

Original Article - Year 2011 - Volume 26 -
Post-bariatric thighplasty: result assessment
Coxoplastias pós-cirurgia bariátrica: avaliação dos resultados
ABSTRACT
Background: Patients who experience massive weight loss often require a thighplasty procedure to reduce excess skin and reshape thighs and lower body contour, improving movement, hygiene, posture, self-image, and quality of life. Methods: After weight loss and stabilization of weight, eight patients in the postoperative period of gastric bypass were subjected to a thighplasty. Measurements of upper and lower circumferences of the thighplasty and thigh heights were obtained in the preoperative and postoperative periods of 60 and 180 days for comparison of volume change after the surgical procedure. Results: The average volume reduction of each thigh at a postoperative period of 180 days was 1,135 cm3 or 1.135 liters. All patients had small areas of dehiscence along the scars on the medial thigh, and dressings were applied for healing by secondary intention. One (12.5%) patient had cysts in both thighs, confirmed by ultrasound, and required surgical intervention for resection and subsequent resolution. Conclusions: It was possible to demonstrate significant reduction in the volume of each thigh after plastic surgery for contour refitting. Patient satisfaction and complications associated with the procedures performed were also documented.
Keywords: Bariatric surgery. Weight loss. Plastic Surgery. Thigh/surgery.
RESUMO
Introdução: Pacientes que apresentam perda maciça de peso muitas vezes precisam reduzir o excesso de pele e remodelar o contorno das coxas e parte inferior do corpo, melhorando os movimentos, higiene, postura, autoimagem e qualidade de vida. Métodos: Oito pacientes em pós-operatório de gastroplastia redutora, após perda e estabilização do peso, foram submetidas a coxoplastia. Medidas das circunferências superior e inferior e da altura das coxas foram obtidas em pré-operatório e pós-operatório de 60 dias e 180 dias, para comparação de alteração de volume consequente ao procedimento cirúrgico. Resultados: A redução média de volume de cada coxa, aos 180 dias de pós-operatório, foi de 1.135 cm3 ou 1,135 litro. Todas as pacientes apresentaram pequenas deiscências ao longo das cicatrizes em face medial das coxas, sendo realizados curativos com cicatrização por segunda intenção. Uma (12,5%) paciente apresentou cistos em ambas as coxas, confirmados por ultrassonografia, sendo necessária intervenção cirúrgica para ressecção e consequente resolução. Conclusões: Foi possível demonstrar redução significativa do volume de cada coxa após cirurgia plástica para readequação do contorno, além de documentar a satisfação das pacientes e as complicações associadas aos procedimentos realizados.
Palavras-chave: Cirurgia bariátrica. Perda de Peso. Cirurgia Plástica. Coxas/cirurgia.
According to the Pittsburgh Rating Scale1, hip deformities in ex-obese patients are classified into three types: the first are deformities with moderate fat accumulation; the second are those with pronounced fat accumulation; and the third are those with large skinfolds with little or no fat content.
Surgery is the treatment for each type of deformity, and the assessment of the results is purely subjective, either by the patient or the surgeon.
This study aims to surgically address thigh deformity types 2 and 3 in the Pittsburgh Rating Scale and assess the results by calculating the geometric volume of the thighs in the pre- and postoperative period of 60 and 180 days.
METHODS
A prospective study was performed for eight female patients with a mean age of 35.22 years, ranging from 24 years to 46 years. The average body mass index (BMI) was 25.6 kg/m2, ranging from 24.4 kg/m2 to 30.5 kg/m2. All patients had undergone the Fobi-Capella gastroplasty approximately four years previously, and the average BMI before that surgery was 49 kg/m2, ranging from 43.9 kg/m2 to 57.8 kg/m2.
Patients were recruited from the Body Contouring Group at the Plastic Surgery and Burn Service of Hospital das Clinicas of the School of Medicine of Universidade de São Paulo (São Paulo, SP).
The patients were in good health, were non-smokers, and did not take drugs that could lead to behavioral changes. They underwent a psychological assessment to ensure understanding of this protocol as well as to receive information on the value of the proposed treatment and overcome any disappointment with the results. All patients signed the informed consent form. No patient was receiving hormone therapy, both contraceptive and replacement.
Following the same methodology, postoperative measurements were obtained at 60 and 180 days.
Surgical Technique
The technique used for medial face treatment was proposed by Aly & Cram2. Hence, the resection followed the design of a longitudinal spindle, superiorly extended from 2 cm below the midpoint between the insertion tendons of the large adductor and gracilis muscles of the thigh up to 2 to 3 cm behind the medial tuberosity of the femur (Figure 1). The width of this spindle was delimited by bi-digital clamping with the patient in the standing position, an essential step to avoid excessive resection that could contribute to tension in the wound suture. Laterally, the next step was the resection scheme proposed by Baroudi3, marking a spindle in the lateral and upper regions of the thigh, delimited by a line that is the prolongation of the lower abdominal groove. The lower limit was obtained by demarcation of a line defined by bi-digital clamping, avoiding excessive resection (Figure 2). Tumescent liposuction was performed in order to reduce fat content and facilitate removal of larger areas. The resections were performed above the superficial fascia. In order to avoid upper excess of adipose tissue in the dermal area, the longitudinal line was broken down with a spindle resection in the inguinal crease. The wounds were sutured in three planes: one deep, with separate 3.0 Polyamide sutures; one subdermal, with separate sutures of 4.0 polyglycolic acid; and an intradermal continuous plane with 5.0 poliglecaprone. Antibiotic dressing was applied (ointment or cream) and covered with gauze and lattice with microporous adhesive tapes. Straps with moderate compression were used. No drains were used. Antibiotic prophylaxis with cefazolin was administered to all patients. In the immediate postoperative period, patients were encouraged to deambulate early; in bed, they were encouraged to actively and passively move the lower limbs.
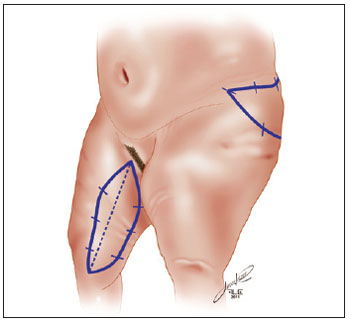
Figure 1 - Demarcation of resection area in the form of a longitudinal spindle for treatment of the medial face of the thigh and demarcation of lateral resection area.
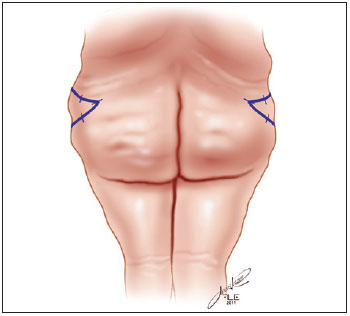
Figure 2 - Demarcation of resection area on the lateral face of the thigh in posterior view.
Calculation
The thigh was considered to be shaped like a cone body, and the volume was assessed in the preoperative period and at 60 and 180 days postoperatively.
The following preoperative measurements of the patients' thighs were obtained in the upright position, always by the same surgeon: the higher circumference (C), horizontally, close to the inguinal crease; the lower circumference (c), horizontally, close to the femur lateral condyle; and the height (h), the vertical distance between two circumference measures on the lateral aspect of the thigh.
The volume was calculated using the following equation:
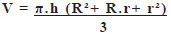
where h = height of the thigh measured from the projection of the greater trochanter to the femur lateral condyle; R = larger radius of the circumference measured from the inguinal crease, encircling the thigh horizontally, and is represented by R = C/2xπ; and r = smaller radius of the circumference measured, circling the thigh on the projections of the medial and lateral condyles of the femur and is given by r = c/2xπ.
RESULTS
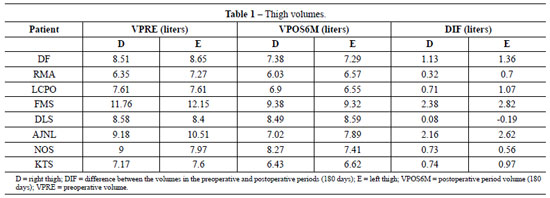
Table 1 shows the result of volumetric assessments of eight patients, revealing that there was a considerable decrease in the size of the thighs operated on 180 days after weight loss operation, with an average total of 1.135 cm3 per thigh.
Subjectively, all patients expressed great satisfaction with the result of the operation, which enabled broader deambulation movements, easier hygiene, use of long pants, sexual performance enhancement, and more harmonious round contour of the thighs (Figures 3 to 9).
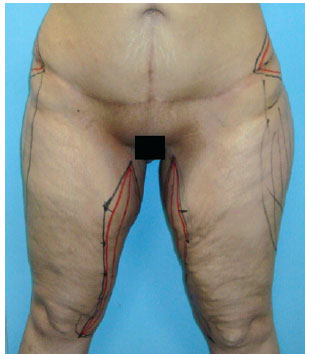
Figure 3 - DLS patient: preoperative surgical marking.
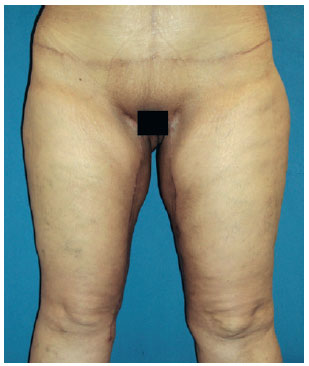
Figure 4 - DLS patient: postoperative period of 180 days.

Figure 5 - DF patient: preoperative period.
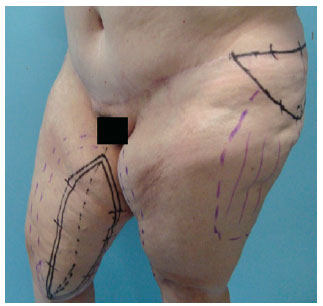
Figure 6 - DF patient: preoperative marking.
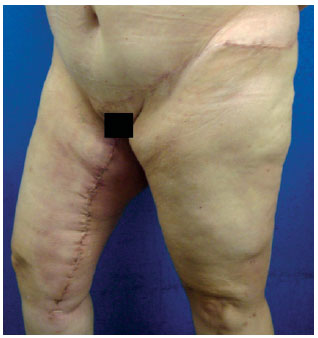
Figure 7 - DF patient: postoperative period of 60 days.

Figure 8 - NOS patient: preoperative period.
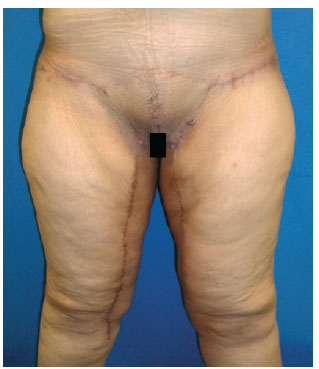
Figure 9 - NOS patient: postoperative period of 180 days.
Complications
The most frequently observed complications in all patients were small areas of dehiscence along the scars on the medial aspect of the thighs, which did not exceed 2 cm and healed by secondary intention without major aesthetic or functional harm. These dehiscences were attributed to sutures being subjected to tension. One patient developed seromas in both thighs; these seromas were subsequently punctured. However, the seromas formed cysts, which were confirmed by ultrasound. Another surgery was performed for resection of these cysts, with good postoperative evolution and no recurrence.
DISCUSSION
Because of residual fat accumulation in the lateral and medial aspects of the thigh, volume reduction surgery and resection of excess skin on the thighs is required by ex-obese patients after major weight loss. Variable degrees of sagging and skinfold accumulation are also present, depending on the fat content. These deformities are included in the Pittsburgh Rating Scale1, and the patients, classified into one of three types, seek surgery to improve physical dynamics as well as hygiene, gain the freedom to wear certain clothing such as long pants, and achieve more pleasurable sexual performance and a balanced hip contour.
There are several techniques for deformity correction on the medial face of the thigh, but two deserve special attention for their pioneering and special abilities: the Lockwood technique4, which enables resection of excess fat in the upper third by fusiform incision in the inguinal crease, and the Lewis5,6 technique, which enables resection of excess adipose tissue in the dermal area of the upper third and part of the medium third by a sickle-shaped incision on the medial face of the thigh.
However, Lockwood4 and Lewis5,6 could not perform liposuction; hence, resections, in addition to being restricted to the upper third and middle part of the thigh, were restricted to cases of extreme local sagging. This study aims to associate the technique suggested by Cram & Aly2, for treatment of medial thigh deformities, with the Baroudi technique3, for resection of excess fat on the lateral thigh, provided this technique has been used for flankoplasties. Resection preceded by liposuction, especially in cases with residual fat, enable the removal of larger areas and placement of sutures without tension. Moreover, treatment of the lateral face of the thigh with liposuction and resection of the residual skinfold ensures a rounder contour to the thighs.
Despite the satisfaction expressed by patients with the results obtained, it was necessary to have a more objective assessment to prove the effectiveness of the proposed method. This was achieved by calculating thigh volumes before and after the surgery; the measurements demonstrated reduction in the size of the treated segment. The average volume reduction per thigh after surgery was a total of 1.135 cm3 at the postoperative period of 180 days. It seems obvious that any surgery performed on the medial aspect of thighs and complemented with lateral resection contributes to volume reduction; however, assessment of volume reduction by means of mathematical calculation reflects this truism.
The combined use of both techniques with liposuction enables the obtainment of a rounder hip contour, and results can be assessed by volume measurement. However, this method of measurement is limited, especially in patients with large skinfolds that are irregularly distributed along the thighs, as the cone body volume is assessed on the basis of the upper circumference in the inguinal crease and the lower circumference in the suprapatellar crease.
Future studies could employ the method proposed by Mayrovitz et al.7, which measures the development of lymphedema in the lower limbs, dividing them into segments and measuring the volume of each of these segments.
CONCLUSION
This study demonstrated, by geometric calculations, reduction in thigh volume after surgeries on the medial and lateral faces of the thigh. In eight patients who underwent thighplasty, there was an average volume reduction of 1,135 cm3 in each thigh, confirmed 180 days after the surgery.
The patients expressed satisfaction, reflected by broader deambulation movements, more effective hygiene, easier use of long pants, sexual performance enhancement, and more harmonious round contour of the thighs. The complications were minor and did not necessitate performance of more complex procedures.
REFERENCES
1. Song AY, Jean RD, Hurwitz DJ, Fernstrom MH, Scott JA, Rubin JP. A classification of contour deformities after bariatric weight loss: the Pittsburgh Rating Scale. Plast Reconstr Surg. 2005;116(5):1535-44.
2. Cram AE, Aly AS. Lower extremity body contouring after massive weight loss. In: Aly AS, ed. Body contouring after massive weight loss. St Louis: Quality Medical Publishing; 2006. p.213-36.
3. Baroudi R. Flankplasty: a specific treatment to improve body contouring. Ann Plast Surg. 1991;27(5):404-20.
4. Lockwood TE. Fascial anchoring technique in medial thigh lifts. Plast Reconstr Surg. 1988;82(2):299-304.
5. Lewis JR Jr. Correction of ptosis of the thighs: the thigh lift. Plast Reconstr Surg. 1966;37(6):494-8.
6. Lewis JR Jr. The thigh lift. J Int Coll Surg. 1957;27(3):330-4.
7. Mayrovitz HN, MacDonald J, Davey S, Olson K, Washington E. Measurement decisions for clinical assessment of limb volume changes in patients with bilateral and unilateral limb edema. Phys Ther. 2007;87(10):1362-8.
1. Specialist in plastic surgery, assistant physician at Hospital das Clínicas of the School of Medicine of Universidade de São Paulo (HCFMUSP), São Paulo, SP, Brazil.
2. Doctor of plastic surgery, assistant physician at HCFMUSP, São Paulo, SP, Brazil.
3. Full professor, associate professor of the Discipline of Plastic Surgery at the School of Medicine of Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil.
4. Undergraduate student of Medicine at FMUSP, São Paulo, SP, Brazil.
5. Full Professor at the Discipline of Plastic Surgery at FMUSP, São Paulo, SP, Brazil.
Correspondence to:
Rodrigo Itocazo Rocha
Rua Abílio Soares, 227 - cj. 101 - Paraíso
São Paulo, SP, Brazil - CEP 04005-000
E-mail: dritocazo@terra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: July 14, 2011
Accepted: August 9, 2011
Study conducted at Hospital das Clínicas of the School of Medicine of Universidade de São Paulo, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter