

Review Article - Year 2025 - Volume 40Issue 1
Efficacy of Pectoralis Nerve Block in Postoperative Pain Control in Breast Surgeries: Literature Review
Eficácia do bloqueio de nervo peitoral no controle da dor pós-operatória em cirurgias mamárias: Revisão bibliográfica
ABSTRACT
Introduction Proper postoperative pain management in breast surgeries reduces complications, improves patient comfort, and decreases opioid use. Pectoralis nerve (PECS) blocks I and II are effective peripheral analgesic techniques in this context, promoting hemodynamic stability and faster recovery. The present article reviews the literature on PECS block efficacy in breast surgery analgesia and its relationship with reduced opioid use.
Materials and Methods We performed a systematic search in the PubMed database using the keywords breast surgery, pectoral nerve block, and opioid use. We included clinical trials published from January 2016 to April 2023 in Portuguese, English, and Spanish on the effects of PECS blocks I and II in breast surgeries, with a focus on pain control, opioid use, antiemetic requirements, length of hospital stay, and associated complications. We selected 14 articles after applying the eligibility criteria.
Results The PECS blocks demonstrated superior postoperative analgesia and reduced opioid use compared to general anesthesia or other interfascial blocks. They also resulted in lower rescue analgesia requirements and fewer complications.
Conclusion The PECS blocks are an effective strategy for postoperative pain management in breast surgeries, reducing opioid use and its adverse effects, while promoting better patient recovery.
Keywords: analgesia; breast; opioid analgesics; pain; postoperative pain
RESUMO
Introduction Proper postoperative pain management in breast surgeries reduces complications, improves patient comfort, and decreases opioid use. Pectoralis nerve (PECS) blocks I and II are effective peripheral analgesic techniques in this context, promoting hemodynamic stability and faster recovery. The present article reviews the literature on PECS block efficacy in breast surgery analgesia and its relationship with reduced opioid use.
Materials and Methods We performed a systematic search in the PubMed database using the keywords breast surgery, pectoral nerve block, and opioid use. We included clinical trials published from January 2016 to April 2023 in Portuguese, English, and Spanish on the effects of PECS blocks I and II in breast surgeries, with a focus on pain control, opioid use, antiemetic requirements, length of hospital stay, and associated complications. We selected 14 articles after applying the eligibility criteria.
Results The PECS blocks demonstrated superior postoperative analgesia and reduced opioid use compared to general anesthesia or other interfascial blocks. They also resulted in lower rescue analgesia requirements and fewer complications.
Conclusion The PECS blocks are an effective strategy for postoperative pain management in breast surgeries, reducing opioid use and its adverse effects, while promoting better patient recovery.
analgesia; breast; opioid analgesics; pain; postoperative pain
Introdução O controle adequado da dor pós-operatória em cirurgias de mamárias reduz complicações, melhora o conforto do paciente e diminui o consumo de opioides. Os bloqueios do nervo peitoral (pectoralis nerve, PECS, em inglês) I e II são técnicas analgésicas periféricas eficazes nesse contexto, pois promovem estabilidade hemodinâmica e recuperação mais rápida. Este artigo revisa a literatura sobre a eficácia do bloqueio PECS na analgesia para cirurgia de mama e sua relação com a redução do uso de opioides.
Materiais e Métodos A base de dados PubMed foi sistematicamente pesquisada utilizando os descritores cirurgia mamária, bloqueio de nervo peitoral e consumo de opioide. Foram incluídos ensaios clínicos publicados entre janeiro de 2016 e abril de 2023, em português, inglês e espanhol, que avaliaram o efeito dos bloqueios PECS I e II em cirurgias mamárias, considerando controle da dor, uso de opioides, necessidade de antieméticos, tempo de internação e complicações. Após aplicação dos critérios de elegibilidade, 14 estudos foram selecionados.
Resultados O bloqueio PECS demonstrou superioridade na analgesia pós-operatória e redução do consumo de opioides quando comparado a anestesia geral e a outros bloqueios interfasciais, além demenor necessidade de analgesia de resgate emenores taxas de complicações.
Conclusão O bloqueio PECS é uma estratégia eficaz no controle da dor pós-operatória em cirurgias mamárias, pois reduz a necessidade de opioides e seus efeitos adversos, o que favorece a recuperação do paciente.
Palavras-chave: analgesia; dor; dor pós-operatória; mama; analgésicos opioides
Introduction
Pain results from a set of sensory, cognitive, emotional, autonomic, and behavioral organic responses. It is an essential part of the postoperative evolution. Poorly-controlled pain can trigger cardiovascular, metabolic, respiratory, gastrointestinal, urinary, and immunological abnormalities.1
In thoracic surgeries, pain, as well as other organofunctional disorders, hinders deep breathing, increases extracellular fluid, decreases lung compliance, and causes hypoventilation and hypoxemia, which can lead to atelectasis and respiratory infections. Therefore, postoperative pain control is a critical factor in patient recovery, postoperative morbidity and mortality, and quality of life.2
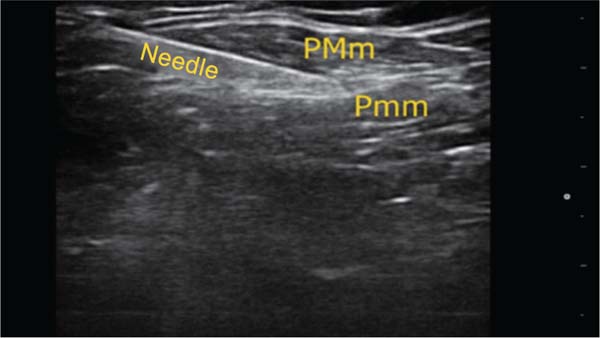
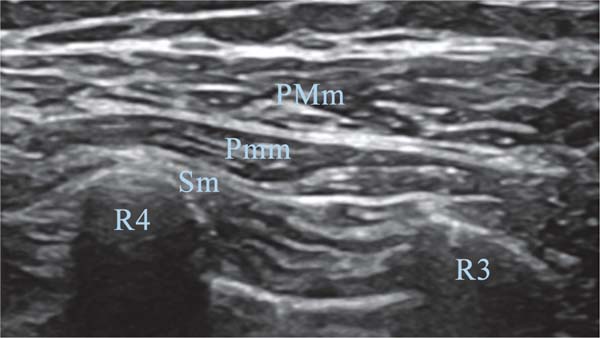
Pain control after breast surgery often uses opioids. These drugs frequently cause adverse events, including nausea, vomiting, sedation, pruritus, paralytic ileus, and urinary retention. These adverse events are uncomfortable for the patient and can increase the length of hospital stay. For better analgesic outcomes after breast surgery, combined with the benefit of reduced opioid use, peripheral analgesic blockshave been performed on the nerves responsible for innervating the pectoral muscles, such as the pectoralis nerve (PECS) block.3,4 The name of the technique depends on the block site. A block with local anesthesia injected only between the pectoralis major and minor muscles consists of a PECS I block (►Fig. 1). With the addition of an anesthetic injection between the pectoralis minor and the serratus anterior muscles, the technique receives the name of PECS II block (►Fig. 2).5,6
For the PECS I block, each site receives a bilateral injection of a 10-mL solution of local anesthetic (levobupivacaine, ropivacaine, or bupivacaine) diluted to a 0.25% concentration. For the PECS II block, also known as modified PECS block, in addition to the aforementioned administration, a volume of 20 mL of the same solution is injected between the pectoralis minor and serratus muscles. These two procedures block the medial and lateral pectoral nerves and the lateral cutaneous branches of the thoracic intercostal nerves.2,7
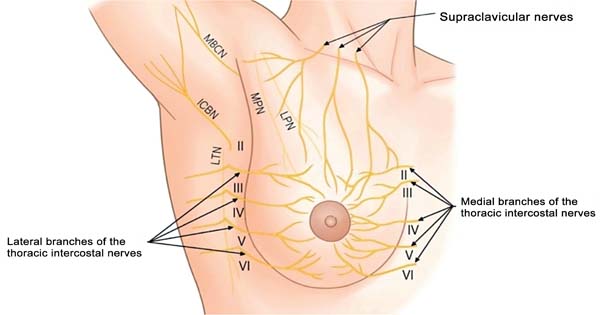
For better postoperative pain control, blocks of the peripheral nerves responsible for breast innervation are under study. These procedures block the supraclavicular nerves, lateral branches of the thoracic intercostal nerves, and medial branches of the thoracic intercostalnerves (►Fig. 3). These studies aim to provide greater postoperative comfort with better pain control, contributing to reduced opioid use and, as a result, decrease the complication rate from opioids and the length of hospital stay.6,8,9
It is worth noting that, as the breast tissue has several nerves, it is unfeasible to block all of them. Moreover, the painful stimulus depends on the surgical technique. Therefore, there may be significant variation in postoperative pain control depending on the type and performance of breast surgery.8,9
Therefore, the present article aims to review the literature on PECS I and II blocks for postoperative pain control in patients undergoing breast surgery and to evaluate the need for rescue opioids for pain control.
Materials and Methods
We performed a literature review in the PubMed database using the following Health Sciences Descriptors (Descritores em Ciências da Saúde, DeCS, in Portuguese) and Medical Subject Headings (MeSH): breast surgery, pectoral nerve block, and opioid use. We used the Boolean operators AND and OR for search refinement per the query strategy.
We included clinical trials published from January 2016 to April 2023, in Portuguese, English, and Spanish that evaluated the effects of PECS I and II blocks in breast surgeries. The outcomes analyzed included postoperative pain control, opioid use, antiemetic requirement, length of hospital stay, and block-associated complications.
The initial search identified 29 articles. After applying the eligibility criteria, we selected 14 clinical trials for the final analysis. The exclusion criteria were studies that did not specifically address the PECS block or that associated it withotherregional blocks(n ¼ 10), articles not about breast surgical procedures (n ¼ 2), and studies that did not evaluate the PECS block for postoperative pain control (n ¼ 3).
Two independent reviewers performed the study selection and solved disagreements by consensus. We used the Jadad scale to assess the methodological quality of the clinical trials, considering randomization, blinding, and description of losses to follow-up.
Results
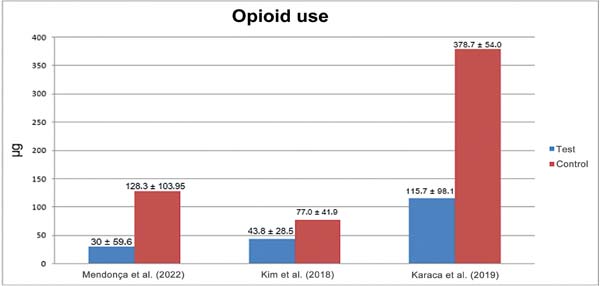
Kim et al.6 (2018) reported that the PECS II resulted in higher opioid use in the control group than in the block group (mean: 77.0 ± 41.9 μg versus 43.8 ± 28.5 μg respectively; p < 0.001), which indirectly resulted in lower blood pressure and heart rate variability (►Fig. 4).6
Karaca et al.3 (2019) observed similar results, reporting lower opioid use during 24 hours in patients who underwent PECS compared to the control group (mean: 115.7 ± 98.1 µg versus 378.7 ± 54.0 µg respectively; p < 0.001), and a shorter hospital stay (24.4 ± 1.2 hours versus 27.0 ± 3.1 hours respectively; p < 0.001) (►Fig. 4).
Consistently, Najeeb et al.10 (2019) compared the pain control provided by the PECS with a control group not undergoing a peripheral nerve block. Immediately after the end of surgery (hour 0), the mean pain score was of 1.05 ± 1.63inpatientsundergoingthePECS,and of 2.42 ± 2.17 in the control group (p <0.001). These findings were reinforced by the significantly lower pain scores in the test group during the first 24 hours postoperatively (0.32 ± 0.87 versus 1.52 ± 1.85; p<0.001), with a similar pattern observed in the other evaluations performed throughout the period.
In addition to the excellent postoperative pain control, Mendonça et al.2 (2022) observed that only 23.3% of patients undergoing PECS block required intraoperative fentanyl, compared with 83.3% in the control group (relative risk [RR]¼0.28; 95% CI: 0.14 -0.54; p¼0.0002). The mean fentanyl administered was also significantly lower in the test group (30±59.6 μg)comparedtothecontrolgroup(128.3±103.95μg; p<0.001), representing an approximately four-fold reduction.
Regarding block performance before or after surgery, Ciftci et al.5 (2021) divided patients into 3 groups: the first underwent a preoperative PECS I block, before surgical incision; the second underwent a PECS I block after the end of surgery; and the third received no block (control group). The authors monitored the patients from the first to the 24th hours postoperatively using the visual analog scale (VAS) for pain. The findings5 showed better pain control in the first group throughout the studied period than in the control group (p < 0.001). The second group did not present better pain control in the first hour after surgery compared to the controls, but presented reduced pain at the 24-hour assessment (p <0.001).5
Discussion
Since the description of the PECS block technique in 2011, several studies, such as those herein cited, have demonstrated its broad benefits. The outcomes show reduced opioid use in the postoperative period, which indirectly reflects better pain control, leading to greater patient comfort not only in terms of pain, but also in reduced blood pressure and heart rate variability. In addition, there was a significant decrease in the number of opioid side effects.2,11
The question about the best time to perform the block (before, during, or after surgery) is answered by Ciftci et al.5 (2021), who showed better pain control throughouttheperiodevaluatedwhenthe block was performed before the surgical incision. Despite this, it is worth emphasizing that the block also showed benefits when performed after surgery compared with patients who did not receive it, once again clarifying the benefit of the technique.5,12
Najeeb et al.10 (2019) reaffirmed this finding when analyzing the numerical pain scale (NPS), showing the important postoperative pain control provided by PECS blocks immediately, 30 minutes, 6 hours, 12 hours, and 24 hours after the end of surgery. Patients undergoing PECS presented mean NPS scores at 0, 0.5, 6, 12, and 24 hours of 1.05 ± 1.63, 1.35 ± 1.23, 0.8 ± 1.23, 0.48 ± 0.72, and 0.32 ± 0.87 respectively (p < 0.001), while patients not undergoing the PECS block presented, in the same period, mean scores of 2.42 ± 2.17, 1.90 ± 1.38, 2.25 ± 1.90, 1.70 ± 2.02, and 1.52 ± 1.85 respectively (p < 0.001). An analogous study by Altıparmak et al.13 (2019) found similar results. In addition to better pain control and, consequently, a reduction in opioid use, Mendonça et al.2 (2022) showed a decrease in the mean length of hospital stay, of 41.2 ± 13.4 hours in the group undergoing PECS compared with 45.1 ± 15.4 hoursin the placebo group.
During breast surgery preparation, it is possible to perform several other blocks rather than the PECS block, including the paravertebral thoracic block and the erector spinae muscle block. Martsiniv et al.14 (2020) evaluated and compared these blocks to determine the best alternative for breast surgeries. In a study by Eskandr et al.8 (2022), the PECS block showed better benefits in postoperative pain control, reduced opioid use during and after surgery, and reduced nausea and vomiting. In addition to the benefits regarding postoperative pain control, compared to other regional block techniques, PECS presented a lower risk of complications such as pneumothorax, abscesses, neuritis, local anesthetic toxicity, vascular puncture, and hematomas, which are undesirable complications, especially in surgeries performed in a day hospital setting.8,14
As PECS II blocks provide analgesia in part of the breast and armpit region, Kim et al.6 (2018) reinforced that they can result in excellent postoperative pain control in the first 24 hours in breast surgeries, consistent with Karaca et al.3 (2019) and other studies reporting that the PECS II block, in addition to the excellent effect on postoperative pain control, significantly reduced opioid use and hospital stays.
Given the evidence from these studies, it is critical to encourage the dissemination and implementation of PECS I and II blocks in breast surgeries, since several clinical trials have proven their benefits and superiority in postoperative pain control and, consequently, reduced opioid use, lower risks inherent to the procedure, and greater patient comfort, results that lead to shorter hospital stays.6,7
Conclusion
The current review demonstrated that PECS I and II blocks provide effective postoperative pain control in breast surgeries, significantly reducing opioid use and its adverse effects and improving hemodynamic stability and patient comfort. The review also showed that preoperative blocks result in better pain control in the first 24 hours after surgery, although the technique also yields benefits when performed after surgery. In addition to pain relief, reduced opioid use is associated with a lower incidence of nausea, vomiting, and other side effects, favoring patient recovery and reducing hospital stay.
Despite the assumption that PECS II blocks would present a better analgesic effect than PECS I blocks because they cover a larger area, the literature analyzed did not prove it. Other variables studied to improve the technique include anesthetic dose, type, and concentration for injection into the block sites, which can increase the duration of pain control. Considering the benefits, we concluded that the implementation of PECS blocks in the clinical practice should be encouraged as part of the multimodal pain management in breast surgeries. Future studies with larger samples and costbenefit analyses may contribute to consolidate this technique as a standard in perioperative analgesia.
References
1. Wang K, Zhang X, Zhang T, Yue H, Sun S, Zhao H, Zhou P.The Efficacy of Ultrasound-guided Type II Pectoral Nerve Blocks in Perioperative Pain Management for Immediate Reconstruction After Modified Radical Mastectomy: A Prospective, Randomized Study. Clin J Pain 2018;34(03):231-236. Doi: 10.1097/AJP.0000000000000529
2. Mendonça FT, Feitosa AdA Junior, Nogueira H, Roncolato H, Goveia CS. Efficacy of type-I and type-II pectoral nerve blocks (PECS I and II) in patients undergoing mastectomy: a prospective randomised clinical trial. Anaesthesiol Intensive Ther 2022;54 (04):302-309. Doi: 10.5114/ait.2022.121096
3. Karaca O, Pınar HU, Arpacı E, Dogan R, Cok OY, Ahiskalioglu A. The efficacy of ultrasound-guided type-I and type-II pectoral nerve blocks for postoperative analgesia after breast augmentation: A prospective, randomised study. Anaesth Crit Care Pain Med 2019; 38(01):47-52. Doi: 10.1016/j.accpm.2018.03.009
4. Wallace CC, Wetzel ME, Howell C, Vasconez HC. The Efficacy of Pectoralis Nerve Blockade in Breast Reductions: A Prospective Randomized Trial. Ann Plast Surg 2021;86(6S, Suppl 5)S632-S634. Doi: 10.1097/SAP.0000000000002763
5. Ciftci B, Ekinci M, Celik EC, Karaaslan P, Tukac İC Ultrasoundguided pectoral nerve block for pain control after breast augmentation: a randomized clinical study. Braz J Anesthesiol 2021;71 (01):44-49. Doi: 10.1016/j.bjane.2020.12.004
6. Kim DH, Kim S, Kim CS, Lee S, Lee I-G, Kim HJ, et al. Efficacy of Pectoral Nerve Block Type II for Breast-Conserving Surgery and Sentinel Lymph Node Biopsy: A Prospective Randomized Controlled Study. Pain Res Manag 2018;2018:4315931. Doi: 10.1155/2018/4315931
7. Aarab Y, Ramin S, Odonnat T, Garnier O, Boissin A, Molinari N, et al. Pectoral Nerve Blocks for Breast Augmentation Surgery: A Randomized, Double-blind, Dual-centered Controlled Trial. Anesthesiology 2021;135(03):442-453. Doi: 10.1097/ALN.0000000 000003855
8. Eskandr A, Mahmoud K, Kasemy Z, Mohamed K, Elhennawy T. A comparative study between ultrasound-guided thoracic paravertebral block, pectoral nerves block, and erector spinae block for pain management in cancer breast surgeries. A randomized controlled study. Rev Esp Anestesiol Reanim (Engl Ed) 2022;69 (10):617-624. Doi: 10.1016/j.redare.2022.02.004
9. Zhang Z, Li Z, Zhang Z, Guan X, Xin M. Analgesic Efficacy of Pectoral Nerve Blocks in Implant-Based Mammoplasty: A Systematic Review and Meta-Analysis. Aesthetic Plast Surg 2023;47 (01):106-115. Doi: 10.1007/s00266-022-03135-8
10. Najeeb HN, Mehdi SR, Siddiqui AM, Batool SK. Pectoral Nerves I, II and Serratus Plane Blocks in Multimodal Analgesia for Mastectomy: A Randomised Clinical Trial. J Coll Physicians Surg Pak 2019;29(10):910-914. Doi: 10.29271/jcpsp.2019.10. 910
11. Hoerner E, Gasteiger L, Ortler M, Pustilnik V, Mathis S, Brunner C, et al. The impact of dexamethasone as a perineural additive to ropivacaine for PECS II blockade in patients undergoing unilateral radical mastectomy - A prospective, randomized, controlled and double-blinded trial. J Clin Anesth 2022;77:110622. Doi: 10.1016/j.jclinane.2021.110622
12. Lanier ST, Lewis KC, Kendall MC, Vieira BL, Oliveira GD Jr, Nader A, et al. Intraoperative Nerve Blocks Fail to Improve Quality of Recovery after Tissue Expander Breast Reconstruction: A Prospective, Double-Blinded, Randomized, Placebo-Controlled Clinical Trial. Plast Reconstr Surg 2018;141(03):590-597. Doi: 10.1097/ PRS.0000000000004104
13. Altıparmak B, Korkmaz Toker M, Uysal Aİ, Turan M, Gümüş Demirbilek S. Comparison of the effects of modified pectoral nerve block and erector spinae plane block on postoperative opioid consumption and pain scores of patients after radical mastectomy surgery: A prospective, randomized, controlled trial.JClinAnesth2019;54:61-65.Doi:10.1016/j.jclinane.2018.10.040
14. Martsiniv VV, Loskutov AO, Strokan MA, Pylypenko MM, Bondar VM. Efficacy of pectoral nerve block type II versus thoracic paravertebral block for analgesia in breast cancer surgery. Klin Onkol 2020;33(04):296-301. Doi: 10.14735/ amko2020296
1. Department of General and Specialized Surgery, School of Medicine, Universidade
Federal Fluminense, Niterói, RJ, Brazil
Address for correspondence Mateus Casotti Colombo, Avenida Marquês do Paraná, 349, Centro, Niterói, RJ, CEP: 24030-215, Brazil (e-mail: mateuscasotticolombo@gmail.com).
Artigo submetido: 30/09/2024.
Artigo aceito: 20/05/2025.
Conflict of Interests
The authors have no conflict of interests to declare.





 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter