

Original Article - Year 2011 - Volume 26 -
Nymphoplasty: classification and technical refinements
Ninfoplastia: classificação e refinamentos técnicos
ABSTRACT
Background: Hypertrophy of the labia minora is a functional and esthetic problem that can have a significant impact on quality of life. Current surgical procedures are based on the excision of excess tissue and reconnection of the edges. However, anatomical alterations associated with labial hypertrophy such as hypertrophy of the foreskin of the clitoris are common, and, if not treated properly, may limit the results of surgery and cause esthetic and functional sequelae. The present report proposes a classification of the different types of hypertrophy and recommended treatments, and describes refinements in the labia minora reduction techniques. Methods: A total of 20 female genital plastic surgery cases from the Center for Plastic Surgery of Brasilia and at Hospital das Forças Armadas from June 1999 to March 2008 were retrospectively reviewed. Patients were classified into three groups according to the degree and location of labia minora hypertrophy. Results: The patients were satisfied with the esthetic results of surgery. No complications were reported, and all patients underwent surgery of the labia minora in accordance with the protocol proposed by the authors and based on hypertrophy type. Conclusions: The surgical procedures reviewed in this study were based on the classification of labia minora hypertrophy. Satisfactory esthetic and functional results were obtained, thus providing new methods for the surgical reduction of labia minora and foreskin of the clitoris without surgical stigma or reduction of sensitivity and no effects on sexual function.
Keywords: Vulva/surgery. Clitoris/surgery. Gynecologic surgical procedures/methods.
RESUMO
Introdução: A hipertrofia dos pequenos lábios traz problemas estéticos e de comprometimento do comportamento íntimo e social. As técnicas existentes, via de regra, propõem excisão do excesso de tecido e reaproximação das bordas; entretanto, diferenças anatômicas são comuns e, frequentemente, observa-se hipertrofia do prepúcio do clitóris associada a aumento dos pequenos lábios. Essas alterações, se não tratadas adequadamente, limitam o resultado, podendo produzir sequelas estéticas e funcionais. Este trabalho propõe uma classificação dos tipos de hipertrofia, com tratamento diferenciado para cada um deles, além de refinamentos técnicos na abordagem da hipertrofia dos pequenos lábios. Métodos: Estudo retrospectivo de 20 casos de plástica genital feminina, realizada no Centro de Cirurgia Plástica de Brasília e Hospital das Forças Armadas, no período de junho de 1999 a março de 2008. As pacientes foram classificadas em três grupos, de acordo com o grau e a localização da hipertrofia dos pequenos lábios. Resultados: As pacientes mostraram-se muito satisfeitas com o aspecto estético proporcionado pela cirurgia. Não foram verificadas complicações relacionadas aos procedimentos realizados. Todas as pacientes foram submetidas a tratamento cirúrgico dos pequenos lábios de acordo com o protocolo proposto pelos autores, baseado no tipo de hipertrofia. Conclusões: Os procedimentos cirúrgicos realizados, propostos de acordo com a classificação da hipertrofia dos pequenos lábios, permitiram a obtenção de resultados estéticos e funcionais satisfatórios, proporcionando à paciente oportunidade de redução do excesso dos pequenos lábios e do prepúcio do clitóris, sem criar estigmas cirúrgicos ou diminuição da sensibilidade, não prejudicando, portanto, a função sexual.
Palavras-chave: Vulva/cirurgia. Clitóris/cirurgia. Procedimentos cirúrgicos em ginecologia/métodos.
Anatomical changes of the labia minora can be associated with functional and esthetic discomfort, interfering with personal hygiene, the use of tight clothing, sexual relations, and affecting feminine self-perception1-11.
Labial hypertrophy can be congenital or acquired through chronic irritation, extreme weight gain, or endogenous or exogenous hormone (androgen) action1-3.
Although there is no established anatomical standard regarding the size of the labia minora, the standard of normality is based on the concept that the labia minora should be covered by the labia majora, which must superiorly converge and partially cover the clitoris when the patient is examined in an anatomical position, i.e., with legs raised.
Because of the current increase in the exposure of the female body in magazines, movies, internet, etc., women are more aware of the natural differences in the external genital anatomy and are able to make comparisons with the more pleasant esthetic model of the nymphs and labia majora.
The perception of the body and its association with self-esteem are important factors for achieving personal satisfaction2-6, and often lead patients to seek plastic surgery to help improve body contour. This fact has, to some extent, led to an increase in the demand for this type of surgery in recent years.
Reservations regarding surgery in this anatomical region are mostly due to surgical stigmas such as scars and potential anatomical changes, or even the possibility of a reduction in sensitivity and dyspareunia5-7. Therefore, the procedure used for genital plastic surgery should not be considered as a simple elliptical resection of the excess tissue. Surgeons should be aware of the particular anatomical characteristics of each individual, and adjust the surgical procedure in each case5-8.
During the course of this study, the absence of a classification to describe the excess tissue and common alterations in different patients was noticed. The present study aims to propose a classification of the most common anatomical variations of the labia minora, and determine the appropriate surgical strategy for each case, as well as the respective technical refinements.
METHODS
A total of 20 female genital plastic surgery cases performed at the Center for Plastic Surgery of Brasilia and at Hospital das Forças Armadas from June 1999 to March 2008 were retrospectively reviewed. Patients' ages ranged from 27 to 55 years. Patients were classified into three groups according to the degree and location of the labia minora hypertrophy:
type I - excess of skin on the posterior/inferior region, adjacent to the vaginal introitus (Figure 1);
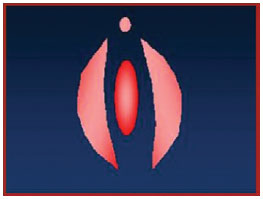
Figure 1 - Schematic representation of type I hypertrophy of the labia minora.
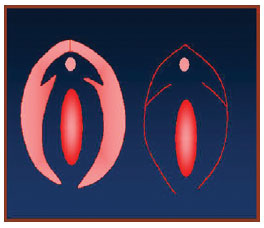
type II - excess of skin laterally and superiorly extended to the clitoris (Figure 2);
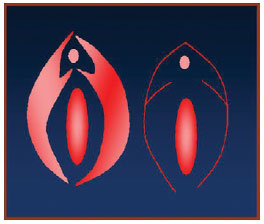
Figure 2 - Schematic representation of type II hypertrophy of the labia minora.
type III - excess of skin in the whole area, including the foreskin of the clitoris (Figure 3).
Figure 3 - Schematic representation of type III hypertrophy of the labia minora.
All patients underwent surgery of the labia minora in accordance with the protocol proposed by the authors, which was based on the type of hypertrophy.
Resection of excess labia minora tissue was performed in a medially inclined plane (more internally, in the vaginal introitus), thus resulting in a more internal and less apparent scar. Hemostasis was performed with a high-frequency scalpel and the continuous whipstitch suture was made with a 5-0 Caprofyl® wire (poliglecaprone 25/Ethicon).
All patients were operated by the same surgical team, 15 under epidural block and 5 under local anesthesia and sedation. The patients were placed in the lithotomy position and kept hospitalized for 6 to 24 hours, depending on the type of anesthesia and the association with other procedures (related surgeries). No other procedure was performed in the vicinity of the operated area.
In the postoperative period, patients were subjected to relative rest and use of cold compresses during the first few hours and local antiseptics (Andolba® spray) for two weeks.
Patients were treated with antibiotic therapy (cefazolin 1 g, intravenously, one dose during anesthetic induction and every 8 hours during the first 24 hours, and cefadroxil 500 mg orally, every 12 hours for five days) and non-steroidal anti-inflammatory drugs (Tilatil® 20 mg, orally, every 12 hours, for five days). Sexual abstinence was recommended for three weeks.
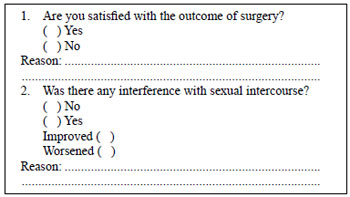
Patients were followed as outpatients for at least six months including examination of the anatomical results of surgery and a subjective evaluation that consisted of a questionnaire on patient satisfaction and the effects of surgery on sexual activity. The following questionnaire was used:
The study was approved by the ethics committee of the Center for Plastic Surgery of Brasilia (CIRPLÁS).
RESULTS
The patients were very satisfied with the esthetic appearance as a result of surgery; they did not report any negative interference during sexual intercourse, in fact there were some reports of improvement in sexual function.
The anatomical results of the operation were considered to be satisfactory, and no surgical scar was verified (Figures 4 to 9).
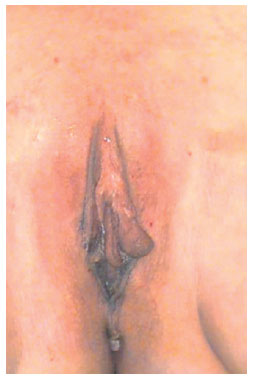
Figure 4 - Case report: type I change.

Figure 5 - Case report: type II change.

Figure 6 - Case report: type III change.

Figure 7 - Postoperative period in patients with type I hypertrophy of the labia minora.

Figure 8 - Postoperative period in patients with type II hypertrophy of the labia minora.

Figure 9 - Postoperative period in patients with type III hypertrophy of the labia minora.
No complications associated with the procedure were reported.
DISCUSSION
The greater average age of patients that seek surgical correction for labial hypertrophy is a reflection of sexual maturity, a higher degree of information, and the search for a better body image that is characteristic of patients in this age group. The current technical refinements for this procedure, the improvement in the results of surgery, and the breaking of taboos are expected to result in a greater number of patients seeking labia reduction surgery at a younger age.
The small number of publications available on this topic is a reflection of a reduced interest in the improvements in female genital surgeries on the part of specialists; moreover, a narrow view regarding the approach to this surgery was noticed, which was often limited to the simple resection of the excess tissue.
The treatment of labia minora hypertrophy based on a classification of different types of anatomical alterations leads to better esthetic results. The present work proposes a new surgical approach for the correction of excess tissue in the clitoris region based on the excision of the foreskin adjacent to the labia minora, which reduces the foreskin in a natural manner, without amputation or loss of sensitivity. The currently proposed procedure was aimed at limiting scars to the most internal part of the vaginal introitus, by means of a more internal resection of the excess tissue in the vulvar region. This treatment led to the achievement of a more natural appearance.
Surgery was preferably performed under epidural anesthesia to ensure the comfort of the patient and the surgeon, as the area is very sensitive to pain and the tissue is loose, which can easily lead to deformation with anesthetic infiltration, thus affecting the anatomical evaluation. Patient comfort is important to obtain better hemostasis and for synthesis of the incision, which helps avoid the major predictable complications, such as error in the amount of resected area, hematoma, wound dehiscence, and barely approximate edges.
The use of non-hormonal anti-inflammatory agents is indicated by the high incidence of edema and local hypersensitivity, which are characteristic of this region.
Using the strategy proposed in this study, which summarizes the authors' approach to the morphological refitting of the vulva, high rates of patient satisfaction were obtained, both in esthetic and functional aspects.
CONCLUSION
Esthetic surgery of the external female genitalia should be approached with seriousness and care, as this is an area associated with strong emotional impact.
New strategies and surgical refinements are currently emerging, and the present study was aimed at revealing the progress in the area of female genital surgery.
The surgical procedures reviewed in this study were based on the classification of labia minora hypertrophy, and satisfactory esthetic and functional results were obtained. These improvements will provide patients with the opportunity to undergo procedures for the reduction of labia minora and foreskin of the clitoris without surgical stigma or sensitivity reduction, thus avoiding undesirable effects on sexual function.
REFERENCES
1. Hodgkinson DJ, Hait G. Aesthetic vaginal labioplasty. Plast Reconstr Surg. 1984;74(3):414-6.
2. Alter GJ. A new technique for aesthetic labia minora reduction. Ann Plast Surg. 1998;40(3):287-90.
3. Alter GJ. Central wedge nymphectomy with a 90-degree Z-plasty for aesthetic reduction of the labia minora. Plast Reconstr Surg. 2005;115(7):2144-5.
4. Rouzier R, Louis-Sylvestre C, Paniel BJ, Haddad B. Hypertrophy of labia minora: experience with 163 reductions. Am J Obstet Gynecol. 2000;182(1 pt 1):35-40.
5. Choi HY, Kim KT. A new method for aesthetic reduction of labia minora (the deepithelialized reduction of labioplasty). Plast Reconstr Surg. 2000;105(1):419-22.
6. Munhoz AM, Filassi JR, Ricci MD, Aldrighi C, Correia LD, Aldrighi JM, et al. Aesthetic labia minora reduction with inferior wedge resection and superior pedicle flap reconstruction. Plast Reconstr Surg. 2006;118(5):1237-47.
7. Maas SM, Hage JJ. Functional and aesthetic labia minora reduction. Plast Reconstr Surg. 2000;105(4):1453-6.
8. Giraldo F, González C, de Haro F. Central wedge nymphectomy with a 90-degree Z-plasty for aesthetic reduction of the labia minora. Plast Reconstr Surg. 2004;113(6):1820-5.
9. Girling VR, Salisbury M, Ersek RA. Vaginal labioplasty. Plast Reconstr Surg. 2005;115(6):1792-3.
10. Radman HM. Hypertrophy of the labia minora. Obstet Gynecol. 1976;48(1 Suppl):78S-9S.
11. Kato K, Kondo A, Gotoh M, Tanaka J, Saitoh M, Namiki Y. Hypertrophy of labia minora in myelodysplastic women. Labioplasty to ease clean intermittent catheterization. Urology. 1998;31(4):294-9.
1. Plastic surgeon, full member of the Brazilian Society of Plastic Surgery (SBCP), clinical director of the Center for Plastic Surgery of Brasília (CIRPLÁS), Brasília, DF, Brazil.
2. Plastic surgeon, full member of the SBCP, plastic surgeon at the State Secretariat of Health of the Federal District, Brasília, DF, Brazil.
3. Plastic surgeon, full member of the SBCP, Brasília, DF, Brazil.
4. Plastic surgeon, full member of the SBCP, plastic surgeon at Hospital das Forças Armadas, Brasília, DF, Brazil.
5. Specialist in plastic surgery, plastic surgeon at the State Secretariat of Health of the Federal District, Brasília, DF, Brazil.
Correspondence to:
Fábio Inácio da Cunha
SHLS 716 - Bloco C - 1º andar - Asa Sul
Brasília, DF, Brazil - CEP 70390-904
E-mail: fabiocunha@brturbo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: May 19, 2011
Accepted: July 29, 2011
Study conducted at Hospital das Forças Armadas and at the Center for Plastic Surgery of Brasília (CIRPLÁS), Brasília, DF, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter