

Original Article - Year 2025 - Volume 40Issue 1
Use of Acellular Dermal Matrix in the Treatment of Capsular Contracture after Radiotherapy
Uso de matriz dérmica acelular no tratamento de contratura capsular após radioterapia
ABSTRACT
Introduction In Brazil, breast cancer is the most common neoplasm after nonmelanoma skin cancer. Radiotherapy increases breast reconstruction complications, including severe capsular contracture. Studies indicate that acellular dermal matrix (ADM) can prevent this complication, reducing local inflammation because it is not recognized as a foreign body.
Materials and Methods In the present prospective study, we evaluated patients with breast cancer who underwent mastectomy with immediate reconstruction using silicone implants or expanders and radiotherapy and developed Baker grade-III or -IV capsular contracture, who underwent a new surgery for treatment. We divided the patients into two groups: group 1 (G1) underwent conventional therapy consisting of capsulotomy and fat grafting without ADM, while the treatment for group 2 (G2) involved ADM and fat grafting.
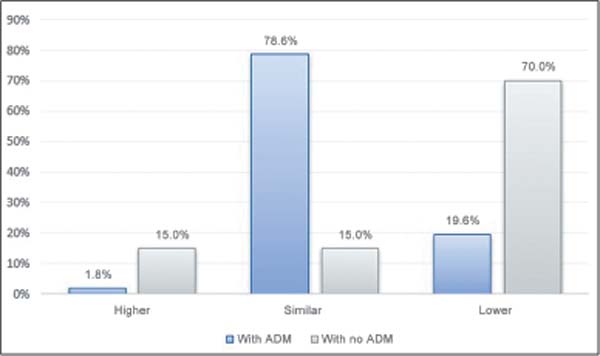
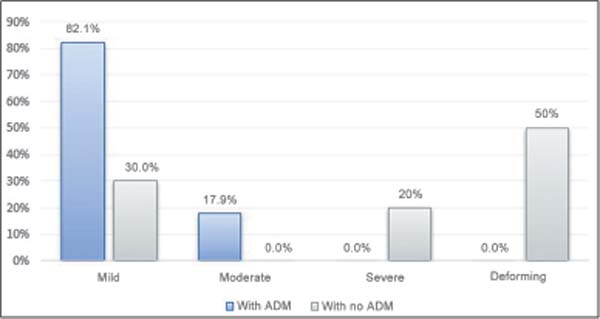
Results The study included 76 patients, 56 in G2 and 20 in G1. The evaluation considered objective (inframammary fold height, nipple-areola complex height, and the number of surgeries) and subjective (volume, consistency, and Baker grade of contracture) measurements of the reconstructed breast compared with the contralateral breast. There were statistically significant differences between the groups. Mild contractures occurred in 82.1% of G2 and in 30% of G1. We observed deforming contractures in 0% of G2 and in 50% of G1 (p<0.001).
Conclusion In patients with postradiotherapy capsular contracture, ADM with fat grafting reduces the lesion and provides better esthetic and functional outcomes compared with the conventional treatment with capsulotomy and fat grafting.
Keywords: acellular dermis; breast neoplasms; implant capsular contracture; mammaplasty; radiotherapy
RESUMO
Introdução No Brasil, o câncer de mama é o mais incidente após o câncer de pele não melanoma, e a radioterapia aumenta as complicações na reconstrução mamária, como a contratura capsular grave. Estudos indicam que a matriz dérmica acelular (MDA) pode prevenir essa complicação, ao reduzir a inflamação local por não ser reconhecida como corpo estranho.
Materiais e Métodos Neste estudo prospectivo, foram avaliados pacientes com câncer de mama, submetidas a mastectomia com reconstrução imediata utilizando implantes de silicone ou expansores, que realizaram radioterapia e evoluíram com contratura capsular de graus III ou IV de Baker, e submetidas a nova cirurgia para tratamento. As pacientes foram divididas em dois grupos: o grupo 1 (G1), de tratamento convencional com capsulotomia e lipoenxertia sem matriz, e o grupo 2 (G2), de tratamento com MDA associada à lipoenxertia.
Resultados Foram incluídas 76 pacientes: 56 no G2 e 20 no G1. A avaliação considerou medidas objetivas (altura do sulco mamário, altura do complexo areolopapilar e número de cirurgias) e subjetivas (volume, consistência e contratura segundo Baker) da mama reconstruída em relação à mama contralateral. Houve diferenças estatisticamente significantes entre os grupos. No G2, 82,1% das pacientes apresentaram contratura leve, e no G1, 30%, ao passo que contraturas deformantes ocorreram em 0% no G2 e em 50% no G1 (p<0,001).
Conclusão O uso da MDA associado à lipoenxertia no tratamento de contratura capsular após radioterapia reduz a contratura capsular e proporciona melhores resultados estéticos e funcionais em comparação ao tratamento convencional com capsulotomia e lipoenxertia.
Palavras-chave: ontratura capsular em implantes; derme acelular; mamoplastia; neoplasias da mama; radioterapia
Introduction
Plastic surgery is a unique specialty with no precise definition and a long and contradictory history of tradition and innovation. It encompasses reconstructive and esthetic surgeries, and, in many cases, these areas are inseparable. The best example of this indivisibility may be breast reconstruction in patients who have undergone mastectomy due to breast cancer.
In all regions of Brazil, breast cancer is the most common neoplasm in women after non-melanoma skin cancer. The South and Southeast are more developed regions and present higher rates than the North region of Brazil. For each year from 2023 to 2025, there are an estimated 73,610 new cases, representing an incidence of 41.89 cases per 100 thousand women (INCA, 2022).1
Breast cancer treatment has evolved as a result of largescale clinical trials, becoming increasingly individualized and less mutilating. Today, most women with breast cancer are candidates for breast-sparing treatment,2 and more patients are undergoing local or systemic adjuvant therapies. The increasing indication of radiotherapy for breast cancer patients has raised the number of complications in breast reconstruction, including local fibrosis, implant extrusion, capsular contracture, and the need for surgical revision.3,4
One of the complications most feared by plastic surgeons is severe capsular contracture. The contracture causes pain, breast stiffening, local anatomy distortion, difficulty in obtaining a satisfactory outcome after another surgical stage of reconstruction, and irreparable esthetic damage.
Recently, radiotherapy was deemed a variable potentially leading to the formation of a pathological capsule.5 A 2009 systematic review6 reported capsular contracture rates in irradiated breasts with tissue expanders or silicone implants of 7.9% and 8.9% respectively. However, in practice, we observe long-term rates higher than 60%. A classic7 study with more than 2 thousand breast reconstructions with implants demonstrated that the rate of Baker III or IV contracture was of approximately 10% in 1 year and higher than 30% in 5 years.
The evolution of radiotherapy devices and irradiation techniques using hypofractionated doses in less time and three-dimensional conformational radiotherapy targeting the tumor area was not enough to eliminate the cellular damage in healthy tissues in postoperative treatment.
Coleman introduced autologous fat grafting in 1893.8 This technique has since been used for a wide range of treatment options in reconstruction and cosmetic surgery. In 2007, Rigotti et al.10 published a successful study on the use of fat grafting in the treatment of postradiotherapy capsular contracture, and this method has become another option in the therapeutic arsenal available for breast reconstruction and its complications.
The basis of this study10 was the theory that adult adipose tissue stem cells had regenerative potential to alleviate the symptoms of severe capsular contracture and increase the volume of the breast compartment. However, this technique has limitations, including unpredictable outcomes, poor response, and recurrence of the contracture. These limitations raise the number of surgeries to improve the success rate.
The first description of acellular dermal matrix (ADM) in breast reconstruction dates from 2001.12 Initially recommended for rippling correction, ADM indication has been expanded to incorporate esthetic and reconstruction aspects.
Recent studies suggest that the dermal matrix can prevent capsular contracture after silicone implant placement. This fact results from the non-recognition of ADM as a foreign body, which reduces the pathophysiological inflammatory process leading to capsular contracture.13,14 In 2010, Komorowska-Timek and Gurtner15 performed an experimental study in animals subjected to ADM-coated silicone implants and radiation. They concluded that ADM undergoes incorporation into the adjacent tissues, decreasing local inflammatory activity.
To date, there are no publications on the use of ADM in the treatment of capsular contracture as a radiation-induced complication.
Objectives
The current study aims to evaluate the outcomes of using ADM and fat grafting in the treatment of severe capsular contracture induced by radiotherapy in the immediate postoperative period of breast reconstruction with implants due to breast cancer, comparing this therapeutic modality with a control group undergoing conventional treatment with capsulotomy and fat grafting.
Materials and Methods
The present prospective study was conducted from 2016 to 2024. The same surgeon performed all procedures at Hospital Daher Lago Sul (HDLS), in Brasília, Brazil. The sample consisted of patients who underwent unilateral or bilateral, partial or total mastectomies due to breast cancer with immediate reconstruction using silicone implants or tissue expanders followed by adjuvant radiotherapy.
We included all patients with grade-III or -IV capsular contracture according to the Baker classification who underwent a new surgery for its treatment, agreed to participate in the study, and signed the informed consent form. We excluded patients who did not complete a postoperative follow-up period of at least 6 months after the second surgery, including photographic documentation.
We randomly distributed the patients into 2 groups: group 1 (G1, the controls) underwent the conventional treatment, that is, capsulotomy and fat grafting but no ADM; and group 2 (G2) underwent treatment with ADM and fat grafting. For each group, we prepared two tables: ►Table 1 shows the demographic data of the sample, and ►Table 2 lists the qualitative data following capsulotomy, fat grafting, and ADM.
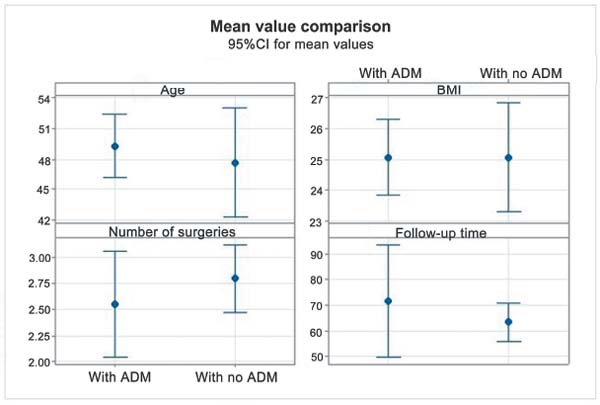
| Group | Mean | Median | Standard deviation | CV | Min. | Max. | N | 95%CI | p-value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | With ADM | 49.3 | 46.5 | 11.7 | 24% | 29 | 77 | 56 | 3.1 | 0.599 |
| Without ADM | 47.7 | 48.5 | 11.4 | 24% | 29 | 71 | 20 | 5.0 | ||
| BMI (kg/m2) | With ADM | 25.07 | 24.80 | 4.55 | 18% | 19.47 | 48.28 | 56 | 1.19 | 0.995 |
| Without ADM | 25.07 | 25.05 | 3.75 | 15% | 20.13 | 32.81 | 20 | 1.64 | ||
| Surgeries (n) | With ADM | 2.55 | 2 | 1.92 | 75% | 1 | 9 | 56 | 0.50 | 0.577 |
| Without ADM | 2.80 | 3 | 0.70 | 25% | 2 | 4 | 20 | 0.30 | ||
| Follow-up (months) | With ADM | 71.77 | 41.5 | 82.20 | 115% | 6.0 | 416.0 | 56 | 21.53 | 0.660 |
| Without ADM | 63.55 | 67.5 | 15.87 | 25% | 35.0 | 87.0 | 20 | 6.95 |
| With ADM (N ¼ 56) | Without ADM (N ¼ 20) | p-value | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
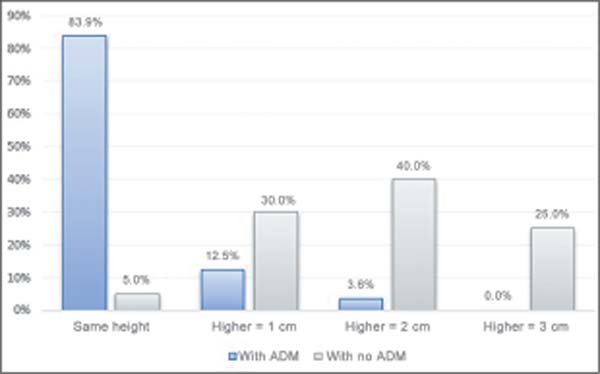
| Inframammary fold height x contralateral breast | Same height | 47 | 83.9% | 1 | 5.0% | < 0.001 |
| 1 cm higher | 7 | 12.5% | 6 | 30.0% | 0.074 | |
| 2 cm higher | 2 | 3.6% | 8 | 40.0% | < 0.001 | |
| 3 cm higher | 0 | 0.0% | 5 | 25.0% | < 0.001 | |
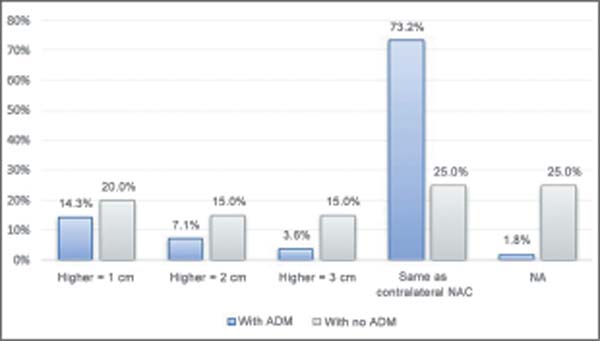
| NAC height x contralateral breast | Same height | 41 | 73.2% | 5 | 25.0% | < 0.001 |
| 1 cm higher | 8 | 14.3% | 4 | 20.0% | 0.547 | |
| 2 cm higher | 4 | 7.1% | 3 | 15.0% | 0.297 | |
| 3 cm higher | 2 | 3.6% | 3 | 15.0% | 0.077 | |
| NA | 1 | 1.8% | 5 | 25.0% | < 0.001 | |
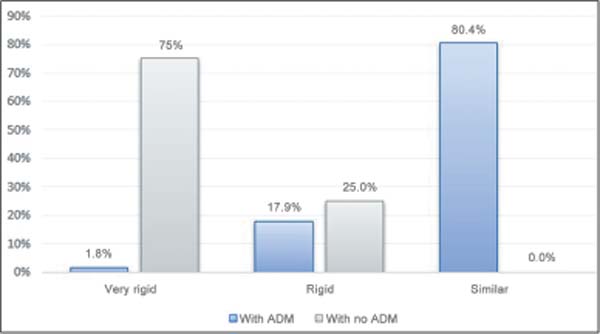
| Consistency | Very rigid | 1 | 1.8% | 15 | 75.0% | < 0.001 |
| Rigid | 10 | 17.9% | 5 | 25.0% | 0.491 | |
| Similar | 45 | 80.4% | 0 | 0.0% | < 0.001 | |
| Contracture | Mild | 46 | 82.1% | 6 | 30.0% | < 0.001 |
| Moderate | 10 | 17.9% | 0 | 0.0% | 0.043 | |
| Severe | 0 | 0.0% | 4 | 20.0% | < 0.001 | |
| Deforming | 0 | 0.0% | 10 | 50.0% | < 0.001 | |
| Volume | Higher | 1 | 1.8% | 3 | 15.0% | 0.023 |
| Similar | 44 | 78.6% | 3 | 15.0% | < 0.001 | |
| Lower | 11 | 19.6% | 14 | 70.0% | < 0.001 | |
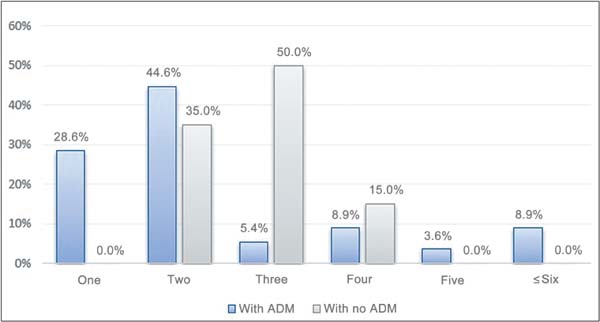
| Number of surgeries | 1 | 16 | 28.6% | 0 | 0.0% | 0.007 |
| 2 | 25 | 44.6% | 7 | 35.0% | 0.453 | |
| 3 | 3 | 5.4% | 10 | 50.0% | < 0.001 | |
| 4 | 5 | 8.9% | 3 | 15.0% | 0.448 | |
| 5 | 2 | 3.6% | 0 | 0.0% | 0.392 | |
| ≥ 6 | 5 | 8.9% | 0 | 0.0% | 0.167 | |
For all patients, we sent a standard authorization request to the health insurance company. Patient allocation into groups was conducted based on the health insurance company’s authorization and agreement to cover ADM-related expenses. Patients with approved coverage requests were included in G2. We adopted this allocation method since ADM is a high-cost material.
Results
This study evaluated 76 patients, 56 in G2 and 20 in G1. The mean ages of the patients in G1 and G2 were of 47.7 and 49.3 years, respectively. There was no difference in the mean body mass index between the groups. The G1 patients underwent a higher mean number of surgeries than the G2 subjects, with no statistically significant difference. The study period ranged from 2016 to the end of 2024. The mean follow-up was of 64 15.87 (minimum: 35; maximum: 87) months for G1, and of 72 82.2 (minimum: 6; maximum: 416) months for G2.
We defined a level of 0.05 (5%) of statistical significance for the present study. We used parametric statistical tests after determining the normal distribution of the quantitative variables of the main outcome using the Kolmogorov-Smirnov test (N < 100). Therefore, the comparison of the mean values of the quantitative factors for G1 and G2 used the Student’s t-test.
Regarding demographic data, there was no statistically significant difference between the groups, meaning that they were homogeneous (►Table 1).
The following comparative graphs of each quantitative variable for both groups show the mean and standard deviation values with 95%CIs.
We evaluated the effectiveness of ADM use through objective and subjective physical measurements distributed as follows: objective – mammary fold height and nippleareola complex (NAC) height, in centimeters, compared with the contralateral breast, and the number of surgeries; subjective – breast volume and consistency compared with the contralateral breast, and contracture according to the Baker classification. We used the Chi-squares test to compare the groups regarding the distribution of the relative frequencies (percentages or prevalence) of the qualitative factors.
►Table 2 shows the results of the relationships and/or associations through absolute values and percentages. The table also reveals the joint distribution of the variables as absolute values and their percentages and all combinations between the two groups.
An analysis of ►Table 2 shows that all factors present at least one response with a statistically significant difference between G1 and G2. For instance, the mild contracture (Baker I) rate was of 82.1% for G2 and of 30% for G1 (p < 0.001). In contrast, the deforming contracture (Baker IV) rate was of 0.0% for G2 and of 50% for G1 (p < 0.001). This same divergence occurs in all other qualitative parameters shown in ►Table 2 and ►Figs. 2–6.
These cases always require surgical treatment. The only surgical option is capsulotomy, since it is not possible to perform capsulectomy after total mastectomy, implant replacement, and fat grafting, especially in patients with more severe and symptomatic conditions. A growing body of clinical evidence strongly supports the therapeutic potential of mesenchymal stem cells to revascularize ischemic tissue and restore function.18 Studies19 have reported that fat grafting is an effective long-term filler material and treatment for contracture and other conditions.
In irradiated tissues, fat grafting decreases collagen content and dermal thickness while increasing tissue vascularization. However, fat graft volume retention is substantially lower. Computed tomography (CT) scans reveals that fat graft survival decreases significantly in irradiated tissues.20 It is estimated that 20 to 40% of grafted fat undergoes resorption, with some cases requiring new injections.21 In practice, these rates are immensely higher, as demonstrated in our previous study.
►Figs. 2–7 show the results for each variable in the comparison between the 2 groups.
Regarding the number of surgeries performed (►Fig. 7), all G2 patients underwent 1 to 2 surgical corrections. The G2 patients who underwent 3 to 4 surgeries had already undergone 2 or 3 unsuccessful attempts at fat grafting for treatment.
Discussion
Radiotherapy for breast cancer is often essential, reducing local recurrence and improving patient survival. However, the negative effects of radiation on tissues trigger shortand long-term complications, including capsular contracture.16
Capsular contracture is one of the main complications in surgeries involving reconstruction with implants (prosthesis and expanders) and radiotherapy. An excessive fibrous capsule forms around the implant, leading to symptoms such as breast stiffness and pain, superomedial displacement of the implant, and complete distortion of its volume and shape.17
The multiple cases of recurrence of severe capsular contracture led to the evaluation of a material that could replace elastic fibers and collagen as a structural base for adipocyte survival and the formation of new tissue to replace the tissue damaged by radiotherapy.
The ADM is a dermal structure consisting of flexible tissue with no antigenic cells due to their elimination by specific chemical processing. This biological skeleton enables cellular repopulation and rapid revascularization of the patient (host), optimizing the surgical outcome. It is produced from human (FlexHD, Alloderm, Allomax, and DermaCell ), pig (Permacol™ and Strattice), or bovine cadavers (SurgiMend), or from bovine pericardium (Veritas).22
The ADM determines local angiogenesis and the organized migration and deposition of fibroblasts and myofibroblasts. As such, it decreases the contracture of normal scar tissue and the capsule around the implant, forming a thinner, less contractile capsule. The ADM also decreases the inflammatory process by inhibiting the transformation of fibroblasts into active myofibroblasts, reducing capsular contracture.23
We started to recommend this treatment protocol to patients who had already undergone conventional treatment and had relapsed in 2016. In 2018, after evaluating the outcomes of patients with multiple relapses, we began to adopt it as a priority treatment protocol for postradiotherapy severe capsular contracture. As ADM is a high-cost material, we used the health insurance company approval as a criterion to allocate the patients into the case and control groups, and the sample presented good homogeneity, as described in the methodology.
For the qualitative study, we selected the main complaints reported by the patients, such as shape, volume, consistency, and height, and their evaluations were objectively parameterized. We demonstrated that most variables presented statistically significant differences in the comparison between G1 and G2, with a highly significant p-values, as shown in ►Table 2.
Individually, each variable demonstrated an interesting behavior of improvement over the years in G2 compared with G1, which showed a worsening of breast consistency during follow-up.
The breast symmetry index was another crucial response in G2. ►Figs. 2–6 reveal that, for all qualitative variables, there was a significant increase in the symmetry in the following aspects: inframammary fold height, NAC position, and affected breast volume and position. In addition, G2 presented an improvement in the Baker contracture classification.
In 2016, Lee and Mun24 published an update article evaluating 23 meta-analyses on the risks and benefits of ADM in breast reconstruction. They concluded that there is no risk of serious complications; however, some variables, such as preoperative chemotherapy and postoperative radiotherapy, can increase these rates.
It is worth emphasizing that there was no increase in the number of complications or reconstruction loss after ADM use. The decrease in the number of surgeries for correction and symmetry improvement was statistically significant, and most patients underwent only one or two procedures to achieve the desired outcome. It is worth noting that symptom improvement requires at least 6 months of follow-up. This improvement was significantly greater in G2, with longer follow-up times, while G1 presented worsening of the condition.
Conclusion
Capsular contracture remains a challenge for plastic surgeons due to its undefined cause, resulting in no definitive absolute or prophylactic treatment. Radiotherapy is a mainstay against breast cancer, but it leads to several tissue changes and is a risk factor for contractures. Although prophylactic ADM resulted in positive outcomes, its therapeutic use in contractures lacks sufficient basis.
The current study concluded that ADM addition to capsulotomy, implant exchange, and autologous fat grafting in the treatment of breast capsular contractures is superior to the previous treatment consisting of capsulotomy, implant exchange, and fat grafting. This new approach generates expectations regarding an issue afflicting all professionals involved in breast cancer treatment and patients who are biopsychosocially affected by the disease.
It is worth emphasizing the need for further studies on the treatment of breast capsular contracture with dermal matrices after radiotherapy, given thelackofspecific scientificevidence.
REFERENCES
1. Instituto Nacional de Câncer (INCA) Incidência: apresenta dados de incidência do câncer de mama no Brasil, regiões e estados. Rio de Janeiro: INCA; 2022. Disponível em: https://www.gov.br/inca/pt-br/assuntos/gestor-e-profissional-de-saude/controle-do-cancer-de-mama/dados-e-numeros/incidencia
2. Instituto Nacional de Câncer (INCA) Estimativa 2020: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2019
3. Sledge GW, Mamounas EP, Hortobagyi GN, Burstein HJ, Goodwin PJ, Wolff AC. Past, present, and future challenges in breast cancer treatment. J Clin Oncol 2014;32(19):1979–1986. Doi: 10.1200/ JCO.2014.55.4139
4. Anker CJ, Hymas RV, Ahluwalia R, Kokeny KE, Avizonis V, Boucher KM, et al. The effect of radiation on complication rates and patient satisfaction in breast reconstruction using temporary tissue expanders and permanent implants. Breast J 2015;21(03): 233–240. Doi: 10.1111/tbj.12395
5. Salzberg CA, Ashikari AY, Berry C, Hunsicker LM. Acellular dermal matrix-assisted direct-to-implant breast reconstruction and capsular contracture: a 13year experience. Plast Reconstr Surg 2016;138(02):329–337. Doi: 10.1097/PRS.0000000000002331
6. Kronowitz SJ, Robb GL. Radiation therapy and breast reconstruction: a critical review of the literature. Plast Reconstr Surg 2009; 124(02):395–408. Doi: 10.1097/PRS.0b013e3181aee987
7. Kim IK, Park SO, Chang H, Jin US. Inhibition Mechanism of Acellular Dermal Matrix on Capsule Formation in ExpanderImplant Breast Reconstruction After Postmastectomy Radiotherapy. Ann Surg Oncol 2018;25(08):2279–2287. Doi: 10.1245/ s10434-018-6549-8
8. Lam TC, Hsieh F, Boyages J. The effects of postmastectomy adjuvant radiotherapy on immediate two-stage prosthetic breast reconstruction: a systematic review. Plast Reconstr Surg 2013; 132(03):511–518. Doi: 10.1097/PRS.0b013e31829acc41
9. Billings E Jr, May JW Jr. Historical review and present status of free fat graft autotransplantation in plastic and reconstructive surgery. Plast Reconstr Surg 1989;83(02):368–381. Doi: 10.1097/ 00006534-198902000-00033
10. Rigotti G, Marchi A, Galiè M, Baroni G, Benati D, Krampera M, et al. Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: a healing process mediated by adipose-derived adult stem cells. Plast Reconstr Surg 2007;119(05):1409–1422, discussion 1423. Doi: 10.1097/01.prs.0000256047.47909.71
11. Papadopoulos S, Vidovic G, Neid M, Abdallah A. Using Fat Grafting to Treat Breast Implant Capsular Contracture. Plast Reconstr Surg Glob Open 2018;6(11):e1969. Doi: 10.1097/GOX.0000000000001969
12. Duncan DI. Correction of implant rippling using allograft dermis. Aesthet Surg J 2001;21(01):81–84. Doi: 10.1067/maj.2001. 113438
13. Stump A, Holton LH III, Connor J, Harper JR, Slezak S, Silverman RP. The use of acellular dermal matrix to prevent capsule formation around implants in a primate model. Plast Reconstr Surg 2009; 124(01):82–91. Doi: 10.1097/PRS.0b013e3181ab112d
14. Basu CB, Leong M, Hicks J. Acellular cadaveric dermis decreases the inflammatory response in capsule formation in reconstructive breast surgery. Plast Reconstr Surg 2010;126:1842–1847. Doi: 10.1097/PRS.0b013e3181f44674
15. Komorowska-Timek E, Gurtner GC. Intraoperative perfusion mapping with laser-assisted indocyanine green imaging can predict and prevent complications in immediate breast reconstruction. Plast Reconstr Surg 2010;125(04):1065–1073. Doi: 10.1097/PRS.0b013e3181d17f80
16. Milanesi L. Impacto da radioterapia em reconstrução mamária tardia com uso de implantes – complicações e revisão de literatura. Rev Bras Cir Plást 2019;34(Suppl 1):150–152. Doi: 10.5935/2177-1235.2019RBCP0078
17. Vinnik Camd. Contratura esférica de Cápsulas Fibrosas ao redor de implantes de mama: Prevenção e Tratamento. Cirurgia Plástica e Reconstrutiva 1976;58(05):555–560
18. Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg 2007;119(03):775–785, discussion 786–787. Doi: 10.1097/01.prs.0000252001.59162.c9
19. Coleman SR. Structural fat grafting: more than a permanent filler. Plast Reconstr Surg 2006;118(3, Suppl)108S–120S. Doi: 10.1097/01.prs.0000234610.81672.e7
20. Garza RM, Paik KJ, Chung MT, Duscher D, Gurtner GC, Longaker MT, Wan DC. Studies in fat grafting: Part III. Fat grafting irradiated tissue–improved skin quality and decreased fat graft retention. Plast Reconstr Surg 2014;134(02):249–257. Doi: 10.1097/ PRS.0000000000000326
21. Feitosa RGF, Araújo RS, Nunes ELF, Isoldi FC, Dotto PG, Gragnani A, Ferreira LM. Lipoenxertia para tratamento de radiodermite após tratamento de câncer de cabeça e pescoço. Rev Bras Cir Plást 2021; 36(01):69–75. Doi: 10.5935/2177-1235.2021RBCP0013
22. Bezerra FJF, Moura RMGd. Tela sintética como potencial alternativa de baixo custo à matriz dérmica em reconstruções mamárias. Rev Bras Cir Plást 2021;36(02):122–128. Doi: 10.5935/21771235.2021RBCP0057
23. Berger Ralf. Avaliação histológica das cápsulas formadas por implantes de silicone texturizados sem e com cobertura por tela de poliéster (PARIETEX): estudo em ratas. [tese (Pós-Graduação em Princípios de Cirurgia)] Curitiba: Instituto Presbiteriano Mackenzie, Faculdade Evangélica Mackenzie do Paraná, Instituto de Pesquisas Médicas; 2020. Disponível em: https://adelpha-api.mackenzie.br/server/api/core/bitstreams/b17c1cc1-1b83-450faa12-3a837a8de271/content
24. Lee KT, Mun GH. Updated Evidence of Acellular Dermal Matrix Use for Implant-Based Breast Reconstruction: A Meta-analysis. Ann Surg Oncol 2016;23(02):600–610. Doi: 10.1245/s10434-015-4873-9
1. Centro de Estudos Daher, Hospital Daher Lago Sul, Brasília, DF, Brazil.
Address for correspondence Marcela Caetano Cammarota, Centro de Estudos Daher, Hospital Daher Lago Sul, SHIS QI 07, Conjunto F, Lago Sul, Brasília, DF, 71615-660, Brazil (e-mail: marcelacammarota@yahoo.com.br).
Article received: December 17, 2024.
Article accepted: March 20, 2025.










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter