

Original Article - Year 2011 - Volume 26 -
Facial paralysis: epidemiological analysis in a rehabilitation hospital
Paralisia facial: análise epidemiológica em hospital de reabilitação
ABSTRACT
BACKGROUND: Facial paralysis is characterized by permanent or temporary loss of facial expression due to facial nerve injury. Several factors influence the development of facial nerve lesions. The purpose of this study was to evaluate the epidemiological aspects and incidence of sequelae after facial paralysis at a rehabilitation institution.
METHODS: We performed a retrospective study of facial paralysis patients admitted to a rehabilitation hospital between January 2001 and January 2005. Sequelae were analyzed according to gender, age, etiology, functional status as measured by the House-Brackmann scale, evaluation time, follow-up, and surgical procedures. Statistical analyses were performed with Epi-info 3.2.2 software.
RESULTS: A total of 285 facial paralysis patients, 157 male and 128 female, were admitted for a rehabilitation program. All subjects followed a rehabilitation program, and 29 (10.2%) underwent surgery; 80% were admitted during the 3rd week of the paralysis or later, and 121 (42.5%) showed gradual recovery after 3 months, either spontaneously or after clinical or physical therapies. Nevertheless, 119 (41.8%) sustained irreversible partial or complete facial paralysis.
CONCLUSIONS: The prevalence of facial paralysis was greater among patients younger than 20 years. Among these patients, paralysis had different causes, and these patients were admitted with lower House-Brackmann grades. Most cases were associated with neurological deficits leading to facial paralysis of central or congenital origin.
Keywords: Facial paralysis. Facial nerve injuries. Facial nerve diseases.
RESUMO
INTRODUÇÃO: A paralisia facial é a perda temporária ou permanente dos movimentos da mímica facial em decorrência do acometimento do nervo facial. São vários os fatores que influenciam a evolução das lesões do nervo facial. Este estudo teve como objetivo avaliar os aspectos epidemiológicos e a frequência de sequelas após paralisia facial em um serviço de reabilitação.
MÉTODO: Estudo retrospectivo dos pacientes com paralisia facial atendidos em hospital de reabilitação no período de janeiro de 2001 a janeiro de 2005. As sequelas foram avaliadas quanto a sexo, idade, etiologia, graduação funcional conforme a escala de House-Brackmann, tempo de evolução, seguimento e intervenções cirúrgicas. Para realização da análise estatística utilizou-se o programa Epi-Info versão 3.2.2.
RESULTADOS: Foram admitidos para programa de reabilitação 285 pacientes portadores de paralisia facial, sendo 157 do sexo masculino e 128 do feminino. Todos os pacientes se submeteram a programa de reabilitação e 29 (10,2%), a cirurgia. Dentre os pacientes analisados, 80% foram admitidos a partir da terceira semana do surgimento da paralisia, e 121 (42,5%) tiveram recuperação gradual em 3 meses, espontaneamente, com tratamento clínico ou fisioterápico. Por outro lado, 119 (41,8%) pacientes permaneceram com paralisia facial parcial ou completa e irreversível.
CONCLUSÕES: Os casos admitidos foram mais frequentes em pacientes com menos de 20 anos de idade, com causas diversas e quando admitidos em graus menores segundo a escala de House-Brackmann, pois muitos deles se associavam a déficits neurológicos consequentes a paralisia facial de origem central ou congênita.
Palavras-chave: Paralisia facial. Traumatismos do nervo facial. Doenças do nervo facial.
The facial nerve is vulnerable to lesions and subsequent facial paralysis. Several causes for facial paralysis have been presented in the literature. In two-thirds of the cases, the cause is unknown. These cases are referred to as cases of idiopathic paralysis or Bell's palsy1,2. In facial paralysis, alterations occur in the facial expression muscles depending on the level of the facial nerve lesion. In most cases, this is a spontaneously reversible phenomenon or is reversed after some type of treatment, either clinical or surgical. However, about 20% of patients develop some type of sequelae, which range from a light degree of paralysis to unilateral or bilateral complete paralysis of facial muscle movements3,4.
Currently, lesions resulting in facial paralysis are difficult to treat and may cause facial expression alterations, with serious emotional consequences5. To minimize sequelae, it is important to understand the causes and factors that could influence disease evolution.
The purpose of this study was to analyze the epidemiological aspects and incidence of sequelae after facial paralysis at a rehabilitation institution.
METHODS
This is a retrospective study of patients with facial paralysis admitted to the Rede SARAH de Hospitais de Reabilitação in Brasília (DF, Brazil) between January 2001 and January 2005. Information on gender, age, etiology, time of evolution, follow-up, recurrences, sequelae, and interventions was obtained from patients' medical records. The degree of dysfunction was determined using the House-Brackmann6 scale upon admission and discharge. The study was assessed and approved by the Ethics Committee of the institution.
Rehabilitation Program
The patients were admitted by a multi-specialty staff. The program consisted of diagnosis using imaging and electromyography examinations and clinical treatment with corticosteroids and antiviral drugs in cases of idiopathic origin or the Ramsay-Hunt syndrome. The preventive measures employed for corneal lesions were glasses, eye drops, ophthalmic ointments, and eye occlusion. Finally, the rehabilitation program included performance of guided physiotherapy exercises7.
For patients with irreversible House-Brackmann grades V and VI paralyses lasting more than 2 years, surgical rehabilitation was recommended. Patients who had no contraindications and who were able to comprehend and provide consent to surgery underwent neurorrhaphy, nerve and muscular transference, or eyelid canthoplasty.
Statistical Analysis
To carry out the statistical analysis, we used the STATCALC package of Epi-Info version 3.3.2 (Epi-Info, Centers for Disease Control, Atlanta, GA, USA) with confidence intervals of 95%. Relative risk was assessed with values of P < 0.05, and Fisher's exact test was applied.
RESULTS
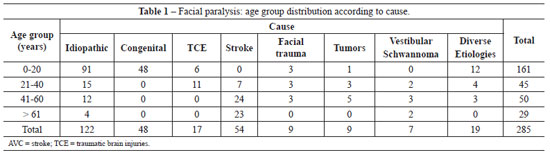
Between January 2001 and January 2005, 285 patients (157 men and 128 women) with facial paralysis were admitted to the rehabilitation hospital in Brasília. Data were obtained from the medical records, and information for 45 (15.8%) patients was incomplete. Causes of facial paralysis and patient ages are described in Table 1. We observed 122 (42.8%) cases of paralysis with idiopathic or Bell's palsy characteristics, 48 (16.8%) of congenital paralysis, 17 (6%) deriving from traumatic brain injuries, 54 (18.9%) due to stroke, 9 (3.2%) due to facial trauma, 9 (3.2%) due to tumors, 7 (2.4%) due to vestibular schwannoma, and 19 (6.7%) due to other etiologies (Table 1).
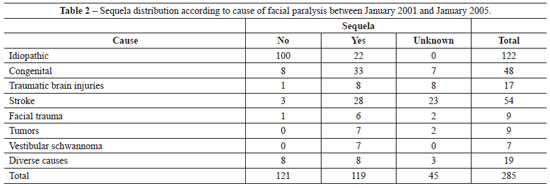
In Table 2, the incidence of sequelae is presented according to the cause of facial paralysis.
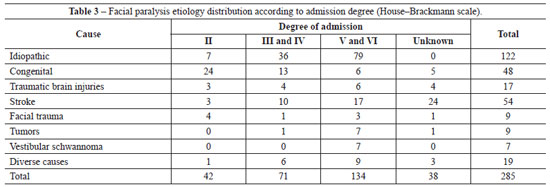
Among patients admitted with facial paralysis, 79 (64.8%) patients with idiopathic causes had House-Brackmann grades V and VI; 24 (50%) with congenital causes had grade II; and 7 (77.8%) with tumors, 7 (100%) with vestibular schwannomas, and 9 (47.4%) patients with different causes had grades V and VI (Table 3).
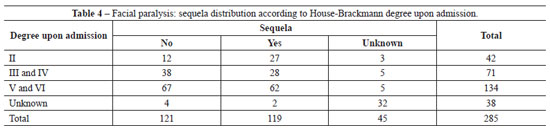
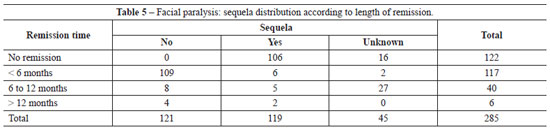
A total of 228 (80%) patients were admitted during the third week of symptoms and signs of facial paralysis, with an average follow-up period of 18 months. Among these patients, 121 (42.5%) showed gradual recovery between 6 and 12 months. Recovery was achieved through clinical treatments such as administration of corticosteroids or antiviral drugs, or through physiotherapy; in some cases, recovery was spontaneous. In 119 patients (41.8%), the recovery was partial or the facial paralysis was irreversible (Tables 4 and 5). Fifty-eight patients (20.4%) had total facial paralysis, and 6 (2.32%) had more than 1 episode of paralysis without any sequelae.
Variables that influenced the development of sequelae were age group (relative risk (RR) of 0.58 (0.45; 0.74) with P = 0.00002), House-Brackmann grades II and III upon admission (RR of 1.5 (1.17; 1.96) with P = 0.007), congenital causes, and stroke sequelae.
All patients underwent a rehabilitation program, and 29 (10.2%) underwent surgery. Lateral canthoplasty was performed for ocular protection in 12 patients with partial paralysis associated with cognitive deficits, clinical or psychological contraindications, or when the patient did not want to undergo the surgical reanimation procedure.
Surgical rehabilitation was indicated in cases of irreversible paralysis with a duration of more than 2 years. End-to-end micro-neurorrhaphy was performed for 2 patients; hypoglossofacial anastomosis was performed for 4, temporal muscle transposition for 7, canthoplasty for 12, and complementary procedures for 4 patients. Among the operated patients, 27 recovered by at least one grade in the House-Brackmann classification, and only 3 patients remained as grade V. These patients were over 60 years old and had late lesions after vestibular schwannoma resection and stroke sequelae.
DISCUSSION
As observed in this study and corroborating literature data, the most common clinical course of facial paralysis is sudden onset, preceded by dysesthesia, epiphora, hyperacusis, and lacrimal alterations. Together, these clinical signs indicate idiopathic paralysis or Bell's palsy1,2,6,7.
A literature review shows that the incidence of idiopathic paralysis is 20 cases per 100,000 individuals per year2. In this report, we found an incidence of 122 cases in 5 years, or an average of 20 cases per year. Of these patients, 80% recovered facial function in less than 1 year. Similar results were reported by Peitersen8 in a study that included 2,570 cases. In this study, 85% of the patients recovered function within 3 weeks and 15% recovered function after 3 to 5 months. In the present study, we observed mild sequelae in 12% of the patients, moderate in 13%, and severe in 4%. In this case selection, the incidence of House-Brackmann grades V and VI was 67%. Twenty percent of the patients remained in this classification, i.e., in a serious condition, and surgery was indicated for 10% of these patients.
It was not possible to analyze the effects of clinical treatment or surgical decompression, because 95% of the patients were admitted 3 weeks after the onset of symptoms, and clinical treatment had already been administered in other services, without defined therapeutic protocols. Studies suggest that among adult patients, the use of corticosteroids with acyclovir is related to a better functional recovery. This treatment could be prescribed within 7 days of symptom onset, with better results observed when used within 4 days of onset7-12.
Two major causes of facial paralysis were brain lesions and congenital lesions. All 48 cases of congenital paralysis were observed in patients younger than 20 years. In this group, as well as in that assessed by Kobayashi (see Stamm13), the most common type of congenital paralysis was isolated unilateral paralysis of the lower lip. Bilateral congenital facial paralysis, which is less frequent, can be caused by Moebius syndrome. This syndrome affects many cranial nerves, including the VII pair, the oculomotor, trigeminal, and especially the hypoglossal nerve14. We observed 4 cases of Moebius syndrome in this report.
Patients with central causes of facial paralysis comprised the third group. The major cause of central facial paralysis is vascular, secondary to stroke4. For differential diagnosis between central facial paralysis and peripheral facial paralysis, the presence of other neurological symptoms and alterations noted upon physical examination are considered, especially partial impairment of the lower third of the face. It is difficult to perform prolonged follow-up for these patients, because many are admitted for brain lesion rehabilitation and family training and are clinically followed through other services.
Among the several causes of facial paralysis, rare syndromes are found, with associated malformations and greater chance of sequelae. In Ramsay Hunt syndrome, observed in 6 patients, the time of remission was greater than 12 months. Four patients had sequelae, in agreement with the observations of Sweeney & Gilden15. According to Sweeney and Gilden, Ramsay Hunt patients with sequelae show less recovery.
All patients were admitted to the physiotherapy program. The real value of physiotherapy has not been demonstrated in several studies. However, physiotherapy seems to benefit treatment by avoiding deformities and maintaining flexibility and muscular elasticity during the paralysis period, particularly in cases of Bell's palsy. Specific exercises can be indicated when attempts to move the impaired muscles are observed, and during the postoperative follow-up of transference of nerve or muscles, with the aid of biofeedback devices. These devices do not interfere with the recovery speed, and may improve function. They may also provide emotional support during the evolutionary phases of the paralysis16.
Surgical rehabilitation is indicated for patients with irreversible paralysis and more than 2 years of lesion duration. Although surgical rehabilitation was possible in 10% of the patients, Labbé et al.17 showed that restoring full symmetrical facial expression is almost impossible, even using a single surgical protocol. Several factors may influence the results, such as age, clinical condition, etiology, degree of lesion, tissue vascularization and, above all, level of the lesion and paralysis duration.
CONCLUSIONS
This was a retrospective study in which 49% of patients were found to have irreversible facial paralysis. The variables that influenced evolution of sequelae were age, House-Brackmann grades II and III upon admission, congenital causes, and stroke sequelae.
REFERENCES
1. Atkin PA. Diagnosis and management of Bell's palsy. Practitioner. 2003;247(1642):36,39,42-3.
2. Valença MM, Valença LPAA, Lima MCM. Paralisia facial periférica idiopática de Bell: a propósito de 180 pacientes. Arq Neuropsiquiatr. 2001;59(3B):733-9.
3. Vlastou C. Facial paralysis. Microsurgery. 2006;26(4):278-87.
4. Lazarini PR, Fouquet ML. Paralisia facial: avaliação, tratamento e reabilitação. São Paulo: Lovise; 2006.
5. Stuart RM, Byrne PJ. The importance of facial expression and the management of facial nerve injury. Neurosurg Q. 2004;14(4):239-48.
6. House JW. Facial nerve grading systems. Laryngoscope. 1983;93(8):1056-69.
7. Informações sobre doenças tratadas: paralisia facial periférica. Disponível em: www.sarah.br. Acesso em: 20/10/2007.
8. Peitersen E. Bell's palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl. 2002;549:4-30.
9. Uri N, Greenberg E, Kitzes-Cohen R, Doweck I. Acyclovir in the treatment of Ramsay Hunt syndrome. Otolaryngol Head Neck Surg. 2003;129(4):379-81.
10. Ramsey MJ, DerSimonian R, Holtel MR, Burgess LP. Corticosteroid treatment for idiopathic facial nerve paralysis: a meta-analysis. Laryngoscope. 2000;110(3 Pt 1):335-41.
11. Beurskens CH, Heymans PG. Physiotherapy in patients with facial nerve paresis: description of outcomes. Am J Otolaryngol. 2004;25(6):394-400.
12. Salinas RA, Alvarez G, Alvarez MI, Ferreira J. Corticosteroids for Bell's palsy (idiopathic facial paralysis). Cochrane Database Syst Rev. 2002;(1):CD001942.
13. Stamm AC. Paralisia facial congênita: avaliação e conduta. Rev Bras Otorrinolaringol. 1985;51(3).
14. Kahane JC. Pathophysiological effects of Möbius syndrome on speech and hearing. Arch Otolaryngol. 1979;105(1):29-34.
15. Sweeney CJ, Gilden DH. Ramsay Hunt syndrome. J Neurol Neurosurg Psychiatry. 2001;71(2):149-54.
16. Beurskens CH, Heymans PG. Positive effects of mime therapy on sequelae of facial paralysis: stiffness, lip mobility, and social and physical aspects of facial disability. Otol Neurotol. 2003;24(4):677-81.
17. Labbé D, Bénateau H, Bardot J. Les procédés chirurgicaux de réanimation labiale dans la paralysie faciale. Ann Chir Plast Esthet. 2002;47(5):580-91.
Full member of the Brazilian Society of Plastic Surgery, plastic surgeon of Rede SARAH de Hospitais de Reabilitação, Brasília, DF, Brazil.
Correspondence to:
Kátia Torres Batista
SMHS - Quadra 301 - Bloco A
Brasília, DF, Brazil - CEP 70335-901
E-mail: katiatb@terra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: June 2, 2011
Paper accepted: October 11, 2011
Study conducted at Rede SARAH de Hospitais de Reabilitação, Brasília, DF, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter