

Original Article - Year 2011 - Volume 26 -
Analysis of the incidence of pressure ulcers at Hospital Metropolitano de Urgência e Emergência in Ananindeua, PA
Análise da incidência de úlcera de pressão no Hospital Metropolitano de Urgência e Emergência em Ananindeua, PA
ABSTRACT
BACKGROUND: Pressure ulcers are one of many complications to which hospitalized patients are susceptible. Such ulcers may lead to partial or total destruction of cutaneous, subcutaneous, and muscular tissues, as well as of bones and articulations.
METHODS: An observational, longitudinal, and prospective study was carried out at Hospital Metropolitano de Urgência e Emergência em Ananindeua, PA, Brazil. Relevant data related to gender, age (younger or older than 60 years old), impairment degree, and region of pressure ulcer impairment were collected from Intensive Care Therapy 1 (UTI 1), Surgical Clinic 1, and the Neuro Clinic.
RESULTS: Among 474 studied patients, 17 developed pressure ulcers, with greater incidence among male patients (88.2%), at stage II (41.2%) and in the sacral region (40%). Patients aged more than 60 years had an incidence rate of 58.8% for pressure ulcers.
CONCLUSIONS: Data obtained in this study are in accordance with the results presented in the literature. It is important to highlight the need for creating risk scales and preventive measures for decreasing the incidence of pressure ulcers in hospitals.
Keywords: Pressure ulcer/epidemiology. Skin ulcer. Incidence.
RESUMO
INTRODUÇÃO: A úlcera de pressão configura-se como uma das diversas complicações às quais pacientes hospitalizados estão suscetíveis, podendo levar à destruição parcial ou total de estruturas como tecidos cutâneo, subcutâneo e muscular, ossos e articulações.
MÉTODO: Estudo do tipo observacional, longitudinal, prospectivo, desenvolvido no Hospital Metropolitano de Urgência e Emergência em Ananindeua, PA, Brasil. Foram coletados dados pertinentes às variáveis sexo, idade (maior ou menor que 60 anos), grau de acometimento e local de acometimento das úlceras de pressão, nos setores Unidade de Terapia Intensiva 1 (UTI 1), Clínica Cirúrgica 1 e Neuroclínica.
RESULTADOS: Dentre os 474 pacientes estudados, 17 desenvolveram úlcera de pressão, com maior incidência no sexo masculino (88,2%), em estágio II (41,2%) e na localização sacral (40%). Pacientes com mais de 60 anos de idade apresentaram incidência de 58,8% de úlcera de pressão.
CONCLUSÕES: Os dados obtidos neste estudo estão de acordo com os resultados apresentados na literatura. Ressalta-se a necessidade de criação de escalas de risco e medidas preventivas para diminuir a incidência de úlceras de pressão nos hospitais.
Palavras-chave: Úlcera por pressão/epidemiologia. Úlcera cutânea. Incidência.
Pressure ulcers, decubitus ulcers, or eschars are lesions that may affect cutaneous and subcutaneous tissues, often affecting muscular tissue and even bones and articulations, leading to partial or total destruction of these structures. They are common in patients who are bedridden for long periods and deprived of movement, which leads to tissue compression conditions, ischemic lesions, and consequent necrosis1.
Pressure ulcers can be superficial or deep, of ischemic etiology (secondary to an increase in external pressure, tangential tension, friction, or a combination of these factors), and are usually located on bony prominences2.
The physiopathogeny is derived from a complex phenomenon involving several factors related to the patient and his or her external environment, including a hospital's physical structure, resources, supplies, and the attitudes of multidisciplinary professionals toward the patient and the procedures they follow3.
Pressure ulcers are complications that arise in critically ill hospitalized patients, especially those who are exposed to numerous risk factors for developing this type of lesion during prolonged surgical procedures4. Critically ill patients are those who have severe clinical conditions or require frequent and specialized care associated with more complex therapies, whether invasive or noninvasive5.
The World Health Organization (WHO) uses the incidence and prevalence of pressure ulcers as an indicator to determine the quality of care provided in healthcare services. According to the WHO, approximately 95% of pressure ulcers can be avoided by adopting special measures.
According to the National Pressure Ulcer Advisory Panel (NPUAP), the prevalence of pressure ulcers in North American hospitals ranges from 3-14%, and increases to 15-25% in cases where patients are on strict bed rest5.
In Brazil, there are not enough data on the national incidence and prevalence of pressure ulcers. Related studies are restricted to specific regions and cities, and limited to a few hospital sectors5.
In advanced stages, pressure ulcer treatment may be protracted and expensive; in some cases, surgical intervention is required. In Brazil, there are no precise data in the literature related to costs associated with pressure ulcers within the healthcare system. However, international studies demonstrate that each lesion may cost from 2,000 to 30,000 dollars, and may even reach 1.3 billion dollars a year6.
METHODS
This was an observational, longitudinal, and prospective study developed at Hospital Metropolitano de Urgência e Emergência in Ananindeua, PA, Brazil. The research project followed legal procedures determined by Resolution 196/96 of the National Health Council with regard to research involving human beings. Immediately following analysis and approval by the Ethics in Research Committee of the Health Sciences Institute, the project was assessed and approved by the Ethics in Research Commission of HMUE. Data collection began shortly thereafter.
The research setting for this study was Intensive Care Unit 1 (UTI 1), Surgical Clinic 1, and the Neuro Clinic at HMUE. UTI 1 has 10 beds, Surgical Clinic 1 has 24 beds, and the Neuro Clinic has 26 beds. The sample was established based on different patient profiles in each studied sector, with the purpose of obtaining a representative population of the hospital as a whole. The research was based on data relevant to the incidence of pressure ulcers at HMUE in each studied sector. Therefore, patient identification variables were used, such as gender, age (older or younger than 60 years old), and degree and region of pressure ulcer impairment.
The study population of both males and females included 115 patients from UTI 1, a total of 170 patients from Surgical Clinic 1, and 189 patients from the Neuro Clinic who were hospitalized at HMUE between May and October 2009. The sample included international patients and participants were selected based on the following inclusion criteria: patients hospitalized in UTI 1, the Surgical Clinic 1 and the Neuro Clinic during the study period. The research excluded patients who: (a) had pressure ulcers at admission, regardless of impairment region and degree; (b) were hospitalized in one of the study sectors for less than 48 hours; and (c) did not consent to participation in the research.
The obtained results were organized in Microsoft Excel 2003 worksheets and were analyzed using Epi Info (v. 3.5.1) and BioEstat (v. 5.0) software. A descriptive data analysis to determine ulcer frequency was performed. The inferential statistical association analysis was based on Fisher's exact test.
RESULTS
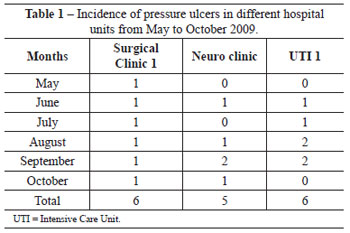
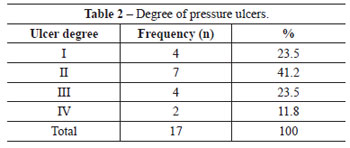
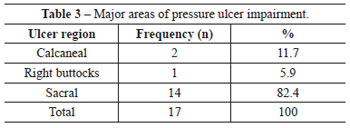
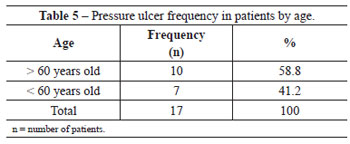
The data analysis from the study protocol implementation yielded a total sample of 474 patients, with 2 deaths recorded in the Neuro Clinic during the data collection period. Of the total number of patients, 170 were from Surgical Clinic 1, 189 were from the Neuro Clinic, and 115 were from UTI 1. During the study period, 17 (3.6%) patients developed pressure ulcers, of which 6 (35.3%) were from Surgical Clinic 1, 5 (29.4%) were from the Neuro Clinic, and 6 (35.3%) were from UTI 1. Table 1 presents the distribution of pressure ulcer incidence in the respective months in each studied sector. Table 2 demonstrates greater prevalence of grade II over other degrees of pressure ulcers, with the sacral region being the most frequent, corresponding to 82.4% of the total (Table 3). With regard to gender, there was no statistically significant pattern that could enable a correlation with pressure ulcers (Table 4). However, a greater incidence of pressure ulcers occurred in patients aged more than 60 years (Table 5).
DISCUSSION
With respect to the incidence of pressure ulcers, it is possible to verify similar distributions within the different hospital units studied at HMUE. However, the study did not consider the admission time for each patient in order to assess correlation with pressure ulcer incidence, a variable that shall be analyzed in future studies. Nonetheless, it is possible to infer that, as they are environments in which admitted patients require longer hospitalization and medical care, both UTI 1 and Surgical Clinic 1 are more vulnerable sectors for the occurrence of pressure ulcers.
Previous studies demonstrate that the incidence of pressure ulcers in patients hospitalized at UTI in Brazil ranges from 10.6% to 55%7. Also, there are reports that the incidence of pressure ulcers in neuropathy patients ranges from 7.5% to 31.7%8. In a study conducted at Hospital Universitário of the Universidade de São Paulo, it was verified that the incidence of pressure ulcers in the surgical clinic corresponds to 36.5%9.
With regard to the incidence of pressure ulcers by gender, it was verified that, out of the 472 treated patients, 17 had pressure ulcers, including 15 males and 2 females, corresponding to a 4.0% and 1.9% incidence rate for males and females, respectively. Among patients who developed pressure ulcers, 88.2% were male, while 11.2% were female. However, this variable was not statistically significant (P = 0.2438); thus, it is unclear whether gender is a factor contributing to the genesis of pressure ulcers. These findings corroborate data from other studies; although pressure ulcers have been found to be more prevalent among male patients (57.7%) than females (42.3%), the results are not statistically significant5,10.
In this study, it was verified that the most common degree of pressure ulcer was grade II, representing 41.2% of the total. Moreover, the sacral region (82.4%) was most the common region for pressure ulcer development. Trochanteric pressure ulcers were not found in any patients, although Blanes et al.5 identified them as major impairment regions. The literature also reports a greater incidence of stage II pressure ulcers (57.16%) compared to later stages among patients hospitalized at Hospital São Lucas11. Blanes et al.5 found a greater incidence of sacral pressure ulcers (40%) among hospitalized patients.
In addition, it was observed that, among the patients who developed pressure ulcers, 41.2% were 60 years or older. Bryant et al.12 attributed the greater vulnerability for elderly individuals to develop pressure ulcers to the fact that this group of patients has decreased subcutaneous and muscular cellular tissues compared to younger patients.
CONCLUSIONS
The results of this study support previous findings in the literature reflecting high incidence rates for pressure ulcers, which is a problem in healthcare. Much discussion has centered on measures to be adopted for preventing pressure ulcers, which should be a top priority for hospitals. These measures include equipping hospital sectors with resources for relieving pressure zones, and for monitoring the risk degree, incidence, and prevalence of pressure ulcers. These should be the first steps for implementing prevention protocols and for raising staff awareness about problems associated with pressure ulcers.
The authors of the study suggest adopting prevention measures and preparing a research protocol compatible with our needs. The adoption of such measures may, in the medium and long term, result in cost savings for hospitals, which could then be used for the purchase of technical equipment and/or investments in other sectors that could further enhance patient well-being.
REFERENCES
1. Moura CEM, Silva LLM, Godoy JRP. Úlceras de pressão: prevenção e tratamento. Univ Ci Saúde. 2005;3(2):275-86.
2. Ferreira LM, Calil JA. Etiopatogenia e tratamento das úlceras por pressão. Diagn Tratamento. 2001;6(3):36-40.
3. Lidgren M, Unosson M, Krantz AM, Ek AC. Pressure ulcer risk factors in patients undergoing surgery. J Adv Nurs. 2005;50(6):605-12.
4. Fernandes NCS, Torres GV. Ulcers of pressure in patients of intensive therapy unit: incidence and association of risk factors. FIEP Bulletin. 2006;76(2):55-8.
5. Blanes L, Duarte IS, Calil JA, Ferreira LM. Avaliação clínica e epidemiológica das úlceras por pressão em pacientes internados no Hospital São Paulo. Rev Assoc Med Bras. 2004;50(2):182-7.
6. Diccini S, Camaduro C, Iida LIS. Incidência de úlcera de pressão em pacientes neurocirúrgicos de hospital universitário. Acta Paul Enferm. 2009;22(2):205-9.
7. Fernandes NCS, Torres GV. Incidência e fatores de risco de úlceras de pressão em pacientes de unidade de terapia intensiva. Ciênc Cuid Saúde. 2008;7(3):304-10.
8. New PW, Rawicki HB, Bailey MJ. Nontraumatic spinal cord injury rehabilitation: pressure ulcer patterns, prediction, and impact. Arch Phys Med Rehabil. 2004;85(1):87-93.
9. Rogenski NMB, Santos VLCG. Estudo sobre a incidência de úlceras por pressão em um hospital universitário. Rev Latino-am Enfermagem. 2005;13(4):474-80.
10. Fernandes NCS. Úlceras de pressão: um estudo com pacientes de Unidade de Terapia Intensiva [dissertação de mestrado]. Natal: Universidade Federal do Rio Grande do Norte, Centro de Ciências da Saúde; 2005. 155 p.
11. Silva SS, Millidiú V, Urbanetto JS, Gustavo AS, Graziela Hax G. Indicador assistencial de enfermagem: incidência de úlcera de pressão em adultos hospitalizados. Rev Graduação PUCRS. 2008;1(1). Disponível em
12. Bryant RA, Shannon ML, Pieper B, Braden BJ, Morris DJ. Pressure ulcers. In: Bryant RA, ed. Acute and chronic wounds: nursing management. St Louis: Mosby; 1992. p. 105-63.
1. Physician graduated at Universidade Federal do Pará (UFPA), Belém, PA, Brazil.
2. Doctor in Plastic Surgery at Universidade Federal do Rio de Janeiro (UFRJ), associate professor of Surgical Technique and Experimental Surgery at UFPA, plastic surgeon at Hospital Metropolitano de Urgência e Emergência, full member of the Brazilian Society of Plastic Surgery, Belém, PA, Brazil.
3. Medical student at UFPA, Belém, PA, Brazil.
Correspondence to:
Daniel Augusto dos Santos Soares
Travessa Djalma Dutra, 1.031
Belém, PA, Brazil - CEP 66113-010
E-mail: dandan_soares@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: July 16, 2011
Paper accepted: October 13, 2011
Study conducted at Hospital Metropolitano de Urgência e Emergência, Ananindeua, PA, Brazil.



 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter