

Original Article - Year 2011 - Volume 26 -
Long-term outcomes of periareolar approach for reduction mammaplasty
Avaliação dos resultados tardios de mamoplastia redutora pela técnica periareolar
ABSTRACT
Objective: To document our procedure for periareolar reduction mammaplasty, evaluate its long-term benefits and disadvantages, and assess the degree of satisfaction of patients with at least 10 years of follow-up. Methods: We randomly selected 25 patients who underwent periareolar reduction mammaplasty with at least 10 years of follow-up and analyzed several criteria such as breast volume, breast shape and symmetry, nipple-areolar complex sensibility, scar quality, patient opinion and satisfaction level, and number of complications and reoperations. All patients answered specific questionnaires, allowing percent-based evaluation of each variable. Results: Most patients would confidently undergo a repeated mammaplasty by the periareolar technique. The breast volume and shape remained stable with good patient satisfaction. The most frequent complaint was the scar quality. Conclusions: The periareolar approach is useful for reduction mammaplasty in patients with small-to-medium breast volume, small-to-moderate ptosis, and moderate-to-good skin turgor. Its main disadvantage is the tendency of enlargement of the scar around the areola over time.
Keywords: Mammaplasty/methods. Breast/surgery. Reconstructive Surgical Procedures. Surgery, Plastic.
RESUMO
Introdução: Foram selecionadas aleatoriamente 25 pacientes submetidas a mamaplastia redutora pela técnica periareolar, com no mínimo 10 anos de pós-operatório. Em nenhum momento houve o espírito de avaliar comparativamente com outros tipos de técnica em uso no arsenal da cirurgia de redução e pexia mamária. Objetivo: Avaliar os benefícios e as desvantagens desta técnica a longo prazo. Método: Foram selecionados e analisados critérios como tamanho, formato, simetria, sensibilidade no complexo aréolo-papilar, qualidade das cicatrizes, assim como a opinião das pacientes, além do registro de complicações, reintervenções e do grau de satisfação. Todas as pacientes responderam a questionários específicos, permitindo conclusões avaliadas percentualmente para cada tipo de variável. Resultados: Dentre os comentários obtidos, a maioria das pacientes concordou que se submeteria a nova mamaplastia pela técnica periareolar. O volume e a forma das mamas mantiveram-se estáveis e com elevado grau de satisfação por parte das pacientes. A queixa mais frequente foi relacionada à cicatriz. Conclusão: O resultado da análise comprovou que a abordagem periareolar é um procedimento muito útil para as mamaplastias redutoras em pacientes com pequena a média hipertrofia, sem ptose marcante e com aceitável a boa elasticidade cutânea. A principal desvantagem, entretanto, é a tendência da cicatriz ao redor da aréola alargar com o tempo.
Palavras-chave: Mamoplastia/métodos. Mama/cirurgia. Procedimentos Cirúrgicos Reconstrutivos. Cirurgia Plástica.
Patient satisfaction after cosmetic surgery, including mammaplasty, is defined by the long-term rather than the short-term results of the surgery with regard to minimal scarring and preservation of skin sensitivity and functionality. Although the periareolar approach1-4 to breast reduction and mammopexy fulfills these criteria, its range of indications is restricted.
In 1992, Bustos5 described the use of the periareolar technique with the implant of a nylon lamina for better modeling of the breasts and greater aesthetic effect in the long term. This approach offers good results but has a high rate of complications. Góes6-8 used the periareolar technique with a polypropylene mesh for the same reasons but reported a lower incidence of delayed reactions and satisfactory long-term results. Benito and Sanza9 did not employ any kind of fabric involving the breast tissue but opted for "round-block" suturing around the areola to minimize the extension of the scar.
We have used Bustos' technique for over 15 years10 while omitting the nylon lamina and including other surgical procedures. Several tactical and technical alterations to the procedure have been introduced over the years11,12. The objectives of this study were to document our procedure for periareolar reduction mammaplasty, evaluate its long-term benefits and disadvantages, and assess the degree of satisfaction of patients with at least 10 years of follow-up.
METHODS
Twenty-five female patients were randomly selected from a series of 100 patients. All had at least 10 years of follow-up and moderate breast hypertrophy, absence or presence of grade I ptosis, and good skin turgor. Their age ranged from 16 to 49 years at the time of surgery. From this group, we collected a broad range of information deemed important to validate the application of this technique in aesthetic mammaplasty.
The patients answered questionnaires with topics ranging from the quality of results; the final volume, shape, and ptosis of the breasts; the aesthetic quality of the papillary-areolar complex (PAC); and symmetry and quality of the scar to the patient's level of satisfaction. We also collected data on complications and reoperations. Furthermore, the patients gave their opinions regarding whether they would undergo the same technique again. All items were scored by grades and/or criteria.
All the questionnaires were prepared by the authors and analyzed by a statistician. Interviews with patients were conducted by a health professional who was not part of the surgical team to avoid possible emotional stress bias.
Demarcation of the Breasts
Preoperative markings were performed with the patient in a sitting position, with the back straight, and without premedication. Point A was marked as the upper limit of the areola about 8 cm from the inframammary fold, and not as point (A') according to Pitanguy's technique13, and was therefore 2 cm above it. Point B was marked as the lower limit of the areola 4-6 cm above the inframammary fold. The medial boundary (point C) and lateral boundary (point D) were positioned according to bidigital skin pinching; they marked the medial and lateral limits of de-epithelization to the respective edges of the areola. Point D should be nearer to the areolar edge than point C to prevent lateralization (Figure 1). Because of the subjectivity involved in such marking, the surgeon should have relevant experience.
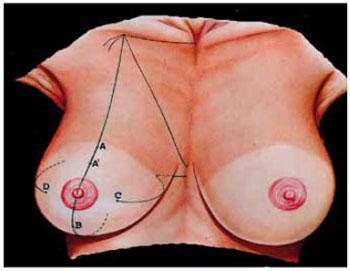
Figure 1 - Schematic appearance of skin markings. Points A and B indicate the upper and lower limits of the areola to be repositioned. They are located 8 and 4 cm from the inframammary fold, respectively. Point A in Pitanguy's technique represents the projection of the nipple, but it was not used as a parameter. Points C and D represent the medial and lateral limits of the areola, with point D a few millimeters closer to the areola than point C, to prevent its lateralization.
Surgical Technique
The surgery was performed with the patient under general anesthesia and with local infiltration of epinephrine (1:200,000) in all the parts to be dissected and a 4.0 cmdiameter areolotome to determine the new external circular limit of the areola.
Epithelial removal was performed in the area bound by points A-D through the boundary demarcated by the areolotome (Figure 2). We then dissected and mobilized the mammary tissue in the upper quadrants in the cranial direction up to the aponeurosis of the pectoral muscle and then caudally to the level of the nipple-areolar complex (NAC) (Figure 3 and 4). The upper quadrants were exposed, with transverse resection of any excess above the NAC, along the line marked by the compass (Figure 5). In cases of inadequate resection, a new wedge-shaped resection of these quadrants on the sagittal plane was performed to complement the volume reduction (Figure 6). The aponeurosis of the pectoral muscle as well as the two upper (lateral and medial) quadrants were sutured together with increased rotation of the external quadrant by using isolated nylon 3.0 stitches, rebuilding the upper pole of the breast.
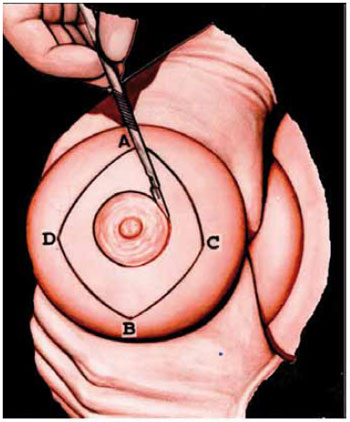
Figure 2 - Schematic view of the limits of skin to be de-epithelialized within points A-D and the areolar edge.
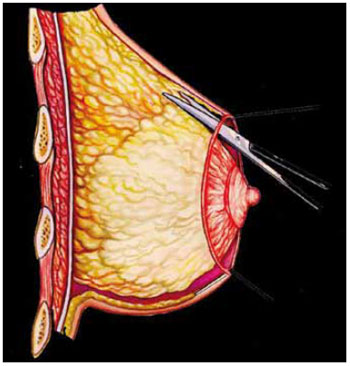
Figure 3 - Schematic sagittal cross-section of the breast. The upper quadrants are dissected with scissors at the edge of the glandular adipose tissue, up to the aponeurosis of the pectoralis major.
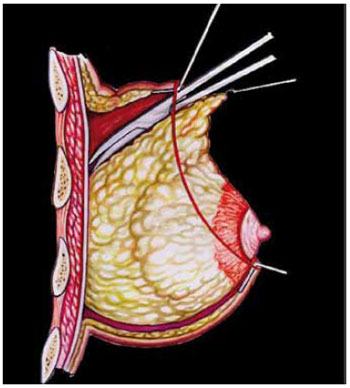
Figure 4 - Continued dissection with scissors by extending along the same plane of the aponeurosis of the pectoral muscle in the caudal direction to the level of the horizontal plane of the top edge of the areola.
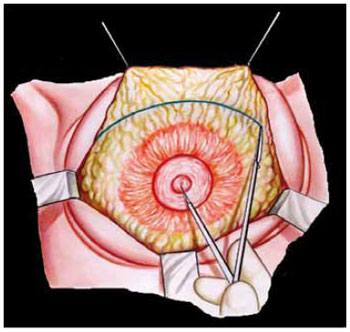
Figure 5 - Anterior view of the dissected breast, where the resection is demarcated according to the surgeon's evaluation. One end of the compass is applied at the NAC and the other is set at the limits of the breast to resect en bloc the excesses in the upper quadrants. The resection is wedge shaped, comprising the entire thickness of the glandular adipose tissue toward the demarcated line. Then, the upper quadrants of the musculoaponeurotic plane of the pectoralis major are sutured.
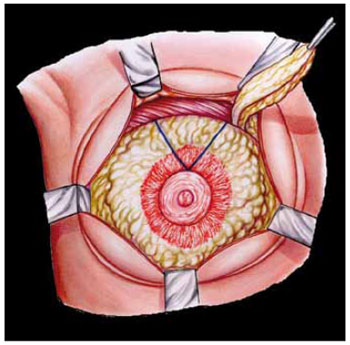
Figure 6 - When the resection of the upper quadrants is insufficient, a new wedge-shaped resection in the sagittal plane is performed to reduce the volume.
The dissection limit and location of stitches determine the upper pole of the mammary tissue (Figure 7). Round-block continuous suturing was performed with nylon 3.0 stitches in the subdermal plane, preferably with a straight needle (Figure 8). Porous tape was applied directly on the whole sutured areola. Vacuum aspiration drains were used for 24-48 h. The breasts were covered with gauze and cotton. The duration of hospital stay was 24 h, and the patients were required to wear a surgical bra before discharge.
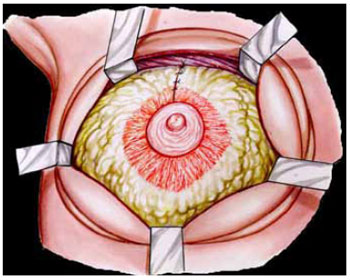
Figure 7 - Suturing performed in the sagittal plane for breast turning and conification.
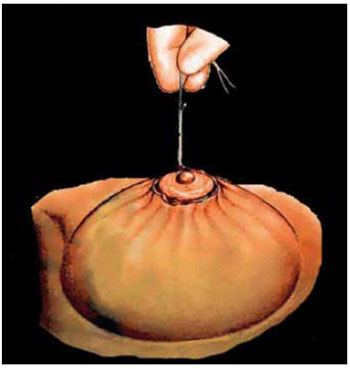
Figure 8 - Final round-block suturing of the skin to the areolar edge.
RESULTS
In this study, a large amount of data regarding patients who underwent periareolar mastoplasty was recorded and statistically analyzed.
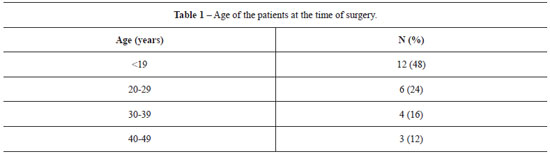
At the time of surgery, 48% of the patients were aged under 19 years, 52% were 20-39 years old, and 12% were 40-49 years old (Table 1).
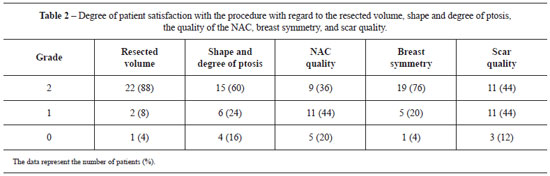
Table 2 shows the degree of patient satisfaction with the procedure, assessed according to 3 grades (2, 1, and 0) for 5 aspects: resected volume, shape and degree of ptosis, quality of the NAC, symmetry of the breasts, and scar quality. Except for the quality of the NAC that was graded as 1, all the other aspects were mostly graded as 2.
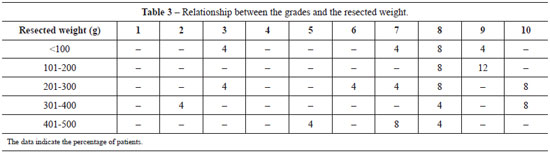
The level of satisfaction with the decrease in breast volume was between 6 and 10 in 60% of the patients for reductions up to 300 g in each breast and 24% for reductions of 301 to 500 g, whereas 16% of the patients indicated scores lower than 6, irrespective of breast volume (Table 3).
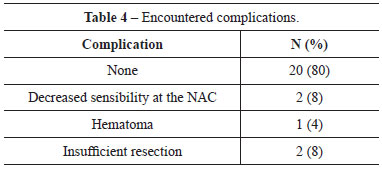
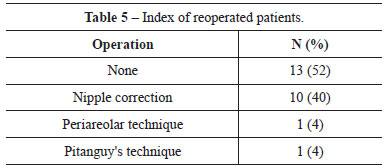
Table 4 shows that 20% of the patients experienced no complications, 2 patients (8%) had unilateral numbness of the NAC, 2 patients (8%) had inadequate resection, and 1 patient (4%) developed hematoma. Concerning reoperations, 10 patients (40%) underwent periareolar scar revision, 1 patient (4%) underwent the same technique, and 1 patient (4%) underwent Pitanguy's technique (Table 5).
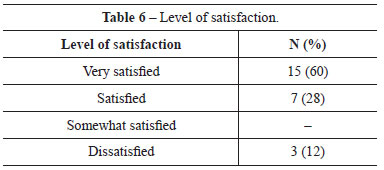
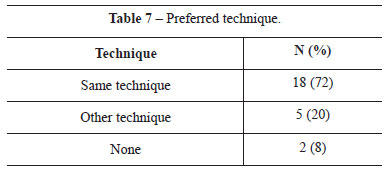
For the results obtained with the procedure, 60%, 28%, and 12% of the patients were very satisfied, satisfied, and dissatisfied, respectively (Table 6). At the time of the interview, when asked about the technique they would choose if they were to undergo the surgery again, 72% of the patients said they would repeat the same technique, 20% preferred another technique, and 8% said they would not undergo any procedure (Table 7). Table 8 shows the sum of the responses regarding the receptivity of the results, scored from 0 to 10.
DISCUSSION
Our surgical procedure is based on the technique of Bustos5, with some modifications that allowed omission of the lamina. Overcorrection of the mammary cone is possible by extensive dissection and resection of breast volume in the upper pole when necessary, followed by cranial sliding of the medial and lateral segments of glandular adipose tissue and suturing between them and the aponeurosis of the pectoralis major. This maneuver induces higher resistance to the contrary pressure of round-block suturing, which causes scar widening over time.
We do not use a lamina in this technique because its use, despite the good quality of results, may present a higher rate of complications. The periareolar technique, especially without a mesh, requires less skin resection than the techniques with final T, L, or even vertical scars. This peculiarity limits its application to small- and medium-sized breasts without markedly flaccid skin, which is more common among younger patients.
According to the results, we observed a very positive response from patients in relation to the volume and final symmetry of the breasts. We believe this to be related to the technical advancements, namely the greater rotation of the medial and lateral flaps of glandular tissue, allowing greater projection of the breast cone and avoiding the flat shapes observed in the earlier uses of this technique. Regarding shape and ptosis, patients were not as satisfied as compared to reports in previous studies; the limited resection of skin and lack of elasticity were prevalent factors in this issue. The worst grades were given to the appearance of the scars and the shape of the NAC. This occurs because the tension experienced by the areola in the round-block technique is greater than that in other procedures, possibly resulting in broadened scars.
As for the satisfaction rate, 88% of the patients reported being satisfied or very satisfied, and this finding was similar to evaluations of other techniques13,14. Among the patients dissatisfied with the results, one was reoperated on by using the same technique, another underwent Pitanguy's technique13, and the third declined further breast surgery.
This study aimed to conduct a follow-up assessment of patients. Undoubtedly, the periareolar technique is another option for mammaplasty, with good acceptance. The use of the periareolar approach has increased, and as quoted by Rohrich et al.13, "the periareolar technique needs a major revision due to the lowest physician satisfaction, despite its application to a large number of mammoplasty per year".
Periareolar reduction mammaplasty is a good option for patients who require a reduction of less than 500 g in each breast15, with some authors using periareolar surgery with vertical offset16,17. We performed higher resection of the upper pole and higher sliding of the glandular flaps, with the areola toward the upper pole; the purpose of this maneuver is to ensure hyperprojection of the breast cone to contrast the contrary pressure on the skin after round-block suturing.
CONCLUSIONS
By evaluating the long-term results and preservation of aesthetic quality, we conclude that periareolar reduction mammaplasty has a high acceptance rate among patients due to the existence of a single scar around the areolas. The main limiting aspects are restricted application in patients with small and medium hypertrophy, with good skin turgor, and the tendency for scar widening.
REFERENCES
1. Rosel E, Starcks RB. Circum areolar mastopexy. Personal communication at the American Society of Plastic and Reconstructive Surgeons; 1973.
2. Andrews JM, Yshizuri MM, Martins DM, Ramos RR. An areolar approach to reduction mammaplasty. Br J Plast Surg. 1975;28(3):166-70.
3. Bartels RJ, Strickland DM, Douglas WM. A new mastopexy for mild or moderate breast ptosis. Plast Reconstr Surg. 1976;57(6):687-91.
4. Erol OO, Spira M. A mastopexy technique for mild to moderate ptosis. Plast Reconstr Surg. 1980;65(5):603-9.
5. Bustos RA. Periareolar mammaplasty with silicone supporting lamina. Plast Reconstr Surg. 1992;89(4):646-57.
6. Góes JCS. Periareolar mammaplasty: double skin technique. Rev Soc Bras Cir Plast. 1989;4:55-63.
7. Góes JC. Periareolar mammaplasty: double skin technique with application of polyglactine or mixed mesh. Plast Reconstr Surg. 1996;97(5):59-68.
8. Góes JC. Periareolar mastopexy: double skin technique with mesh support. Aesthet Surg J. 2003;23(2):129-35.
9. Benito J, Sanza IF. Periareolar techniques for mammary reduction and elevation. Aesthetic Plast Surg. 1993;17(4):311-6.
10. Aboudib JH Jr, Castro CC. Mammaplasty utilizing the periareolar approach. Aesthetic Plast Surg. 1998;22(1):51-7.
11. Felício Y. Periareolar reduction mammaplasty. Plast Reconstr Surg. 1991;88(5):789-98.
12. Fayman MS, Potgieter E, Becker PJ. Outcome study: periareolar mammaplasty patient's perspective. Plast Reconst Surg. 2003;111(2):676-84.
13. Rohrich RJ, Gosmann AA, Brown SA, Reisch J. Mastopexy references: a survey of board-certified plastic surgeons. Plast Reconst Surg. 2006;118(7):1631-8.
14. Cho BC, Yang JD, Baik BS. Periareolar reduction mammaplasty using an inferior dermal pedicle or a central pedicle. J Plast Reconstr Aesthet Surg. 2008;61(3):275-81.
15. Courtiss EH, Goldwyn RM. Reduction mammaplasty by the inferior pedicle technique. An alternative to free nipple and areola grafting for severe macromastia or extreme ptosis. Plast Reconstr Surg. 1977;59(4):500-7.
16. Martins PDE. Periareolar mammaplasty with flap transposition. Rev Bras Cir Plast. 1991;6(1-2):1-6.
17. Hammond DC, Alfonso D, Khuthaila DK. Mastopexy using the short scar periareolar inferior pedicle reduction technique. Plast Reconstr Surg. 2008;121(5):1533-9.
1. Professor of Plastic Surgery, State University of Rio de Janeiro, Chief of Plastic Surgery, Pedro Ernesto University Hospital - State University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
2. Plastic Surgeon, Pedro Ernesto University Hospital - State University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Ana Claudia Weck Roxo
Rua Ipanema, 21 - Barra
Rio de Janeiro, RJ, Brazil - CEP 22631-390
E-mail: anacwroxo@rjnet.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: July 8, 2009
Accepted: March 17, 2011
Work performed at the Hospital Universitário Pedro Ernesto - Universidade Estadual do Rio de Janeiro - (Pedro Ernesto University Hospital - State University of Rio de Janeiro), Rio de Janeiro, RJ, Brazil.



 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter