

Original Article - Year 2011 - Volume 26 -
Comparative study of the use of ethyl cyanoacrylate adhesive and intracutaneous suture for cutaneous excision closure
Estudo comparativo entre etilcianoacrilato e sutura intradérmica no fechamento de excisões cutâneas
ABSTRACT
BACKGROUND: The advantages of cyanoacrylates in cutaneous wound closure have been widely demonstrated in the literature. However, these products have not been widely used in Brazil due to the high costs of octyl cyanoacrylates. Moreover, there have been only a few studies on the most affordable product, ethyl cyanoacrylate, as a cutaneous adhesive. The objective of this study was to evaluate the efficacy of ethyl cyanoacrylate in cutaneous excision repair.
METHODS: A retrospective study conducted in patients with superficial skin lesions who underwent elliptical excision and repair by primary closure. The excisions were closed using deep relaxing sutures and either ethyl cyanoacrylate (case group; CaG) or intradermal suture (control group; CoG) on the skin surface.
RESULTS: Thirty-three patients were identified with 43 cutaneous lesions (CaG, n = 20; CoG, n = 23). Unsightly scars (CaG = 20%; CoG = 48%), eye irritation (CaG = 15%; CoG = 0), dehiscence (CaG = 5%; CoG = 0), infection (CaG = 0; CoG = 4.3%), and contact dermatitis (CaG = 0; CoG = 4.3%) were the problems observed. The cosmetic results were satisfactory in almost all excisions (CaG = 100%; CoG = 95.7%).
CONCLUSIONS: Ethyl cyanoacrylate was adequately tolerated in this study group, with no necrosis, allergic reactions, or infections. Ethyl cyanoacrylate presented several advantages over suture use, including low complication rates and high patient satisfaction.
Keywords: Tissue adhesives. Cyanoacrylates. Suture techniques.
RESUMO
INTRODUÇÃO: As vantagens dos cianoacrilatos em síntese cutânea têm sido sobejamente demonstradas na literatura. Entretanto, esses produtos têm sido subutilizados no Brasil, em decorrência dos elevados custos do octilcianoacrilato. Ademais, a forma mais economicamente acessível, etilcianoacrilato, tem sido pouco estudada como adesivo cutâneo. O objetivo deste estudo foi avaliar a eficiência do etilcianoacrilato na síntese de excisões cutâneas.
MÉTODO: Estudo retrospectivo realizado em pacientes portadores de lesões cutâneas superficiais submetidos a excisão elíptica e reparo por fechamento primário. As excisões foram fechadas por meio de suturas profundas relaxadoras e, na superfície da pele, foi utilizado etilcianoacrilato (grupo caso - GCa) ou sutura intradérmica (grupo gontrole - GCo).
RESULTADOS: Foram encontrados 33 pacientes portadores de 43 lesões cutâneas (GCa = 20 excisões; GCo = 23 excisões). Cicatrizes inestéticas (GCa = 20%; GCo = 48%), irritação ocular (GCa = 15%; GCo = 0), deiscência (GCa = 5%; GCo = 0), infecção (GCa = 0; GCo = 4,3%) e dermatite de contato (GCa = 0; GCo = 4,3%) foram os problemas encontrados. Os resultados cosméticos foram considerados satisfatórios na maioria das excisões (GCa = 100%, GCO = 95,7%).
CONCLUSÕES: O etilcianoacrilato foi adequadamente tolerado neste grupo de estudo, sem induzir necrose, reações alérgicas ou infecções, apresentando diversas vantagens de uso em relação à sutura, incluindo reduzido índice de complicações e grande satisfação dos pacientes.
Palavras-chave: Adesivos teciduais. Cianoacrilatos. Técnicas de sutura.
Cyanoacrylates have been the most commonly used tissue adhesives in the last 50 years, and their safety for use in cutaneous wound healing has been widely demonstrated in the literature1. However, these substances have seen limited use due to their high costs, including the surgical adhesive currently used almost exclusively in Brazil, 2-octyl cyanoacrylate (Dermabond®, Ethicon Inc., Somerville, New Jersey, United States)2.
Formulations of 2-ethyl cyanoacrylate (Aron Alpha, Permabond, Krazy Glue, Epiglu®) have been used with satisfactory results in dentistry, abdominal surgery, gynecology, gastroenterology, neurological surgery, maxillary surgery, orthopedics, plastic surgery, dermatology, urology, vascular surgery, cardiac surgery, thoracic surgery, and legal medicine1-9. Several clinical and experimental studies have shown the advantages of ethyl cyanoacrylate use as a skin adhesive, including biocompatibility, low cost, and wide availability2-4. However, there have been few reports of closure of excisional cutaneous wounds using ethyl cyanoacrylate1,8.
This study aims to fill this gap in knowledge by comparing the effectiveness of ethyl cyanoacrylate against intracutaneous suture for cutaneous excision closure.
METHODS
This retrospective study was performed by reviewing data from patients who underwent primary closure of skin wounds resulting from excision of superficial lesions. The procedures were carried out at Hospital Geral de Camaçari, Camaçari, BA, Brazil.
Exclusion criteria included clinical and/or laboratory evidence of allergy to ethyl cyanoacrylate components, blood dyscrasias, diabetes mellitus, alcoholism, severe nutritional deficiencies, coronary disease, hyperthyroidism, psychopathy, emotional instability, or use of immunosuppressive drugs. We also excluded lesions located in moist areas (armpits, perineum, and mucocutaneous junctions), lesions with edema, infected lesions, or lesions with signs of inflammatory disease. Finally, patients were also excluded if they chose not to undergo the excision or declined to provide informed consent.
Patients were divided into two groups, according to the cutaneous synthesis procedure they underwent. In the control group (CoG), lesions were sutured in two planes: the first subdermal, with simple inverted sutures covering the deep part of the dermis; the second dermal, with intradermal continuous sutures. In the case group (CaG), the closure planes were the same, but instead of the intradermal continuous suture, the wound was closed with ethyl cyanoacrylate adhesive (Figure 1).

Figure 1 - Surgical technique in the case group. A) Nevus in the lateral aspect of the left arm. B) Elliptic excision. C) Simple inverted point of subdermal suture. D) Completion of subdermal suture. E) Completion of intracutaneous suture. F) Radial spread of ethyl cyanoacrylate with a swab. G) Completion of skin gluing; notice the removal of the intracutaneous suture and translucent and corrugated aspect of the acrylic layer.
No prophylactic antibiotics were used and no occlusive dressings were applied in the CaG patients. Digital photographs were taken preoperatively and postoperatively for 90 days.
RESULTS
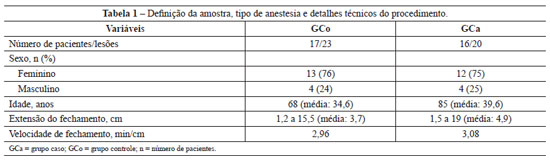
We selected 33 patients who underwent surgery between June 2005 and February 2010. The patient characteristics and technical details of the procedure are shown in Table 1.
Figures 2 to 5 show the location and diagnoses of the lesions, the incidence of postoperative complications, and the aesthetic results of surgery according to records of the patients' personal satisfaction level.
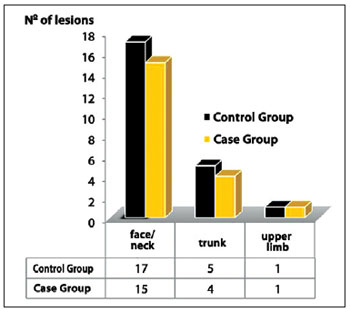
Figure 2 - Distribution of lesions.
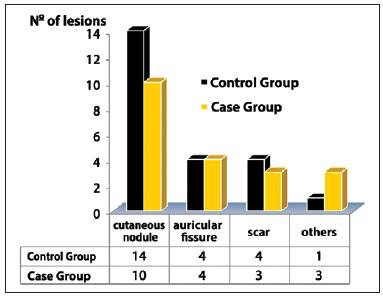
Figure 3 - Diagnosis of lesions.
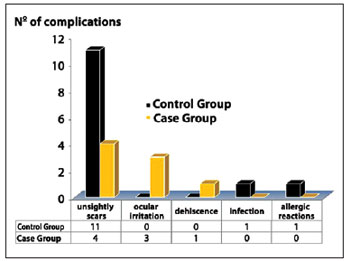
Figure 4 - Postoperative complications.
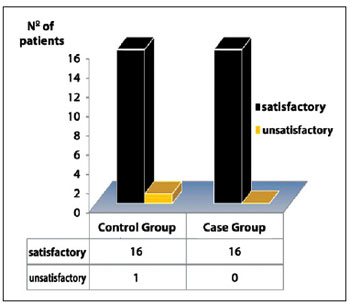
Figure 5 - Aesthetic results according to patients' personal satisfaction record.
Figures 6 to 8 illustrate some of the cases in this study.
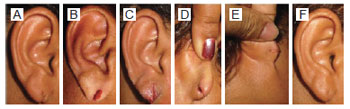
Figure 6 - Patient 33 years of age with fissure in the right auricular lobe, 2 cm in length, due to earring use. A) Preoperative aspect. B) Transoperative period. C) Immediate postoperative period. D) Postoperative period of 7 days with partial dehiscence. E) and F) Postoperative period of 3 months.

Figure 7 - Patient 65 years of age with nasal sebaceous cyst, 1 cm in diameter. A) Preoperative aspect. B) Transoperative period. C) Immediate postoperative period (arrow: tearing). D) Postoperative period of 3 months.

Figure 8 - Patient, 85 years of age, with cutaneous horn, 4 cm in diameter, in the left forearm. A) Preoperative aspect. B) Transoperative period. C) Immediate postoperative period. D) Postoperative period of 3 months.
DISCUSSION
Acute and chronic inflammation, cytotoxicity, necrosis, leukonychia, and allergic dermatitis are the major problems attributed to ethyl cyanoacrylate use on the skin, and such adverse effects have hampered its acceptance 2,10,11. However, these studies have small patient populations and the use of ethyl cyanoacrylate deserves further evaluation. Moreover, other studies have confirmed that the adverse effects of cyanoacrylate use are restricted to slight local complications, especially inflammation and partial dehiscence, which probably result from the surgery itself and not specifically from use of the adhesive1,4,12.
Several authors have shown that the main disadvantage of cyanoacrylates is cytohistotoxicity, as shown by cell lysis in vitro and inflammatory reactions in vivo1,3-5. The toxicity is attributed to the release of the degradation products formaldehyde and cyanoacetate. The short-chain cyanoacrylate derivatives show greater histotoxicity than long-chain derivatives because they are degraded more quickly. Ethyl cyanoacrylate generates a milder histotoxic response than do other short-chain cyanoacrylates or sutures4,5. The intensity of the inflammatory response triggered by cyanoacrylate does not affect its tensile strength13. The histotoxic effect is more pronounced in well-irrigated deep tissues; thus, cyanoacrylates are recommended for use only on non-vascular surfaces such as the skin4.
The use of ethyl cyanoacrylate as a cutaneous adhesive has been considered to be very safe owing to its low index of complications1,2. The low infection rates have been attributed to the low deposition of foreign bodies on the wound14. Studies show that the product is not carcinogenic5, and allergic reactions are extremely rare11. Ethyl cyanoacrylate has qualities that are common to other cyanoacrylates, such as resistance to the action of exudates, capacity to bear up to 500 g of traction, rapid polymerization and sealing, and bactericidal and hemostatic effects5,13. Several studies have recommended that ethyl cyanoacrylate should be more widely used, despite the availability of other possibly less toxic products, because it has distinct advantages in its lower cost, rapid elimination, and wide availability2-4,9.
This study demonstrated that cyanoacrylates can be used successfully in wounds anywhere in the body except (1) in areas of very tense skin such as over joints, unless deep relaxing sutures are placed; (2) in contaminated, exudative, bleeding, or infected wounds; (3 in lesions subjected to friction and moisture such as those in the plantar and palmar regions and in mucosal membranes, because there may be premature detachment of the adhesive; and (4) in patients with allergies to cyanoacrylate or its degradation products1,2.
The average patient age and the predominance of women in this study reflect the age group and gender most frequently affected by skin lesions caused by exposure to weather and surgical procedures. Experience has shown that most patients undergoing cutaneous excisions are aged 30 years and older, which is conventionally considered to be the age at which when aging begins15, and is also the age at which skin health declines. Women face the most pressure to maintain their appearance because of the demands of an obstinate society8,16.
The lesions in this investigation were those resulting in an open area that could be closed by direct suture under local anesthesia, without tension or distortion of the surrounding structures. The lesion characteristics were as follows: the depth of the lesion was restricted to the skin and subcutaneous plane, and the lesion had a maximum width of 3 cm on the face and neck and a maximum width of 5 cm on other parts of the body.
No antibiotics were used in the surgeries because there is evidence that antibiotic prophylaxis does not influence the occurrence of infection in sterile or potentially contaminated inpatient surgeries lasting up to 2 hours17,18.
Among the lesions treated in this study, those located on the face accounted for 75% of the CaG and 65% of the CoG, and included nevus (CaG = 35%; CoG = 26% of facial lesions), auricular lobe fissures caused by earrings (CaG = 20%; CoG = 17%), and non-diagnosed nodules due to lack of histopathological examination (CaG = 10%; CoG = 20%). As shown in Figure 2, few lesions were located on the trunk and upper limbs, and none in the lower limbs. Therefore, the results of this study should be applied to small benign facial lesions, but should not be extrapolated to lesions on the body extremities, especially the hands and feet.
The elliptical excision is the most common technique for skin lesions. If the ellipsis is too short, dog-ears are formed, which do not disappear spontaneously. To avoid this, the ellipsis should be two or three times the width of the cutaneous lesion15. Following this method, the widest excision performed in this study was 5 cm, which resulted in a scar with more than 15 cm of extension. No wider excisions were performed because they would be impossible to close by direct suture.
Long suture extensions can be closed with cyanoacrylates. Adhesives have been used on lacerations and cutaneous incisions of up to 50 cm, with results similar to closure with sutures1,2. In this study, the longest adhesive closure was for an excision of a xyphopubic hypertrophic scar, which resulted in a closure of 19 cm, within the limits recommended in the literature.
The average suture speed, using simple sutures separated by intervals of 2 mm, is about 1 min/cm, which is three times faster than the average speed in this study (3 min/cm). The longer time results from the need to close three planes: subdermal, by relaxing the shoulders of the lesion; intradermal, by sealing the cutaneous surface to prevent the entry of acrylate into the wound; and epidermal, by applying the surgical adhesive. Although closures of up to 5 cm of extension prolong the acceptable time (10 minutes), this is balanced by the benefits of the cyanoacrylates. Moreover, the smaller the wound and the greater the training of the surgical staff, the lower is the total time required for excision closure.
Placement of the subdermal suture is essential. In the authors' experience, excisions closed only with cyanoacrylates result in enlargement of the scar. This is likely because the surgical glue only joins the epidermal surface as a bridge, which enables the underlying dermis to suffer a gradual distancing, resulting in a larger scar in the late postoperative period2,19.
Clinical and experimental studies have suggested that commercial ethyl cyanoacrylate can be used for closure of surgical skin wounds1,3,6-8. In this case, special care should be taken to sterilize the cyanoacrylate prior to use. The packaging must be disinfected with ethylene oxide and confirmed by culture to be free of bacterial growth6. However, microbiological studies show that bacteria do not proliferate in the non-sterilized adhesive5.
The application of cyanoacrylates is relatively easy. The wound must be dry and relaxed by detachment of the edges or by deep sutures. A meticulous apposition of the edges is performed and two to three thin lines of the adhesive are spread over and around the lesion (5 mm to 10 mm). The tube should be squeezed carefully to avoid the product flowing into the wound. If the application is close to the patient's eyes, the eyes should be protected with gauze. Some precautions are necessary in the postoperative period to avoid premature loss of the adhesive. The wounds should be kept dry, although lesions can become moist even if they have not been rubbed or soaped. Swimming or other activities that cause intense perspiration should be avoided. Dressings are not necessary, and no ointment or dressing tapes should be placed directly on the adhesive1,2,8.
In this study, the cyanoacrylates considerably facilitated wound closure. The adhesive application was simple and rapid. After polymerization, the ethyl cyanoacrylate formed a flexible, translucent, and waterproof coating over the wound, avoiding the need for suture removal or dressing. This reduced the need for care, monitoring, and anesthetic use, resulting in lower postoperative costs. Moreover, the product can be up to four times cheaper than simple sutures and 30 times cheaper than 2-octyl cyanoacrylate2. Patients were able to wet the sutures from the day after the repair. The adhesive loosened completely and spontaneously between 4 and 8 days after surgery. Because needles were not used, there was no risk of puncture accidents. The instantaneous polymerization allowed the early formation of a mechanical barrier to prevent penetration of dirt, and loss of moisture from the wound, which shortened the surgical time, facilitated healing, and provided rapid keratinized epithelialization. These characteristics have been confirmed in the literature, and the use of cyanoacrylates is currently the method of skin closure with the highest patient satisfaction1.
Unsightly scars were the most common complications associated with this study, occurring in 48% (n = 11) of all CoG excisions and 20% (n = 4) of the CaG. Most of the unsightly scars occurred on the face (82% of CoG and 50% of CaG) and on the abdomen (13% of the CoG and 50% of the CaG). Unsightly scars occurred in all patients who underwent mid abdominal excisions. These observations suggest that the hypertrophies were not specifically derived from the use of cyanoacrylate, but to local characteristics, such as very mobile skin, inflammatory reactions against the relaxing subdermal sutures, and closures against force lines, which are unquestionably fibrogenic factors15. Unsightly scars were not attributed to the residual effect of the adhesive, and the rapid permanent contact of cyanoacrylate with the tissues may explain the lower inflammatory reaction triggered by adhesives compared with the sutures2. Interestingly, with one exception, all patients with unsightly scars (91% of the CoG and 100% of the CaG) were satisfied, because there was an improvement in the appearance compared with the previously treated scars.
The total complication index that the authors specifically attribute to the tissue adhesive or to intracutaneous suture was one dehiscence in CaG (5%) and one infection in CoG (4.4%). Dehiscence occurred after early accidental removal of the adhesive layer, resulting in a partial opening of the wound (Figure 6). Dehiscence is a constant concern with the use of cyanoacrylates and has been considered the most common complication after histotoxicity, with the incidence ranging from 0.3% and 26%. Dehiscence occurs mainly in wounds with irregular or traumatized edges, in lesions located in extremities, or in tensile skin zones without deep relaxing sutures1,2,11. The use of cyanoacrylates for high tension wounds is contraindicated because this adhesive can only achieve the tensile strength of 5-0 nylon sutures1,14,20.
The infection rate in the present study was similar to that reported in the literature (CaG = 0; CoG = 4.4%; other closure methods = 1.1%)1,14. Some publications report infection rates of between 1.5% and 2.9% for clean surgeries18. In our study, the infection occurred in an abdominal scar excision in an obese patient who had inadequate hygiene in CaG. The infection was treated with dressings, but resulted in formation of an unsightly hypertrophic scar that displeased the patient, and led to the single dissatisfied patient in this study selection. In clean wounds, the reported occurrence of infection is similar between sutures and cyanoacrylate (0.7% vs. 1.1%)1, but in contaminated lesions, cyanoacrylates demonstrate a pronounced bactericidal effect5,19. The exact mechanism by which this occurs remains unknown, but it is likely related to the cell wall because sensitivity to cyanoacrylates is restricted to gram-positive bacteria, including Staphylococcus aureus. It is possible that the strong electronegative charge of the polymer reacts with the cell wall of gram-positive bacteria, which has a positive charge. Gram-negative bacteria are relatively resistant because their lipopolysaccharide membrane isolates the cell wall. Cyanoacrylates also prevent deposition of foreign bodies in the wound, which enhances its bactericidal effect. It has been shown that sutures decrease the amount of contamination required to produce infections19.
This study confirmed that ethyl cyanoacrylate has a strong and unpleasant odor that may irritate the conjunctivae; however, the irritating effect does not seem to affect the buccal mucosa21,22. In this study, although the eyes were covered with bandages, a burning sensation or tearing occurred in 43% of excisions in which adhesive use was close to the eyes (3 of 7 excisions). Therefore, the authors suggest that application of cyanoacrylates should be avoided in periorbital regions1,8,10,22.
Cyanoacrylates have provided satisfactory aesthetic results, similar to those of sutures1,2. The appearance of scars remains the most important negative factor in evaluating aesthetic surgery23. The results of this study were consistent with these data. Only one patient in the CoG (4.6% of the lesions) was dissatisfied with the aesthetic result of the surgery due to the unfavorable appearance of a surgical scar. To obtain optimal results, proper selection of lesions to be treated and knowledge of specific technical aspects and the limitations of the adhesive in wound closure are important. Clinical studies reveal that the use of cyanoacrylates on the skin results in scars with an aesthetic appearance that is similar to that of intradermal sutures2.
The most significant outcomes of this study were the absence of the most feared complications of ethyl cyanoacrylate use (necrosis, infection, allergic reactions, and total dehiscence), together with the high level of satisfaction of patients submitted to cyanoacrylate closure (100%). These findings strongly suggest that cyanoacrylate is safe for use on the skin. Experimental studies suggest that necrosis induced by cyanoacrylates is limited to the methyl cyanoacrylate formulation1. Although rare, skin necrosis with ethyl cyanoacrylate is possible10. Application of the correct surgical technique, use on external areas of the skin relaxed by subdermal sutures, a short period of contact with the body's surface, and application of a minimum quantity of adhesive are all factors attributed to the good results observed three months after surgery. This result is predictive outcome at one year19.
CONCLUSIONS
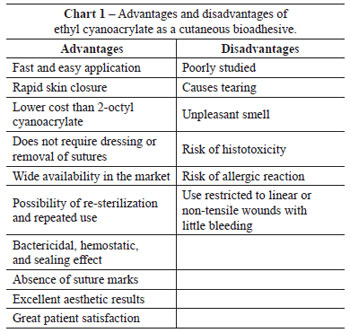
Compared with intracutaneous sutures, ethyl cyanoacrylate was shown to be safe and to achieve similar cosmetic results. Ethyl cyanoacrylate presented some advantages, including a low rate of complications and high levels of satisfaction for both patients and physicians (Chart 1).
REFERENCES
1. Singer AJ, Thode HC Jr. A review of the literature on octylcyanoacrylate tissue adhesive. Am J Surg. 2004;187(2):238-48.
2. Souza SC, Oliveira WL, Soares DF, Briglia CH, Athanázio PR, Cerqueira MD, et al. Comparative study of suture and cyanoacrylates in skin closure of rats. Acta Cir Bras. 2007;22(4):308-16.
3. Borba CC, Roubaud Neto E, Val RLR, Borba Jr CO, Soufen MA, Francisco Neto A, et al. Uso do cianoacrilato na síntese da pele de ratos - trabalho de pesquisa experimental. Acta Cir Bras. 2000;15(1):48-54.
4. Toriumi DM, Raslan WF, Friedman M, Tardy ME. Histotoxicity of cyanoacrylate tissue adhesives: a comparative study. Arch Otolaryngol Head Neck Surg. 1990;116(5):546-50.
5. Montanaro L, Arciola CR, Cenni E, Ciapetti G, Savioli S, Filippini F, et al. Cytotoxicity, blood compatibility and antimicrobial activity of two cyanoacrylate glues for surgical use. Biomaterials. 2001;22(1):59-66.
6. D'Assumpção EA. Cola de cianoacrilato de baixo custo em cirurgia plástica. Rev Soc Bras Cir Plast. 2008;23(1):22-5.
7. Souza SC, Briglia CH. Reparo de fissura de lóbulo auricular usando cola cirúrgica de menor custo. Rev Bras Cir Plast. 2010;25(4):715-8.
8. Souza SC, Briglia CH. Reparo de feridas cutâneas usando cola cirúrgica de baixo custo. An Bras Dermatol. 2011;86(1):435-42.
9. Alferes FCBA, Lyra MC, Orgaes FAFS, Leão Junior H, Gonella HA. Avaliação do etil-2-cianoacrilato (Epiglu®) na síntese de pele: estudo em ratos. Rev Bras Cir Plast. 2008;23(3):179-83.
10. Wang AA, Martin CH. Full-thickness skin necrosis of the fingertip after application of superglue. J Hand Surg Am. 2003;28(4):696-8.
11. Tomb RR, Lepoittevin JP, Durepaire F, Grosshans E. Ectopic contact dermatitis from ethyl cyanoacrylate instant adhesives. Contact Dermatitis. 1993;28(4):206-8.
12. Caloi TM, Manganello-Souza LC. Uso do cianoacrilato no fechamento cutâneo das queiloplastias primárias. Rev Soc Bras Cir Plast. 2005;20(2):108-11.
13. Tseng YC, Hyon SH, Ikada Y, Shimizu Y, Tamura K, Hitomi S. In vivo evaluation of 2-cyanoacrylates as surgical adhesives. J Appl Biomater. 1990;1(2):111-9.
14. Quinn J, Wells G, Sutcliffe T, Jarmuske M, Maw J, Stiell I, et al. A randomized trial comparing octylcyanoacrylate tissue adhesive and sutures in the management of lacerations. JAMA. 1997;277(19):1527-30.
15. Weinzweig J. Plastic surgery: secrets plus. 2nd ed. Philadelphia: Mosby Elsevier; 2010.
16. Avelar JM. Contribuições à cirurgia plástica. São Paulo: Hipócrates; 2001.
17. Reese RE, Betts RF, Gumustop B. Manual de antibióticos. 3ª ed. Rio de Janeiro:Guanabara-Koogan;2002.
18. Dias GA. Antibioticoterapia profilática e/ou terapêutica em pacientes submetidos à cirurgia plástica estética: uma necessidade? Rev Bras Cir Plast. 2010;25(3):423-7.
19. Blondeel PN, Murphy JW, Debrosse D, Nix JC 3rd, Puls LE, Theodore N, et al. Closure of long surgical incisions with a new formulation of 2-octylcyanoacrylate tissue adhesive versus commercially available methods. Am J Surg. 2004;188(3):307-13.
20. Bernard L, Doyle J, Friedlander SF, Eichenfield LF, Gibbs NF, Cunningham BB. A prospective comparison of octyl cyanoacrylate tissue adhesive (dermabond) and suture for the closure of excisional wounds in children and adolescents. Arch Dermatol. 2001;137(9):1177-80.
21. Quinn J, Maw J, Ramotar K, Wenckebach G, Wells G. Octylcyanoacrylate tissue adhesive versus suture wound repair in contaminated wound model. Surgery. 1997;122(1):69-72.
22. Kine BB, Novak RW, Rohm and Haas Company. 2-cyanoacrylics ester polymers. In: Encyclopedia of chemical technology: A to alkanolamines. 3rd ed. vol. 1. New York: John Wiley & Sons; 1978. p. 408-13.
23. Ferreira MC. Cirurgia plástica estética: avaliação de resultados. Rev Soc Bras Cir Plast. 2000;15(1):55-61.
1. Full member of the Brazilian Society of Plastic Surgery (SBCP), Plastic Surgeon at the Clinic of Faculdades Adventistas da Bahia, Cachoeira, BA, Brazil.
2. Associate member of SBCP, Plastic Surgeon at Hospital Geral de Camaçari, Camaçari, BA, Brazil.
Correspondence to:
Sandro Cilindro de Souza
BR 101, km 197 - Caixa Postal 18
Cachoeira, BA, Brazil - CEP 44300-000
E-mail: sandrocilin@ig.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: August 25, 2011
Paper accepted: October 10, 2011
Study conducted at Hospital Geral de Camaçari, Camaçari, BA, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter