

Original Article - Year 2011 - Volume 26 -
Versatility of the bilobed flap
Versatilidade do retalho bilobado
ABSTRACT
Background: The bilobed flap is a double transposition flap. Its geometric drawing allows a better distribution of tensile forces along its axis of rotation, avoiding distortions and dog ears generated by other flaps and primary closure. It can be harvested in an axial or random pattern depending on where the defect is located on the body. Methods: Retrospectively, this study reviewed 45 consecutive bilobed flaps searching for pathology, anatomical area, clinical evolution and complications. The technique utilized in drawing and harvesting the flap is described in detail. Sizes of the defects were classified as small, moderate and large, taking into account the anatomical sites. A variety of clinical cases is presented exploring the versatility of the flap and etiology of the defects. Results: The bilobed flap was employed in oncological surgery in 93% of the cases while the skin of the head was involved in 71%.The post operative period was free of complications in 85%. Infection rate was 4.4%, trapdoor scaring rate was 4.4% and partial flap loss rate was 11.1%. The overall complication rate was 15%. In spite of all complications there were no compromise in the functional and aesthetic results and the bilobed flaps proved to be resolute and reliable in different clinical presentations and body regions. Conclusions: The bilobed flap is extremely versatile, easily reproducible with wide application in plastic surgery.
Keywords: Skin. Face. Surgical flaps. Plastic surgery/methods. Reconstructive surgical procedures.
RESUMO
Introdução: O retalho bilobado é um retalho de dupla transposição. Sua estruturação geométrica permite melhor distribuição das forças de tensão ao longo de seu eixo de rotação, evitando distorções e redundâncias cutâneas geradas por outros retalhos ou sutura primária. Pode ser confeccionado com padrão vascular axial e aleatório, dependendo da região anatômica. Métodos: Este trabalho faz uma revisão de 45 casos operados, descrevendo em detalhes a técnica utilizada para confeccionar o retalho bilobado. Os defeitos são classificados em pequenos, médios e grandes e diversos casos clínicos são apresentados, explorando a versatilidade desse retalho em diferentes diagnósticos etiológicos e sítios anatômicos. Resultados: Em 93% dos casos, o retalho bilobado foi empregado em reconstruções oncológicas, sendo o segmento cefálico acometido em 71%. Não houve qualquer intercorrência pós-operatória em 85% dos casos. A taxa de infecção foi de 4,4%; de cicatriz em alçapão, de 4,4%; e de epiteliólise e necrose, de 11,1%. A taxa geral de complicações foi de 15%. Entretanto, tais complicações não comprometeram a evolução clínica dos casos e o retalho bilobado mostrou-se resolutivo em diferentes situações, propiciando bom resultado tanto funcional como estético. Conclusões: O retalho bilobado é versátil, de fácil execução e com ampla aplicabilidade em cirurgia plástica.
Palavras-chave: Pele. Face. Retalhos cirúrgicos. Cirurgia plástica/métodos. Procedimentos cirúrgicos reconstrutivos.
The bilobed flap was first described in the German literature in 1918 by Esser1 as an ideal structure for closing defects in the nasal tip. However, it became popular in 1953 when Zimany2, a plastic surgeon at the University of New York, published a description of this flap in the English literature. The bilobed flap is a double transposition flap with a single pedicle in which the first flap is transposed into a defect and the second, smaller flap is transposed to fill the secondary defect caused by the larger flap transposition. Thus, the forces of tension are distributed in various directions, and the skin distortions and redundancy generated by a simple transposition flap or by primary closure are reduced.
In 1989, Zitelli3 methodized the bilobed flap for the reconstruction of defects in the nasal tip and alar. After performing studies in cadavers, several other authors4,5 introduced changes in lobe angles and sizes in order to reduce the incidence of the 5% of distortion in the tip and alar retraction.
Defects in other anatomical sites have subsequently been repaired using the bilobed flap6. Yenidunya et al.7,8 demonstrated the applicability of the flap in the frontal and infraorbital regions and stressed the importance of locating the pedicle superiorly in these areas to avoid caudal traction of the lower eyelid. Furthermore, for male patients, they warned against the movement of beard hair contained in the flap lobes.
El-Khatib9 reported a series of 11 cases of necrotizing fasciitis in the posterior cervical region, in which he reported excellent results from using bilobed fasciocutaneous flaps whose pedicles were formed by musculocutaneous perforators of the contralateral trapezius muscle. The same principle was used by Atik et al.10, who treated 20 cases of myelomeningocele with an average size of 38 cm2. The employed design positioned most of the flap in a contralateral position relative to the pedicle. Despite the reported stasis, only 1 case of partial necrosis of the flap, which did not harm the case evolution, was found.
Mutaf et al.11 demonstrated the applicability of the bilobed flap from the anterior cervical region in the total and post-traumatic reconstruction of the ear under unfavorable conditions due to the presence of large amounts of scar tissue and the impossibility of using the temporoparietal fascia.
Hsieh et al.12 used the isolated bilobed flap to close the donor area of the antebrachial radial free flap. The pedicle, consisting of 1 to 3 fasciocutaneous perforators of the ulnar artery, gave mobility and good perfusion to the flap. This technique eliminated the need for partial skin grafting, enabled early mobilization of the hand in the immediate postoperative period, and offered great aesthetic improvement to the donor area.
In order to facilitate flap marking, Iida et al.13 converted the defect into a rhomboid shape and the lobes into a triangular shape, resulting in the increased consumption of skin and a worse aesthetic result. Therefore, this technique was not widely used. The bilobed flap was used in lower limb and upper limb reconstruction by Maruyama14 and Onishi et al.15, respectively.
In an attempt to standardize marking and provide better use of the surrounding tissues, Meadows et al.16 developed an excellent methodology that can be applied in many cases of reconstruction with a bilobed flap. The larger lobe is 75% of the size of the defect, and the smaller lobe is 75% of the size of the larger lobe. This systematization is easy to understand and reproduce (Figure 1).

Figure 1 - Marking of Meadows et al.16 In A, basal cell carcinoma of the patients back and flap design. In B, resected tumor and flap ready for transfer. In C, postoperative period of 3 months, showing good tissue accommodation.
This review aims to describe the applicability, surgical planning, and complications of using the bilobed flap in the reconstruction of defects caused by various diseases in different anatomical regions.
METHODS
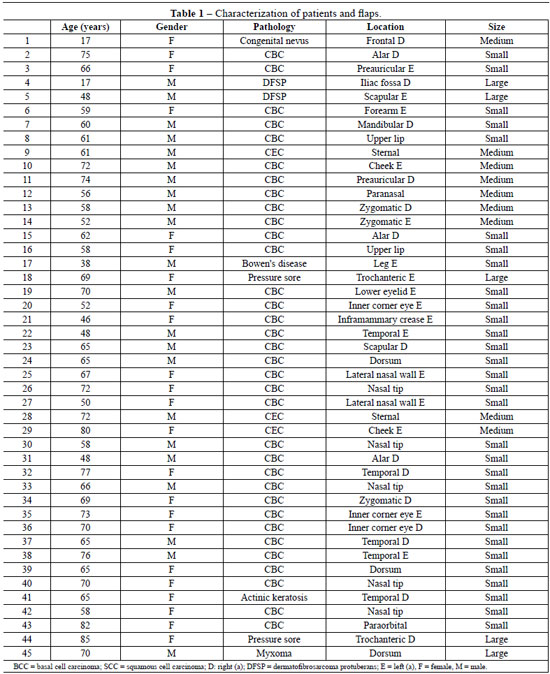
In a retrospective analysis conducted between July 2004 and August 2010, 42 patients who underwent 45 tissue reconstructions with bilobed flaps used for treatment of injuries of different etiologies were identified (Table 1).
Patients were 62 years old on average, ranging from 17 to 85 years old. The flaps were equally distributed between the genders, and 93% of the reconstructions were derived from tumor resections. Although basal cell carcinoma was the most prevalent (81%) among skin tumors, rare tumors (7.1%) such as dermatofibrosarcoma protuberans and angiomyxoma, together with other disorders, completed the case selection.
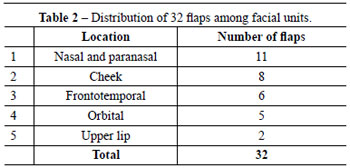
The face was the most frequently involved body part in reconstructions (71%) followed by the trunk (20%), lower limbs (6.7%), and upper limbs (2.2%). On the face (Table 2), the most affected region was the nose (34%), followed by the cheek (25%) and the frontotemporal (18.7%) and infraorbital (15%) regions. The flaps were employed for the closure of small defects in 70% of the cases and major defects in 11%.
Surgical Technique
The flaps were designed according to the size and location of the defect, the presence of adjacent perforating vessels, neighboring tissues compliance, and position; where possible, future scars were positioned along lower tension skin lines.
To this end, the following plan was used:
1. the larger lobe was designed in an arc shape and was the same size as the defect, was 10% larger when located in inelastic areas or the alar or nasal tip, or was 10% to 20% smaller in other cases, with an angle of approximately 45° between the defect and the flap;
2. the smaller lobe was designed in an arc or ogive shape and was 25% to 50% smaller than the larger lobe, forming an angle of approximately 45° to 50° between the larger and smaller lobes;
3. the lobes were designed where the skin was looser;
4. the defect location, tension lines, and clamping the skin between the fingers helped to define the smaller lobe location;
5. the flaps were detached and rotated so that the first flap would fill the primary defect, the second would fill the secondary defect, and the defect left by the smaller lobe would be primarily closed;
6. occasionally, it was necessary to remove a triangle of skin between the defect and the pivot point;
7. anchor points were routinely made between the flap and the deep tissue in the recipient bed;
8. the underlying muscle fascia was incorporated into the flap in the trunk and limbs.
The defects were measured and classified as small, medium, or large based on their size and anatomical location. The flap versatility was determined by the ability to close defects in different anatomical sites, causing minimal tissue distortion and favorable aesthetic and functional outcome. The flap reproducibility was determined by the ability of the flap to close a defect in a specific anatomical site with a low incidence of complications.
The flaps were monitored in the immediate and later postoperative periods for the occurrence of infection, hematoma, epitheliosis, necrosis, and trapdoor scar. A flap that did not show any of the changes mentioned above was determined as favorable evolution.
Figures 2 to 8 illustrate the bilobed flap applicability.
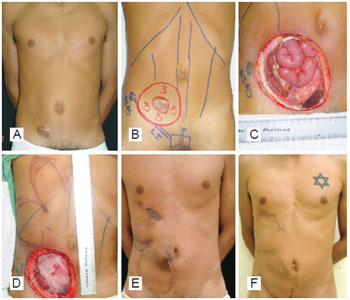
Figure 2 - Large defect. In A, dermatofibrosarcoma protuberans present in the right inguinal region. In B, preoperative marking with a safety margin of 3 cm. In C, tumoral resection including aponeurosis, right rectus abdominis, and right parietal peritoneum (107 cm2). In D, polypropylene mesh on the parietal peritoneum flap and bilobed flap marking. In E, postoperative period of 2 months. In F, postoperative period of 2 years and 4 months, after scar revisions.

Figure 3 - Medium defect. In A, congenital hair nevus in the right frontal region. In B, surgical planning to avoid eyebrow distortion. In C, postoperative period of 7 days. In D, postoperative period of 2 months: the well-positioned eyebrow with makeup.

Figure 4 - Medium defect. In A, dermatofibrosarcoma protuberans in the left scapular region. In B, safety margin of 3 cm and defect of 32 cm2. In C, elevated flap. In D, postoperative period of 5 years.

Figure 5 - Medium defect. In A, basal cell carcinoma in the nasal tip. In B, surgical planning with a narrow pedicle. In C, epitheliosis. In D, postoperative period of 9 months: despite the notch in the soft triangle, there was no retraction of the nose margin.

Figure 6 - Small defect. In A, defect after resection of basal cell carcinoma located at the left lower eyelid. In B, myocutaneous flap of sutured orbicularis muscle. In C, postoperative period of 14 days.

Figure 7 - Complication. In A, ulcerated basal cell carcinoma in the left forearm. In B, surgical planning. In C, infection and partial necrosis of the flap. In D, postoperative period of 10 months, demonstrating excellent functional and aesthetic results after debridement and healing by secondary intention.

Figure 8 - Medium defect. In A, ulcerated basal cell carcinoma in the left alar and nasogenian region with invasion of the facial mimic muscles. In B, surgical planning. In C, sutured flap. In D, postoperative period of 1 year and 10 months.
RESULTS
The largest reconstructed defects with bilobed flaps were 107 cm2 (Figure 2), 44 cm2 (case 45), and 32 cm2 (Figure 4) and involved rare skin tumors, which often require wide 3-dimensional safety margins.
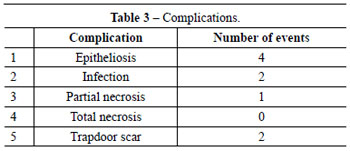
The rates of infection, trapdoor scar, and epitheliosis that evolved with or without necrosis were 4.4%, 4.4%, and 11.1%, respectively. The overall rate of complications was 15%, which is comparable with that found in the reviewed literature (Table 3). The procedure was expectant in cases of epitheliosis, and debridement was performed and healing occurred by secondary intention without aesthetic or functional harm in the single case of necrosis (Figure 7).
DISCUSSION
This study has many similarities with numerous publications in the literature17. The incidences of infection and necrosis were low and the management of epitheliosis was expectant. In the single case of necrosis, debridement was performed and healing occurred by secondary intention without aesthetic or functional harm.
Oncological reconstructions prevailed and the most affected body part was the head. The most affected regions of the face were the nose and cheek followed by the frontotemporal and orbital regions. In all cases, the flaps were well-indicated, resolutive, and provided good final functional and aesthetic results.
Although these is no single angle that provides better results, angles from 45° to 50° between both the defect and the larger lobe and between the lobes were most frequently used in this case selection and in different publications. The size of the largest lobe must be equal to the defect or slightly larger (approximately 10%) when the anatomical site does not allow any distortion (nasal and orbital regions) or the skin is inelastic and has intense movement (joint and neck regions). In other cases, the largest lobe can be slightly smaller (10% to 20%) than the defect. The smaller lobe may be 25% to 50% smaller than the larger lobe, depending on the tissue elasticity of the specific region.
Infection, tension in the sutures, or narrow pedicle was present in cases where total or partial loss of tissue thickness occurred.
The bilobed flap enables both defect closure with no or minimal distortion of the surrounding tissues and transfer of skin with similar color and texture. Therefore, it can be randomly or axially applied, structured in a simple (skin) or complex (fasciocutaneous and myocutaneous) manner, and is easy to perform. Given these advantages, the bilobed flap has been applied in other regions of the face, neck, trunk, and limbs.
The Dzubow18 study, which demonstrated the restriction exercised by the pedicle in the movement of rotation and transposition flaps, corroborates the conclusions and changes suggested by Zoumalan et al.4 and Cho & Kim5 to the methods of Zitelli3,19. Dzubow18 determined that the length of the larger lobe is elongated at the alar and nasal tips and in areas where the skin has reduced elasticity. Therefore, the smaller lobe should be perpendicularly positioned to an anatomical structure that cannot undergo displacements, such as the eyebrow and nostril margin.
The versatility of the flap was proven by its ability to close defects of different sizes and in different locations with the same efficiency. Given the systematic use of the described method and the low rate of complications, it was possible to observe that the flap is easy to implement and its outcome is reproducible.
The analysis of this case selection and the referenced literature show that since its creation by Esser1, the bilobed flap has undergone modifications that made its implementation easier and improved its outcomes. Many of the concepts introduced for the performance of nasal defect reconstruction were incorporated into the reconstruction of other anatomical regions (Figures 2, 4, and 6). Thus, this evolution gives the plastic surgeon the freedom to choose lobe sizes and angles (Figure 8), and it can be inferred that the term "bilobed" alludes not only to the flap but to the principle of tissue transfer.
CONCLUSION
The bilobed flap is a versatile and resolutive flap. Its applicability in different etiologies and different anatomical sites provides various forms of reconstruction with very satisfactory results. The main advantages of this flap include the low rates of complication, easy reproducibility, the similarity in color and texture in relation to the site of the defect, and the possibility of designing it in different sizes and tissue compositions. Many authors consider it the first choice in the closure of various defects, even in areas with low skin compliance.
REFERENCES
1. Esser JFS. Gestielte lokale nasenplastik mit zweizipfligen lappen: deckung des sekunderen defectes vom ersten zipfel durch den zweiten. Dtsch Z Chir. 1918;143:385-90.
2. Zimany A. The bilobed flap. Plast Reconstr Surg. 1953;11(6):424-34.
3. Zitelli JA. The bilobed flap for nasal reconstruction. Arch Dermatol. 1989;125(7):957-9.
4. Zoumalan RA, Hazan C, Levine VJ, Shah AR. Analysis of vector alignment with the Zitelli bilobed flap for nasal defect repair: a comparison of flap dynamics in human cadavers. Arch Facial Plast Surg. 2008;10(3):181-5.
5. Cho M, Kim DW. Modification of the Zitelli bilobed flap: a comparison of flap dynamics in human cadavers. Arch Facial Plast Surg. 2006;8(6):404-9.
6. Cordeiro CN, McCarthy CM, Mastorakos DP, Cordeiro PG. Repair of postauricular defects using cervical donor skin: a novel use of the bilobed flap. Ann Plast Surg. 2007;59(4):451-2.
7. Yenidunya MO. Axial pattern bilobed flap for the reconstruction of the midline forehead defects. Plast Reconstr Surg. 1999;103(2):737.
8. Yenidunya MO, Demirseren ME, Ceran C. Bilobed flap reconstruction in infraorbital skin defects. Plast Reconstr Surg. 2007;119(1):145-50.
9. El-Khatib HA. Bilobed fasciocutaneous flap for reconstruction of the posterior neck after necrotizing fasciitis. Plast Reconstr Surg. 2004;114(4):885-9.
10. Atik B, Tan O, Kiymaz N, Yilmaz N, Tekes L. Bilobed fasciocutaneous flap closure of large meningomyeloceles. Ann Plast Surg. 2006;56(5):562-4.
11. Mutaf M, Isik D, Atik B, Bulut O. Versatility of the bilobed cervical skin flap for total ear reconstruction in the unfavorable temporoauriculomastoid region. Plast Reconstr Surg. 2006;118(3):652-62.
12. Hsieh CH, Kuo YR, Yao SF, Liang CC, Jeng SF. Primary closure of radial forearm flap donor defects with a bilobed flap based on the fasciocutaneous perforator of the ulnar artery. Plast Reconstr Surg. 2004;113(5):1355-60.
13. Iida N, Ohsumi N, Tonegawa M, Tsutsumik K. Simple method of designing a bilobed flap. Plast Reconstr Surg. 1999;104(2):495-9.
14. Maruyama Y. Bilobed fasciocutaneous flap. Br J Plast Surg. 1985;38(4):515-7.
15. Onishi K, Maruyama Y, Okada E. Bilobed fasciocutaneous flap for primary repair of a large upper arm defect with secondary closure of the donor site without a skin graft. Ann Plast Surg. 1997;39(2):205-9.
16. Meadows AE, Rhatigan M, Manners RM. Bilobed flap in ophthalmic plastic surgery: simple principles for flap construction. Ophthal Plast Reconstr Surg. 2005;21(6):441-4.
17. Moy RL, Grossfeld JS, Baum A, Rivlin D, Eremia S. Reconstruction of the nose utilizing a bilobed flap. Int J Dermatol. 1994;33(9):657-60.
18. Dzubow LM. The dynamics of flap movement: effect of pivotal restraint on flap rotation and transposition. J Dermatol Surg Oncol. 1987;13(12):1348-53.
19. Zitelli JA. Design aspect of the bilobed flap. Arch Facial Plast Surg. 2008;10(3):186.
1. Non-masters postgraduate course at the School of Medicine of Universidade de São Paulo (FMUSP), plastic surgeon at public and private hospitals, São Paulo, SP, Brazil.
2. Full professor of the Discipline of Plastic Surgery at FMUSP, Head of the Department of Craniomaxillofacial Surgery, Hospital das Clinicas, FMUSP, São Paulo, Brazil.
3. Specialist member of the Brazilian Society of Plastic Surgery (SBCP), physician in a private clinic, São Paulo, SP, Brazil.
4. Practitioner resident at the Plastic Surgery Service of Oswaldo Cruz-Mandaqui, São Paulo, SP, Brazil.
Correspondence to:
Luiz Alexandre Lorico Tissiani
Rua Mato Grosso, 306 - cj. 1405 - Cerqueira César
São Paulo, SP, Brazil - CEP 01239-040
E-mail: latissiani@terra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: May 28, 2011
Accepted: August 4, 2011
Study conducted at Complexo Hospitalar do Mandaqui, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter