

Articles - Year 2001 - Volume 16 -
Capsulectomy without Capsulotomy for Treating Capsule Contractures
A Capsulectomia sem Capsulotomia no Tratamento das Contraturas Capsulares
ABSTRACT
The increase in the utilization of silicone breast implants for reconstruction and cosmetic purposes, has led to a great deal of discussion as to the possible complications resulting from their presence in the body. Some ofthe problems are related to the fibrous capsule (capsule contracture) and/or to the patient's immunologic response. The authors propose the utilization of an easily approachable technique for changing or removing breast implants, by removing-the capsule and implant in one piece, the so-called "capsulectomy without capsulotomy." The objective of the study is to describe the procedure in detail, showing its advantages and risks and correlate data with the pertinent literature.
Keywords: Breast implants; capsulectomy; augmentation mammaplasty; capsule contractures
RESUMO
Com o crescente aumento do uso de implantes mamarios de silicone para fins estéticos e reparadores, muito se tem discutido a respeito das possíveis complicações resultantes da sua presença no organismo, sendo que alguns desses problemas encontram-se relacionados à capsula fibrosa (contratura capsular) e/ou à resposta imunológica do paciente. Os autores propiõem o emprego de uma abordagem de fácil execução técnica nas situações de troca ou retirada de próteses mamárias, removendo cápsula e implante em monobloco, a chamada "capsulectomia sem capsulotomia". 0 objetivo do estudo é detalhar o procedimento, evidenciar suas vantagens e riscos e correlacionar os dados com a literatura pertinente.
Palavras-chave: Implantes mamários; capsulectomia; mamoplastia de aumento; contratura capsular.
As the utilization of breast implants became more popular over the last decade, the insertion of implants, whether for cosmetic purposes or for reconstruction, became an increasingly routine procedure. It is estimated that in Brazil, 25,000 of these surgeries were performed in 1999, with silicone being the material used in most of the procedures. This trend led to a more intense discussion of the risks and complications due to silicone gel implants. Many studies printed in international literature focus on the different aspects of the relationship between the body and silicone. An important part of the discussion focused on the aspects related to the fibrous capsule: its development, biological behavior and, mainly, its surgical mangement in situations in which it becomes pathological. Some of these studies focus on the effects due to the presence of silicone in the body and the possible immunologic responses to it(1).
The objective of the present study is to join both concepts (capsule pathology and risks due to the presence of silicone) by reviewing the known aspects as reported in the literature, proposing the utilization of a tactical approach that is being employed with satisfactory results at the Instituto de Cirurgia Plastica Santa Cruz: the removal of the capsule along with the implants in one piece ("capsulectomy without capsulotomy"), as a feasible alternative for situations in which implant removal or substitution is necessary, with advantages and disadvantages over conventional approaches.
SURGICAL TECHNIQUE AND CASE REPORTS
After routine pre-operative preparation, patients with silicone gel breast implants who, for different reasons, needed to undergo surgery to substitute or definitely remove the implants were submitted to the technique under general anesthesia in the surgical center. The surgical approach begins with a larger incision on the previous scar; the planes are separated until the fibrous capsule is reached. At this point rhomboid dissection of the capsule is performed, using scissors to avoid bursting. After the capsule-implant set is removed in one piece, vigorous electro cauterization is used to stem wound blood flow and a new silicone implant mayor may not be inserted. Routine suction drainage and raphe by wound planes are employed.
In recent years, this has been the usual approach used in our Service for removing or substituting breast implants for cosmetic or reconstruction purposes.
Two cases are presented as examples:
Case 1: M.L.H., 43 years old, female, Caucasian patient, with smooth texture silicone gel implants, inserted in the anterior muscular plane for thirteen years. The patient had a Baker Grade III capsule contracture. The patient's complaints began after the implants had been inserted: upper limb pain (mainly in arm pits) and muscular pains. The patient was submitted to implant and capsule removal using the technique described, without inserting new implants. The postoperative period evolved without complications and the symptoms lessened three weeks after the surgical procedure.
Case 2: D.S., 46 years old, female, Caucasian patient, with textured silicone implants that had been inserted four years before, after being submitted to immediate right breast reconstruction and a myocutaneous flap of the greater dorsal, due to ductal carcinoma. Three years later the patient presented Baker Grade IV capsule contracture (Fig. 1). The implant was then replaced, using the technique described above, evolving well (Figs. 2 to 5). Pre-operative symptoms were myalgia and hair loss that improved after capsule removal.
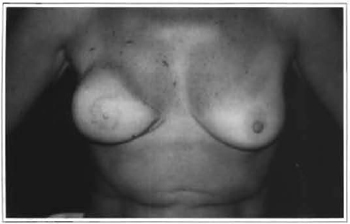
Fig. 1 -Baker Grade IV capsular contracture in the right breast.
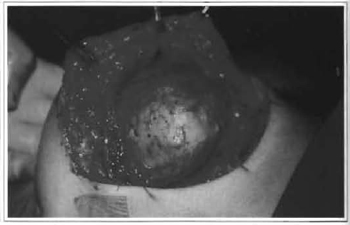
Fig. 2 -Capsulectomy without capsulotomy (intra-operative).
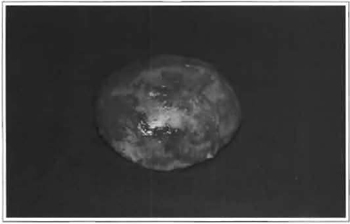
Fig. 3 -Intact fibrous capsule with silicone implant.

Fig. 4 -Incision of the fibrous capsule showing the implant inside.
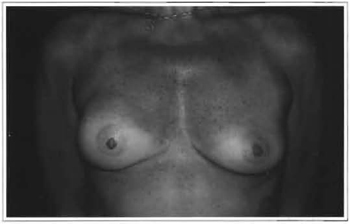
Fig. 5 -Last post-operative period (14 months).
DISCUSSION
Over the past few years, the use of breast implants has grown markedly, both for medical and cosmetic or reconstruction purposes. So far, the most commonly used material in such insertions has been silicone gel implants. No polyurethane implants have been used in this study and we do not know its effect on the formation of the capsule, nor on its removal, as it is not standard practice in our facility. However, as it is alloplastic material inserted in the body, implants may cause many complications related either to their own insertion or to the organic response triggered by their presence.
These complications have already been described as the result of the use of silicone implants, and some of them are still controversial today (Table I).
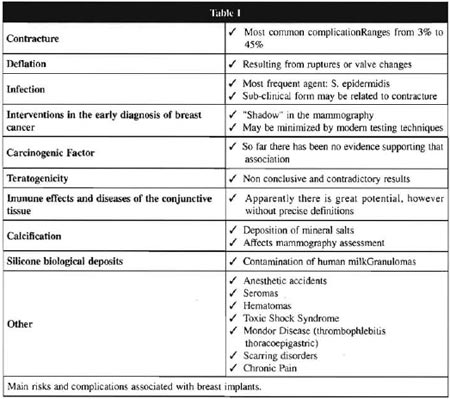
Fibrous capsules are formed around the implant as an immunologic reaction to the foreign body in an attempt to isolate it from the surrounding tissue. How ever, in about 10% to 20% of cases(2) silicone may reach the capsule and even go beyond it, towards the breast tissue. Several studies have been conducted on capsule histology, but most of them indicate common features: presence of fibrous scar, histiocytic response, gigantic cells, metaplasia and heterotopic calcifications(3) .
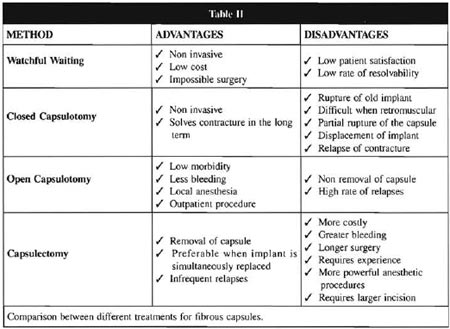
Most authors regard capsule contracture as the most frequent complication, reaching 45% in one of the studies(2). A few factors may be related to the development of such contractures, including sub-clinical infections, hematomas, silicone extravasation, type and texture of the implant and position of the implant(4). The mechanism for the contracture, however, has yet to be fully established. We know that the intensity of the capsular contracture is related to the thickness of the fibrous capsule. The therapeutic approach for capsular contracture includes the following alternatives: closed or open capsulotomy, capsulectomy, in addition to watchful waiting. The advantages and disadvantages of each one of these techniques are summarized in Table II.
In 1981, Hakme described very high rates of complications associated to closed capsulotomy in patients with silicone implants(5).
There is already consensus as to the leaking of silicone into adjacent tissues. However, the mechanisms through which such migrations take place are not yet clear, and they are not the result of the rupture of the implant. Evidence of silicone has been found inside the breast parenchyma, in the galactophore ducts, in axillary lymphnodes and, particularly, in the fibrous capsule(6). According to some authors, such leaking may be related to the emergence of autoimmune manifestations, both at the clinical and laboratory levels.
Autoimmune manifestations have been extensively described in a number of studies which associated the presence of implants to changes such as pain and joint rigidity, paresthesia in the extremities, fatigue, myalgia, hair loss, fever, excessive sweating, lower limb edema, memory loss, gastrointestinal complications, and others(7), in addition to a few symptoms that would fit into the diagnosis of fibromyalgia. Laboratory findings also included the presence of antinuclear antibodies, anticollagen(8) and antimacrophage CD68, in addition to an increase in the speed of blood sedimentation. In spite of these clinical and laboratory data (most of them non-specific), the so-called "silicone disease" has never been conclusively proven. In some patients these manifestations may be totally or partially alleviated by the simple removal of the implant(9), which seems to indicate a possible cause and effect relationship. Considering the findings of clinical improvement following the removal of the implants, as well as the proven presth ence of silicone in the capsule, the most sensible option in these situations, taking into account the diferent techniques, seems to be the removal of the capsule with the implant in one piece (capsulectomy without capsulotomy). In 1976, Carvalho and Baroudi(10) already defended the complete resection of the capsule when there was capsuto lar contracture.
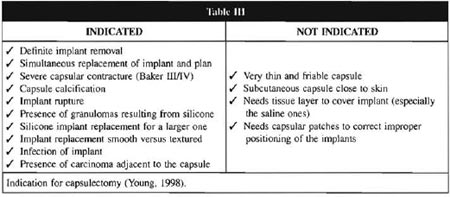
In 1998, Young(7) established the guidelines for capsulectomies, as well as the instances when they are not recommended (Table III). However, in our view, it could be more widely indicated, considering that technically speaking, this approach does not present any major difficulties (when done by experienced professionals), as the implant itself serves as the base and reference for the dissection of the plane between capsule and breast tissue. On the other hand, a new intervention for isolated capsulectomy presents much greater difficulties and risks. Moreover, removal of the capsule, which means removing a considerable amount of silicone, the role of which is yet to be determined, may contribute to the improvement or disappearance of the autoimmune manifestations. Rockwell(9) et al.(1998) provided evidence of that in their study, in which patients with persistent systemic symptoms even after the isolated removal of the implants presented improvement when the capsule was extirpated.
It is worth mentioning that, once patients were made aware of the risks and benefits of this procedure as compared to the isolated removal of the implant, almost all the patients preferred removal of the implant along with the capsule. This information is supported by literature findings, and a few authors
suggest that patients who undergo capsulectomy and implant replacement will present rates of contracture again similar to that of the patients with primary surgery(11, 12).
Therefore, based on our experience, we chose to expand our indications for capsulectomy, using the one-piece approach in practically all cases of replacement or final removal of the implants in which there were no definite obstacles to the indication for the procedure. We did not observe an increase in morbidity with this procedure, but just a slight augmentation in the size of the incision that the technique requires. When performed by a well-trained surgical team, it did not present relevant technical difficulties. This has led us to regard it as the first choice in the management of periprosthetic fibrous capsules in our facility.
CONCLUSIONS
Supported by the experience acquired in the several cases our team followed, and comparing them with the data published in international literature in recent years, the authors have drawn the following conclusions:
1. The use of silicone implants for cosmetic and/or reconstruction purposes, althougth widespread, is not a procedure free of riscks or complications, some of which are still subject to controversy.
2. In the manifestations related to autoimmune reactions, which may occasionally occur in implants bearers, the relevance of the presence of silicone in the fibrous capsule should not be undervalued.
3. Comparing the different choices for treating the capsule, it has been observed that all of them present similar risks. However, capsulectomy is the only one that permits an apparently complete removal of the silicone content.
4. Before suspected or confirmed silicone leakage, the one-piece removal of the capsule and implant (capsulectomy without capsulotomy) seems to be the safest procedure, avoiding greater dissemination of silicone particles through adjacent tissues. However, it has been proven that silicone may leak even without macroscopic rupture of the implant pocket.
5. Capsulectomy without capsulotomy, in skilled hands, was a good surgical choice for the replacement or final removal of breast implants, with low morbidity rates and without technical difficulties. This requires, however, a larger incision than the conventional technique.
6. In our view, these reasons contribute to a broader indication of one-piece capsulectomy for the management of fibrous capsules in breast implants.
REFERENCES
1. AMERICAN SOCIETY OF PLASTIC AND RECONSTRUCTIVE SURGEONS. The Removal of Silicone Gel-Filled Brest Implants and Capsulectomies at Pacients. New York, 1994.
2. KASPER CS. Histologic Features of breast capsules reflect surface configuration and composition of silicone bag implants. Am. J. Clin. Pathol. 1994; 102:655-60.
3. COPELAND M, et al. Systemic inflammatory disorders related to fibrous breast capsules after silicone implant removal. Plast. Reconstr. Surg. 1993; 92:1179-84.
4. FOOD & DRUG ADMINISTRATION. Letter for further information on breast implants, 1998.
5. HAKME F. Contratura capsular. Complicações da capsulotomia fechada pós-implante de silicone nas hipomastias.F.Méd. (BR), 82 (5): 537-546, 1981.
6. SEMPLES J., et al. Breast milk contamination and silicone implant: preliminary results using silicon as a proxy measurement for silicone. Plast. Reconstr. Surg. 1998; 102:528-31.
7. YOUNG VL. Guidelines and indications for breast implant capsulectomy. Plast. Reconstr. Surg. 1998; 102:884-90.
8. TUEBER, et al. Anti-collagen are found in women with silicone breast implants. J. Autoimmunity. 1993; 6:357-62.
9. ROCKWELL WB et et al. Breast capsule persistence after breast implant removal. Plast. Reconstr. Surg. 1998; 101: 1085.
10. CARVALHO CG, BAROUDI R. Contratura esférica em torno das proteses mamarias. Anais do XIII Congr. Bras. Cir. Plast. e I Congr. Bras. Cir. Estet., Porto Alegre, RS, Brasil, 1976.
11. EMBREY M, et al. A review of the literature on the etiology of capsular contracture and a pilot study to determine the outcome of capsular contracture interventions. Aesth. Plast. Surg. 1999; 23:197-206.
12. COLLIS N, SHARPE DT. Recurrence of Subglandular breast implant capsular contracture: anterior versus total capsulectomy. Plast. Reconstr. Surg. 2000; 106: 792-97.
I - Senior Member of the Brazilian Society of Plastic Surgery and director of Instituto de Cirurgia Plastic a Santa Cruz [Santa Cruz Institute of Plastic Surgery].
II - Member of the Brazilian Society of Plastic Surgery and assistant physician of Instituto de Cirurgia Plástica Santa Cruz.
III - Aspiring member of the Brazilian Society of Plastic Surgery and resident physician at the Instituto de Cirurgia Plástica Santa Cruz.
Address for correspondence:
José Marcos Mélega, MD
R. Santa Cruz, 398 - Vila Mariana
04122-000 - São Paulo - SP Brazil
Phone: (55 11) 5575-9863
e-mail: ispsc@uninet.com.br
Study performed at the Instituto de Cirurgia Plástica Santa Cruz [Santa Cruz Institute of Plastic Surgery]


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter