

Articles - Year 2002 - Volume 17 -
Giant Breast Lipoma - Case Report
Lipoma Mamário Gigante - Relato de Caso
ABSTRACT
The manuscript describes a quite infrequent giant breast lipoma progressing slowly since adolescence, in a young female adult. Clinical, pathology, diagnosis and therapeutic aspects are emphasized.
Keywords: Lipoma; breast; mammaplasty; breast reconstruction; surgery
RESUMO
É relatado um caso pouco freqüente de lipoma mamário gigante, com evolução lenta desde a adolescência, em uma paciente adulta jovem, enfatizando-se os aspectos clínicos, patológicos, diagnósticos e terapêuticos.
Palavras-chave: Lipoma; mama; mamoplastia; reconstrução mamária; cirurgia
Lipomas are benign fat tissue minors, of which mesenchymal tumors arc the most common ones(1) . They are generally single, but may be multiple and finely encapsulated, and present an estimated incidence of 10 %. They have an insidious and limited growth, mainly in the subcutaneous tissue of the neck, trunk, face, hands and feet. They also affect deep structures, such as the retroperitoneum, skeletal muscles, mediastinum, gastrointestinal tract, kidneys, bronchi, liver, myometrium, spleen, heart, central nervous system, salivary and mamary glands(2). They grow in the breast as in any other site with fatty tissue(3,4) and may be considered giant when thcv grow excessively Breast lipomas must be palpated and have to present capsule and fibrous septs in order to be diagnosed as such.
OBJECTIVE
To point out clinical, pathology, diagnosis and therapeutic aspects of giant lipomas, by describing a quite infrequent breast lipoma progressing slowly since adolescence, in a young female adult.
CASE REPORT
ECM, 30 years old, female, Caucasian, married, business administrator, from the city of Rio de Janeiro.
The patient presented since adolescence, a palpable, mobile, elastic-firm consistence, painless tumor 1ocated in the lower portion of the left breast, measuring approximately 15 cm in its longest axis. The steady growth led to important asymmetry (Figs.la-c). The radiographic exam of the breast showed an encapsulated tumor with a defined contour and precise limits compatible with lipoma (Fig. 2). Both breasts were marked according to the Pitanguy mammaplasty technique (Fig. 3). The indicated resection of the tumor was performed. The macroscopic aspect was of fat, yellowish and shiny tissue, weighing 400 g and measuring 15 x 9.5 x 5 cm (Figs. 4a-e). Immediate reconstruction of the left breast was performed, with a lateral flap of the upper pedicle (Figs. 5a-b). Balance mammaplasrv was performed on the contralateral breast (Fig. 6).
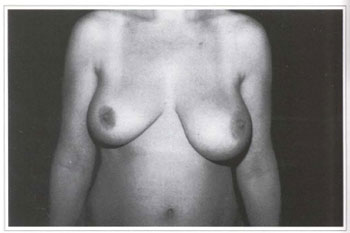
Fig. la - Preoperative period; frontal view.
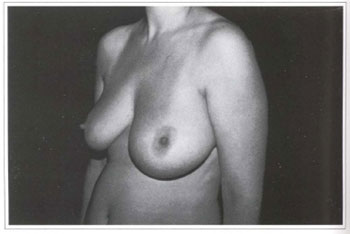
Fig. 1b - Preoperative period; lef lateral view.
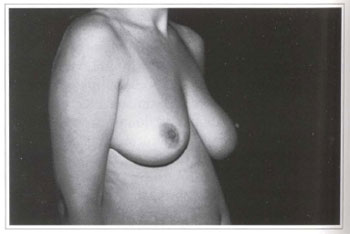
Fig. 1c - Preoperative period; right lateral view.

Fig. 2 - Detail of the x-ray showing the encapsulated tumor with defined contours and accurate limits, suggesting lipoma.
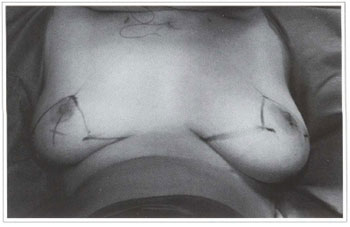
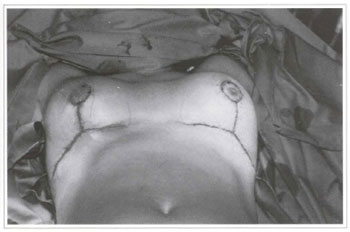
Fig. 3 - Preoperative marking according to Pitanguy's mammaplasty technique.
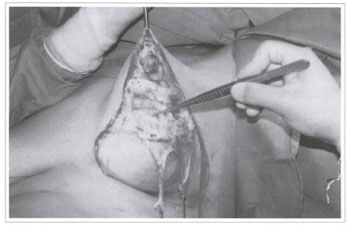
Fig. 4a - Intraoperative period; partial view of the tumor.

Fig. 4b - Resection of the tumor comprised of yellowish, shiny fatty tissue.
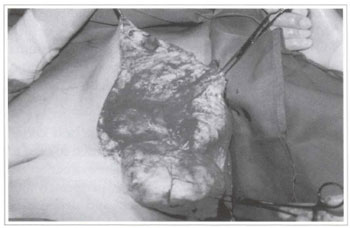
Fig. 4c - Resection of the tumor comprised of yellowish, shiny fatty tissue.
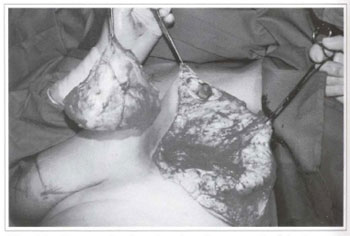
Fig. 4d - Panoramic view showing the removal of the large tumor.
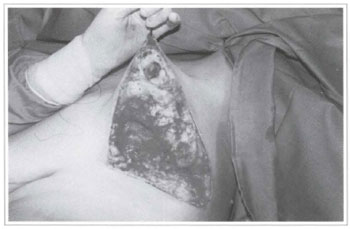
Fig. 4e - Space left after tumor removal.

Fig. 5a - Reconstruction of the left breast with a lateral surgical flap of the upper pedicle.
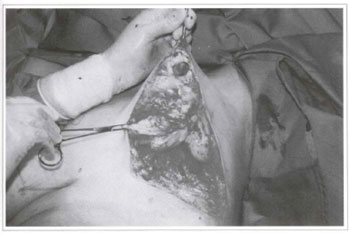
Fig. 5b - Reconstruction of the left breast with a lateral surgical flap of the upper pedicle.
Fig. 6 - Immediate postoperative period. Final suture. The right, breast was submitted to balance mammaplasty.
RESULTS
There were no problems during the postoperative period, and the surgical wound healed very well. Breast asymmetry was corrected making the patient more comfortable and greatly satisfied due to the excellent aesthetic result (Figs. 7a-c).
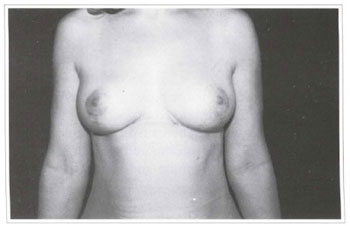
Fig. 7a - 1 year postoperative period; frontal view. Excellent healing of the surgical wound with satisfactory results.
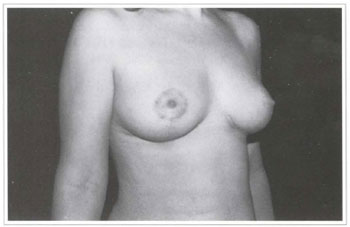
Fig. 7b - Postoperative period; right lateral view.
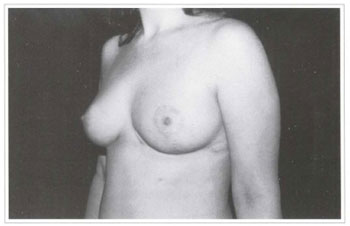
Fig. 7c - Postoperative period; left lateral view.
DISCUSSION
Lipomas affect mostly women with a positive family history, mainly when they are multiple. There seems to be a relationship between their development and obesity. Most tumors are single or present in a limited number. Subcutaneous lipomas are frequently small, measure 1 to 4 cm in diameter, and they may grow beyond 10 cm and weigh up to 10 g(2). Lipomas rarely grow excessively leading to symptoms.
In 1894, Brandlers(5) described a 22.7 kg skin lipoma in the left scapular region, of a young 26 year-old male adult.
There are no rules for defining the exact size of a tumor in order to consider it giant. Weight alone is not enough to define it, since the multiplication of fibrous obstacles in the fatty tissue increases tumor density, without substantially changing its size(6). Our literature review suggested that giant lipomas should measure at least 10 cm in diameter or weigh at least 1,000 g(2).
Lipomas are considered one of the most innocent tumors and rarely cause symptoms. Deeper lipomas, however, may cause symptoms due to pressure on contiguous structures(7). Internal lipomas may grow considerably before producing symptoms such as abdominal pain, renal failure or other systemic complications, and may evolve into a sarcomatous rumor.
On the other hand, skin lipomas rarely become lipossarcomas(8).
Giant skin lipomas basically pose aesthetic problems, which are more frequent in the cervical, thoracic and lower limb (inguinal and thigh) regions. Thev may occasionally lead to functional limitations or linfedema. Signs and symptoms derive from proximity to other structures, such as nerves for example. Lipomas rarely calcify and, when they do, the degeneration is due to infarctions of large volume tumors.
They should not be confounded with galactoceles or steatonecrosis that do not have internal fibrous septs. The differential diagnosis of lipomas is primarily with cysts (sebaceous, pilonidal and inclusion), xanthoma and papulonodular lesions, such as rheumatoid nodules and neuromas. The main differential diagnosis of giant lipomas are with soft tissue rumors (that affect vessels, nerves, tendons, and muscles), in addition to bone tumors.
Malignant transformation is rare, and it should be suspected in fast growing, recurrent tumors with skin ulcerations(9). When there is a clinical suspicion of lipoma, imaging tests help supply additional diagnostic information. Ultra-sound, mammography, computerized tomography and magnetic nuclear resonance may show a lipoma-compatible lesion(7).
Only histopathological diagnosis is definite. Macroscopically, it consists of yellowish, shim; fatty tissue separated by fine fibrous trabecula. Microscopy reveals mature fatty tissue, without cell atypia; only perfectly developed adipocytes are present. Fat cells are identical to normal fat, and may be mixed to fibrous tissue. Mesenchymial elements are frequently found. Areas of infarction, necrosis, calcification, bone or cartilaginous metaplasia, superficial ulceration, infection and gangrene are possible secondary changes(2).
The surgical treatment of lipomas is generally performed under local or general anesthesia. Tumor dissection is eased by the pressure of the surrounding tissue that forms a well-defined pseudo-capsule. There are usually no signs of recurrence after surgery(7).
Conventional surgical treatment is preferable, mainly when the lipoma infiltrates muscles or involves large vessels or nerves. Lipoaspiration, has, however, been reported as another form of treatment, by removing fat. Large hematomas and recurrences caused bv incomplete removal of tumors are possible complications of lipoaspiration(10).
In the case presented, tumor resection and immediate reconstruction of the left breast were indicated and performed, with a lateral flap of the upper pedicle, and aesthetic correction using Pitanguy's mammaplasry technique. After the extirpation of the tumor in the left breast, the contra lateral breast was submitted to balance mammaplasty.
In 1961, Pitanguy described one of the best known mammaplasty techniques, which was used for the reconstruction of the case presented. The evaluation and delimitation of the resection area is performed individually, on each breast separately and depends on various factors, such as glandular consistency, volume and skin elasticity. The technique has proven itself capable of avoiding skin-gland detachment because the previously calculated and precise measurements of the three pedicles (median, upper and lateral) allow for the spontaneous adjustment of the borders of the initial incisions to their final positions and into a cone-shaped breast(11).
CONCLUSION
Giant lipomas appear in the breast as in other parts of the body, and are considered primarily an aesthetic and benign problem. When suspected clinically, radiographic tests may corroborate the diagnosis. The surgical treatment is definite and satisfactory when performed adequately.
REFERENCES
1. Mescon H. Lipoma in clinical dermatology. Clin Dermatol. 1991;4:1-2.
2. Juan R. Surgical Pathology. 1994; 2:1573-79.
3. Bloom RA, Gomnri JM, Feelds SI, Katz E. Abdominal wall lipoma - CT and MRI appearence. Compute Med Imaging Graf 1991;15:37.
4. Ryndholm A, Berg HO. Size, site and clinical incidence of lipoma. Acta Orthop Scand. 1983;54:929-34.
5. Brandler TI. Large Fibrolipoma. Br Med J. 1894;1:574.
6. Sanchez MR. Giant lipoma - case report and review of the literature. J Am Acad Dermatol. 1993;28:266-8.
7. Eli KH, et al. Giant lipomas. Plast Reconstr Surg. 1994;94:369-71.
8. Enzinger FM, Weiss SW. Soft tissue rumors. St. Louis: CV Mosby. 1988:341-45.
9. Fleegler EJ. Tumors of the Upper Extremity. WC Grabb and JW Smith (Eds). Plast Surg. Boston:Little Brown; 1991. p.983-4.
10. Lewis CM. Treatment of large lipoma of the back. Herter GP ed. Lipoplasty: the theory and practice of blunt suction lipectomy Boston:Little Brown; 1984. p. 128-41.
11. Piranguy I. Mammaplastic, Estudo de 245 casos consecutivos de mamoplastia e apresentação de técnica pessoal. Rev Bras Cir. 1961;42:201-20.
I. Senior Member Of the Brazilian Society of Plastic Surgery, Assistant Professor of the Plastic Surgery Discipline of Hospital Universitário Pedro Ernesto - UERJ.
II. Senior Member Of the Brazilian Society of Plastic Surgery, Assistant Professor of the Plastic Surgery Discipline of Hospital Universitário Pedro Ernesto - UERJ.
III. Candidate Member of the Brazilian Society of Plastic Surgery, Medical Resident of Hospital Universitário Pedro Ernesto - UERJ.
Address for correspondence:
José Horácio Costa Aboudib Júnior, MD
Av. Ataulfo de Paiva, 341, sls. 801/802
22440-030 - Rio de Janeiro - RJ - Brazil
Phone: (55 21) 2511-3669
e-mail: aboudib@mtecnet.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter