):1157-1169
8. Friede H, Pruzansky S. Longitudinal study of growth in bilateral cleft lip and palate, from infancy to adolescence. Plast Reconstr Surg 1972;49(04):392-403. Doi: 10.1097/00006534-197204000-00005
9. Heidbuchel KL, Kuijpers-Jagtman AM, Freihofer HP. An orthodontic and cephalometric study on the results of the combined surgical-orthodontic approach of the protruded premaxilla in bilateral clefts. J Craniomaxillofac Surg 1993;21(02):60-66. Doi: 10.1016/s1010-5182(05)80149-0
10. Bartzela T, Katsaros C, Rønning E, Rizell S, Semb G, Bronkhorst E, et al. A longitudinal three-center study of craniofacial morphology at 6 and 12 years of age in patients with complete bilateral cleft lip and palate. Clin Oral Investig 2012;16(04):1313-1324. Doi: 10.1007/s00784-011-0615-y
11. Bartzela T, Katsaros C, Shaw WC, Rønning E, Rizell S, Bronkhorst E, et al. A longitudinal three-center study of dental arch relationship in patients with bilateral cleft lip and palate. Cleft Palate Craniofac J 2010;47(02):167-174. Doi: 10.1597/08-249_1
12. Vyas RM, Kim DC, Padwa BL, Mulliken JB. Primary premaxillary setback and repair of bilateral complete cleft lip: indications, technique, and outcomes. Cleft Palate Craniofac J 2016;53(03): 302-308. Doi: 10.1597/14-099
13. Mulliken JB, Schmidt AG. Gustav Simon’s band and the evolution of labial adhesion. J Craniofac Surg 2013;24(01):108-114. Doi: 10.1097/SCS.0b013e318270fe4d
14. Holdsworth WG. Later treatment of complete double clert. Br J Plast Surg 1963;16:127-133. Doi: 10.1016/s0007-1226(63)80093-4
15. Spina V. The advantages of two stages in repair of bilateral cleft lip. Cleft Palate J 1966;3:56-60
16. Spina V. A proposed modification for the classification of cleft lip and cleft palate. Cleft Palate J 1973;10:251-252
17. Daskalogiannakis J, Mehta M. The need for orthognathic surgery in patients with repaired complete unilateral and complete bilateral cleft lip and palate. Cleft Palate Craniofac J 2009;46 (05):498-502. Doi: 10.1597/08-176.1
18. Good PM, Mulliken JB, Padwa BL. Frequency of Le Fort I osteotomy after repaired cleft lip and palate or cleft palate. Cleft Palate Craniofac J 2007;44(04):396-401
1. Hospital do Trabalhador, Centro da Atendimento Integral ao Fissurado Labiopalatal
(CAIF), Curitiba, Paraná, Brasil
Address for correspondence Beatriz Marcomini Arantes, MD, Hospital do Trabalhador, Centro da Atendimento Integral ao Fissurado Labiopalatal (CAIF), Curitiba, Paraná 81050-000, Brasil, (e-mail: bia.marcomini@hotmail.com marcomini@ufpr.br).
Article received: September 22, 2024.
Article accepted: March 24, 2025.
Conflict of Interest
The authors have no conflict of interest to declare.




 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter