

Original Article - Year 2011 - Volume 26 -
Mandible fracture: epidemiological study of 70 cases
Fratura de mandíbula: estudo epidemiológico de 70 casos
ABSTRACT
BACKGROUND: Mandible fractures are most often caused by direct trauma, but occasionally, pathologic fractures may occur due to tumor lesions. The surgical approach is determined by the type and the location of the mandible fracture. This study aimed to evaluate the epidemiological profile of 70 patients who suffered mandible fracture and underwent surgery at Instituto Dr. José Frota (Fortaleza, CE) between January 2005 and December 2009.
METHODS: We analyzed medical records of 70 patients who underwent surgical treatment for mandibular fractures and assessed gender, age, skin color, anatomic site of fracture, etiology, associated fractures, treatment, hospitalization and complications.
RESULTS: There was male predominance (90%) among patients, with a mean patient age of 28.25 + 11.04 years. Most patients (80%) were Caucasian and from small towns (68%). The most affected jaw sites, in descending order, were the parasymphysis region, body, and angle. The major cause was traffic accidents (70%), with motorcycle accidents being the most prevalent (55.7%). The main associated facial fractures were maxilla fracture type Le Fort and zygomatic-orbital. Surgical treatment was carried out with rigid internal fixation in most patients (75%). The only complication was infection in one patient.
CONCLUSIONS: Reduction and fixation of mandibular fractures should occur as accurately and quickly as possible, since malocclusion is an important long-term complication. In our study, we did not observe such a complication; there was only one case of infection. Concurrent with the findings of other studies, there was a prevalence of young adult males among patients, and traffic accidents were the main cause. The fractures were frequently located in the parasymphysis region and were corrected through rigid internal fixation in 75% of cases.
Keywords: Mandible/surgery. Mandibular injuries. Mandibular fractures. Facial injuries.
RESUMO
INTRODUÇÃO: As fraturas de mandíbula são frequentemente causadas por traumatismo direto, mas, eventualmente, podem surgir fraturas patológicas, em função de lesões tumorais. A abordagem cirúrgica é determinada pelo tipo e pela localização da fratura na mandíbula. O objetivo deste estudo foi avaliar o perfil epidemiológico de 70 pacientes que sofreram fratura de mandíbula e foram operados no Instituto Dr. José Frota (Fortaleza, CE) no período de janeiro de 2005 a dezembro de 2009.
MÉTODO: Foram analisados prontuários de 70 pacientes submetidos a cirurgia para correção de fratura de mandíbula, avaliando-se sexo, idade, cor, procedência, sítio anatômico da fratura, etiologia, fraturas associadas, tratamento, tempo de internação e complicações.
RESULTADOS: Houve predomínio do sexo masculino (90%), com média de idade de 28,25 + 11,04 anos. A maioria dos pacientes (80%) era de cor branca e procedente do interior (68%). Os locais da mandíbula mais acometidos foram a região da parassínfise, o corpo e o ângulo, tendo como principal causa os acidentes de trânsito (70%), sendo os acidentes motociclísticos (55,7%) mais prevalentes. As principais fraturas de face associadas foram de maxila do tipo Le Fort e zigomático-orbitário. O tratamento cirúrgico foi feito com fixação interna rígida na maioria dos pacientes (75%). A única complicação foi infecção, observada em um paciente.
CONCLUSÕES: A redução e a fixação das fraturas mandibulares devem ocorrer tão precisa e rapidamente quanto possível, visto que a maloclusão é uma complicação grave a longo prazo. Neste estudo, essa complicação não foi observada, havendo apenas um caso de infecção. Coincidindo com os achados de outros estudos, houve prevalência de adultos jovens do sexo masculino e de acidentes de trânsito como etiologia. As fraturas foram localizadas preferencialmente na região da parassínfise e corrigidas por meio de fixação interna rígida em 75% dos casos.
Palavras-chave: Mandíbula/cirurgia. Traumatismos mandibulares. Fraturas mandibulares. Traumatismos faciais.
Maxillofacial injuries are very common and may have a significant functional impact1. Initially, most of these injuries are not life threatening, so assessment and definitive care are frequently postponed in patients with multiple lesions2.
Facial fractures may lead to significant hemorrhage of the maxillary or palatine arteries, which are branches of the external carotid artery. The internal carotid artery may also be injured in cases of fracture in the cranial base1.
The focus of this study is the mandibular bone, the largest among the facial bones and the only one that has mobility (temporomandibular articulation) 3. This bone is vital for functions such as chewing, swallowing, maintenance of dental occlusion, and phonation3-5.
A mandibular injury normally involves two fractures; therefore, whenever a fracture is identified, it is necessary to investigate whether another exists3.
Mandible fractures are often caused by direct trauma, but occasionally pathologic fractures may occur due to tumor lesions6. The need for surgical intervention and its nature are determined by the type and location of the fracture in the mandible1. The common lines of fracture are symphysis, parasymphysis, angle, branch, condyle, intracapsular, and coronoid. The prevalence of fracture at each location varies in previously published studies1.
In most cases, simple fractures result from low-impact trauma, such as fall from height or physical aggression6. Compound fractures are usually caused by high-impact trauma, which is more frequent in car accidents6. In almost all cases, comminuted fractures are caused by firearm bullets6. Most studies indicate car accidents as the major cause for such trauma2,4,5,7-10.
Imaging techniques frequently used to identify and classify this type of fracture include radiography, panoramic tomography, and helical computed tomography (CT) scan1. The most indicative specific sign of mandibular fracture is the "disarticulated interdental" or dental occlusion. Another sign in almost all cases is mandibular trismus6.
This study aimed to evaluate the epidemiological profile of patients who suffered mandible fracture and underwent surgery at Instituto Dr. José Frota (Fortaleza, CE, Brazil) between 2005 and 2009. We also sought to analyze the major causes, most affected regions of the mandible, surgical procedures chosen for each case, existence of associated trauma and preexisting diseases, post-surgical complications, and prognosis.
METHODS
An epidemiological, observational, descriptive, and retrospective study was conducted by analyzing medical records of 70 patients treated at Institute Dr. José Frota between 2005 and 2009.
The collected data were used to assess the following information: gender, age, ethnicity, city origin, anatomical site and cause of the fracture, associated trauma, preexisting diseases, surgical treatments and drugs used, admission period, and complications.
The data were analyzed with Epi-Info 6.04 and Microsoft Excel 2007 software and were presented in absolute and percentage values.
The present study was approved by the Ethics Committee of the institution.
RESULTS
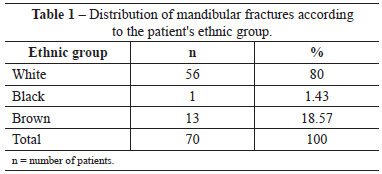
Analyses of the medical records of 70 patients diagnosed with mandibular trauma showed that 90% were men and only 10% were women. Males therefore outnumbered females 9 to 1. With regard to the ethnicity of patients, the most prevalent group was Caucasian (80%) (Table 1).
The patients were divided into 4 groups, according to age: <18 years old (10%), 18 to 25 years old (40%), 26 to 35 years old (24.29%), and >35 years old (25.71%). The mean age was 28.25 + 11.04 years.
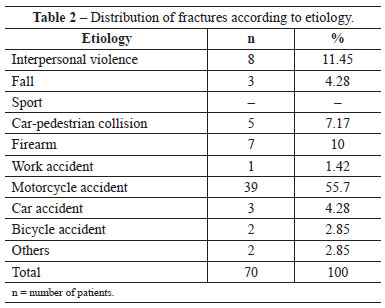
In 55.7% of patients, the major cause of fracture was motorcycle accident, followed by interpersonal violence (11.45%), and car-pedestrian accidents (7.17%) (Table 2).
Most of the analyzed patients (68.57%) were from the countryside, and some (31.43%) were from Fortaleza (the State capital).
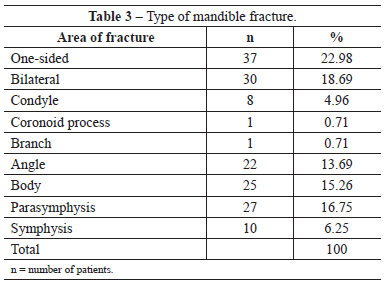
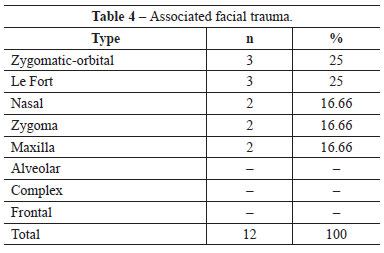
The most affected regions of the mandible were (in descending order) the parasymphysis, body, and angle (Table 3). In the presence of associated facial trauma, fractures of the zygomatic-orbital type and of the maxilla (Le Fort) were the major types, both affecting three patients. Nasal, zygomatic, and other maxilla fractures affected two patients (Table 4).
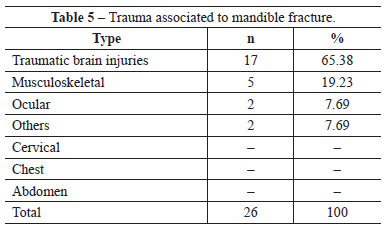
With regard to associated injuries, traumatic brain injuries affected 65.38% of the patients, while injuries involving the skeletal muscle and ocular areas comprised 19.23% and 7.69% of all associated injuries, respectively (Table 5).
There was no history of preexisting diseases in the analyzed records.
Surgical treatment with rigid internal fixation was the most commonly used intervention (75.72%), followed by rigid internal fixation plus maxillomandibular block (24.28%). The patients were medicated with antibiotics, non-steroid anti-inflammatory drugs, and corticosteroids. Only one patient had infection as a post-surgical complication.
DISCUSSION
Facial trauma constitutes frequent lesions that may be severe due to association with functional and psychological problems6.
After studying 1,326 facial fractures in 911 patients, Chrcanovic et al.11 reported that the most commonly fractured facial bone was the mandible, followed by the zygomatic complex and nose.
Martins Junior et al.12 carried out a study involving 222 patients with maxillofacial fractures and observed a greater prevalence of mandible fracture (35.87%), followed by nose (22.9%) and zygoma (20.99%) fracture.
The site where the mandibular fracture occurs is variable, depending on the cause of trauma. Therefore, reports in the literature are quite divergent with regard to the most affected sites4. In the present study, the parasymphysis and the body were the regions with the greatest incidence of fractures.
Accidents with automotive vehicles are highlighted worldwide as the main and most aggressive agents of facial trauma. Head trauma accounts for more than 70% of trauma cases8 resulting from car accidents.
The present study evidenced many more male patients than females, and this fact may be attributed to several factors. Men are more frequently involved in traffic, mainly on roads; they also participate in more physical contact sports, go to bars as a social activity, and consequently, misuse drugs such as alcohol before driving9. With regard to different causes of mandible fracture, 39 (55.7%) patients in the study were injured as a result of a motorcycling accident.
The most affected age group was the 18- to 25-year-old group. The literature indicates that the 21- to 30-year-old age group is the most affected by facial trauma, as young individuals are more likely to get involved in urban violence and psychosocial economic conflicts8.
The major surgical treatment employed in this study was rigid internal fixation with mini-plates and screws. This is the most efficient method for the reduction of mandible fracture and enables the best containment of fragments, in addition to long-term stabilization and decrease of bone repair time10. Moreover, the use of biocompatible material that has excellent physical and mechanical properties promotes greater stability of fractures. Its use is indicated in a bicortical manner in fractures with bone defect and comminution and lateral injury of the bone10.
REFERENCES
1. Hoyt DB, Coimbra R, Acosta J. Atendimento inicial ao traumatizado. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston: tratado de cirurgia. 18ª ed. Rio de Janeiro: Elsevier; 2010. p. 462.
2. Goto AAA, Aguiar AS, Denardin OVP, Rapport A. Tratamento cirúrgico das fraturas subcondilares: avaliação da abordagem retromandibular de Hinds. Rev Col Bras Cir. 2007;34(5):303-8.
3. Moore KL, Dalley AF. Cabeça. In: Anatomia orientada para a clínica. 4ª ed. Rio de Janeiro: Guanabara Koogan; 2001. p. 747-8.
4. Horibe EK, Pereira MD, Ferreira LM, Andrade Filho EF, Nogueira A. Perfil epidemiológico de fraturas mandibulares tratadas na Universidade Federal de São Paulo - Escola Paulista de Medicina. Rev Assoc Med Bras. 2004;50(4):417-21.
5. Patrocínio LG, Patrocínio JA, Borba BHC, Bonatti BS, Pinto LF, Vieira JV, et al. Fratura de mandíbula: análise de 293 pacientes tratados no Hospital de Clínicas da Universidade Federal de Uberlândia. Rev Bras Otorrinolaringol. 2005;71(5):560-5.
6. Freire E. Fraturas da face. In: Gardelmann I, Boghossian LC, Medeiros PJ, eds. Trauma: a doença dos séculos. São Paulo: Atheneu; 2001. p. 1297-9.
7. Andrade Filho EF, Fadul Junior R, Azevedo RA, Rocha MA, Santos R, Toledo SR, et al. Fraturas de mandíbula: análise de 166 casos. Rev Assoc Med Bras. 2000;46(3):272-6.
8. Silva JJL, Lima AAAS, Torres SM. Fraturas de face: análise de 105 casos. Rev Bras Cir Craniomaxilofac. 2009;12(1):16-20.
9. Rodrigues FHOC, Miranda ES, Souza VEM, Castro VM, Oliveira DRF, Leão CEG. Avaliação do trauma bucomaxilofacial no Hospital Maria Amélia Lins da Fundação Hospitalar do Estado de Minas Gerais. Rev Soc Bras Cir Plást. 2006;21(4):211-6.
10. Silva J, Cauás M. Fratura de mandíbula decorrente de acidente automobilístico: relato de caso. Odontol Clín Cient. 2004;3(3):199-207.
11. Chrcanovic BR, Freire-Maia B, Souza LN, Araújo VO, Abreu MH. Facial fractures: a 1-year retrospective study in a hospital in Belo Horizonte. Braz Oral Res. 2004;18(4):322-8.
12. Martins Junior JC, Keim FS, Helena ETS. Aspectos epidemiológicos dos pacientes com traumas maxilofaciais operados no Hospital Geral de Blumenau, SC, de 2004 a 2009. Arq Int Otorrinolaringol. 2010;14(2):192-8.
1. Master in Surgery, plastic surgeon, full member of the Brazilian Society of Plastic Surgery (SBCP), Fortaleza, CE, Brazil.
2. Physiotherapist of Instituto Dr. José Frota, Fortaleza, CE, Brazil.
3. Medicine Student, Fortaleza, CE, Brazil.
Correspondence to: Joaquim José de Lima Silva
Rua Barão do Rio Branco, 1.816 - Centro
Fortaleza, CE, Brazil - CEP 60025-061
E-mail: cirurgiaoplastico@joaquimjose.med.br
Submitted to SGP (Sistema de Gestão de Publicações/ Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica / Brazilian Journal of Plastic Surgery).
Paper received: April 2, 2011
Paper accepted: October 16, 2011
Study conducted at Instituto Dr. José Frota, Fortaleza, CE, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter