

Original Article - Year 2011 - Volume 26 -
Use of latissimus dorsi muscle segment with muscle and fat components in single decubitus position for breast reconstruction after quadrantectomy
Uso do retalho miogorduroso segmentar do músculo latíssimo do dorso em decúbito único para reconstrução da mama pós-quadrantectomia externa
ABSTRACT
BACKGROUND: Nowadays, more and more immediate breast reconstructions are carried out after cancer treatment. For performing radical mastectomy, there are several recognized techniques. In quadrantectomy, the options for defect repair range from primary closure to the use of oncoplastic surgery techniques. In the case of external quadrant tumors, there is no option of rotation of the entire latissimus dorsi muscle, which usually exceeds the actions necessary for repairing lost volume. A new option for post-quadrantectomy reconstruction in external quadrants is proposed in this study.
METHODS: The surgical technique consists of dissection of the lateral segment of the latissimus dorsi muscle by an extension of the incision for lesion removal in the same supine position, followed by rotation and modeling of this segment to repair the defect caused by cancer removal. Twenty-one women aged 33 to 69 years underwent quadrantectomies of external quadrants followed by reconstruction with the technique described in this paper. To evaluate the method, each result had a score attributed to volume, shape, symmetry, and changes in the nipple areolar complex, as well as scar and operated quadrant surface.
RESULTS: The obtained results of volume and shape were superior in relation to those of symmetry. The average grade was 7.048, equivalent to B concept.
CONCLUSIONS: The new technique decreased surgical time. The acquisition of the B concept demonstrates the method's feasibility.
Keywords: Breast neoplasms/surgery. Mammaplasty. Plastic surgery/methods.
RESUMO
INTRODUÇÃO: Cada vez mais são realizadas reconstruções imediatas da mama pós-tratamento do câncer. Para as mastectomias radicais, há várias técnicas consagradas. Na quadrantectomia, as opções de reparação do defeito vão do fechamento primário à utilização de técnicas de cirurgia oncoplástica. Para os tumores dos quadrantes externos, a opção de rotação de todo o músculo latíssimo do dorso é desnecessária, uma vez que usualmente excede ao necessário à reparação do volume perdido. Neste trabalho é proposta uma nova opção para a reconstrução pós-quadrantectomia em quadrantes externos.
MÉTODO: A técnica cirúrgica consiste na dissecção do segmento lateral do músculo latíssimo do dorso pelo prolongamento da incisão para a retirada da lesão, no mesmo decúbito dorsal, seguida de sua rotação e modelagem para reparar o defeito decorrente da extirpação do câncer. No total, 21 mulheres com idade entre 33 anos e 69 anos foram submetidas a quadrantectomias de quadrantes externos, seguidas da reconstrução com a técnica descrita neste trabalho. Para a avaliação do método, cada resultado teve atribuído um escore a volume, forma, simetria e alterações do complexo areolopapilar, da cicatriz e da superfície do quadrante operado.
RESULTADOS: Os resultados obtidos na avaliação do volume e da forma foram superiores em relação aos da simetria. A nota média foi 7,048, equivalente ao conceito B.
CONCLUSÕES: A nova técnica propiciou diminuição do tempo cirúrgico. A aquisição do conceito B demonstra a viabilidade do método.
Palavras-chave: Neoplasias da mama/cirurgia. Mamoplastia. Cirurgia plástica/métodos.
Globally, breast cancer is the most frequent malignant tumor among women and the leading cause of cancer death in women1. In Brazil, breast cancer is one of the leading causes of death, second only to cardiovascular diseases2. Based on the major types of breast neoplasia, almost all patients who have breast cancer have to undergo a surgical procedure as part of treatment3.
Until the end of the 20th century, breast cancer was considered incurable. William Steward Halsted (1852-1922), in Baltimore (Maryland, United States), gave rise to a new age in breast cancer treatment by introducing concepts that included the removal of cancerous tissues en bloc, avoiding contamination of the wound with tumoral cells. From the time his study was presented in 1894, Halsted's technique dominated the surgical horizon of breast cancer. Indeed, this technique was the standard surgical treatment for this type of neoplasia4 for more than 70 years.
Recently, several researchers have demonstrated that more conservative surgical procedures that achieve satisfactory and long-lasting results can be performed, suggesting alternatives to aggressive techniques. There are no differences in survival when well-indicated use of each type of procedure is compared5.
In the current view of breast cancer treatment, the concept of oncoplastic (OP) surgery is highlighted. This therapeutic option includes 3 essential points: ideal oncological surgery, homolateral reconstruction, and immediate contralateral remodeling by employing plastic surgery techniques6.
The first attempts to perform breast reconstruction date back to the end of the 19th century, when Verneuil used part of a normal breast to reconstruct the other in 18877. The first autogenous breast reconstructions were performed in the late 1970s by Brantigan, who used transposition of the latissimus dorsi muscle7. Since the end of the 20th century, other regions are used for obtaining free distant myocutaneous flaps, such as the superior gluteal artery perforator (SGAP)8.
In cases of enlarged mastectomy because of advanced cancer, thoracic wall reconstruction is performed using myocutaneous flaps of the latissimus dorsi muscle; this procedure gave rise to the idea of using the flap of the latissimus dorsi with its pedicle to fill the excision zones of breast quadrants in cases of external quadrant resection of small breasts.
The purpose of this study was to demonstrate the benefits of dissection and transposition of the lateral segment of the latissimus dorsi muscle - at the same decubitus in which the tumor is removed and in the same position (supine) - by placing it over the deep lamellar layer of the subcutaneous cellular tissue. This technique provides the necessary muscular volume for remodeling the operated breast. Post-quadrantectomy breast reconstruction becomes considerably easier, thus ensuring greater safety, less surgical trauma, and lower possibility of surgical field contamination.
METHODS
This is a descriptive study containing observational analysis of surgical results. The research project, previously submitted for review to the Ethics and Research Committee of Maternidade Escola Assis Chateaubriand of Universidade Federal do Ceará (CEP/MEAC/UFC), was approved (Protocol No 82/07) and developed according to the principles established by the National Commission of Ethics in Research (CONEP).
Twenty-one adult patients aged between 33 and 69 years were included in the study. Patients were treated for breast cancer over a period of 11 months in the Mastology Service of MEAC/UFC, after signing the Terms of Free and Clarified Consent.
Lee et al.9,10 reported a test to assess the health of patient latissimus dorsi muscles. The following patients were excluded: those not fulfilling the criteria of the muscular health test, those with malignant lesions greater than 3 cm in diameter and/or impairing more than 1 breast quadrant, and those with comorbidities that contraindicated major surgical procedures.
The surgical technique consisted of dissecting and rotating the lateral myoadipose segment and the latissimus dorsum muscle, in order to compose the shape and volume of the lost breast tissue in the oncological procedure. The procedure was performed with the patient in the same decubitus position and using the same incision through which the lesion was resected. The patient was in the established decubitus, with the side to be operated elevated by approximately 30 degrees, constituting a modified supine position (Figures 1 and 2).
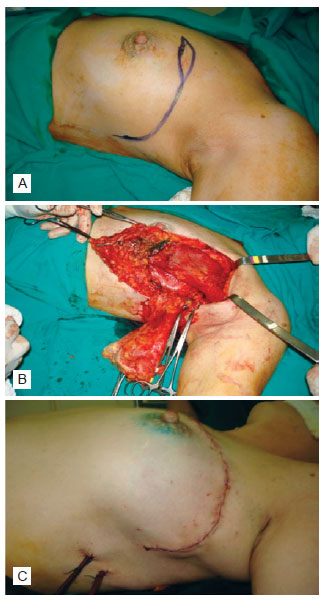
Figure 1 - In A, cutaneous incision demarcation to remove the lesion in junction of upper quadrants, with prolongation in the craniocaudal direction for access to the latissimus dorsi. In B, surgical wound aspect, after resection of the specimen and flap dissection. In C, lateral aspect of the closed surgical wound.
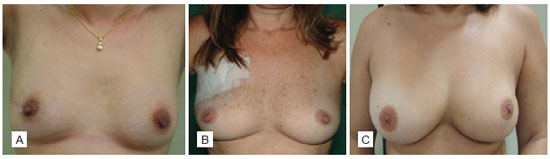
Figure 2 - In A, example of small breast reconstruction. In B, example of medium-sized breast reconstruction. In C, example of large breast reconstruction.
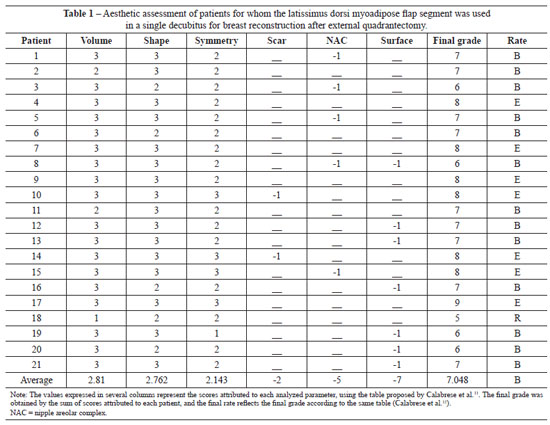
The assessment method was adapted from the model proposed by Calabrese et al.11 and also employed by Urban12. Result assessment was based on the perception of a plastic surgeon or mastologist evaluator, with reference to 3 parameters (volume, shape, and symmetry). The comparative basis was the non-operated breast, and grades from 1 to 3 were allocated by postoperative evaluation of parameters. This score was decreased by 1 point every time the following elements were identified: apparent and poor quality scar, malpositioned nipple areolar complex, and irregularity of the reconstructed quadrant surface (Figure 3). Summed scores of between 8 and 9 were considered excellent (operated breast with little noticeable differences); between 6 and 7, good (operated breast with differences in dimensions, yet aesthetically acceptable); between 4 and 5, regular (noticeably different breasts, and the operated breast significantly misshapen); and 3 or less, unsatisfactory.
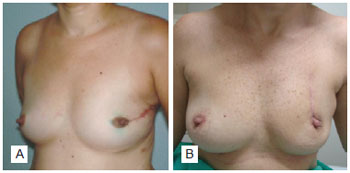
Figure 3 - In A, healing disorders and lateral deviation of the nipple areolar complex. In B, surface disorders of the operated quadrant.
RESULTS
The values obtained in the aesthetic assessment are listed in Table 1.
The results of volume and shape evaluations were better than those of symmetry evaluation (Figure 4).
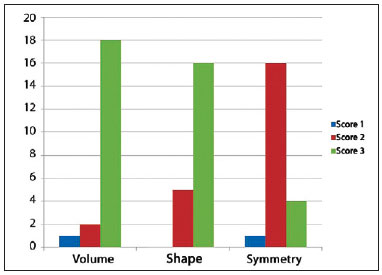
Figure 4 - Representation of the absolute frequency distribution of surgical results, according to the variables of volume, shape, and symmetry.
There was suitable healing in 19 patients. We observed surface alterations of the reconstructed quadrant in 7 patients and alterations in the nipple areolar complex in 5 patients.
Most of the results obtained with the procedures performed were assessed as excellent (33.33%) or good (57.14%). In only 2 (9.52%) cases, the results classified as regular. With regard to postoperative complications, 2 patients had hematomas and 4 had seromas.
DISCUSSION
The results obtained in 21 operated patients who underwent breast reconstruction using the latissimus dorsi myoadipose flap reveal the promising applicability of this technique. Variability in volume, shape, and symmetry was assessed in this study, taking into account alterations in healing, nipple areolar complex position, and appearance and deformity of the operated quadrant.
The data support the concept that the technique is feasible in a single decubitus position. One of the most relevant aspects of this technique is the ease of dissecting the latissimus dorsi muscle with the patient in a modified supine position, the same surgical position in which quadrantectomy is performed. This technique therefore decreases surgical time and lowers risk of accidental extubation and infection of surgical sites.
To determine the quality of the final outcome, the operated breast was assessed using the other breast as a comparison parameter. By assessing only the replacement of lost breast volume in the external quadrantectomy, the result analysis proves that the technique proposed herein is feasible and advantageous. Average scores for the postoperative volume were equivalent to 94% of the total possible score. For result assessment with regard to volume, each breast received a score of 1 to 3, as described above. Of 21 patients, 18 received grades 3; 2 patients received grade 2; and 1 patient received grade 1. On average, the grade assigned to the volume was 2.8. The data collected for breast shape and symmetry after surgery also provided evidence of the feasibility and advantage of the technique described. Average scores for breast shape in each case were equivalent to 92% of the maximum possible grade. In 16 patients, the score for shape was 3, the maximum possible. In the other 5 cases, shape scores were 2. Thus, even with a small number of patients, the aesthetic benefits of this technique were apparent. With regard to symmetry, the following results were achieved: 1 patient received grade 1; 16 patients received grade 2; and 4 patients received the maximum grade of 3. Average scores for all cases was equivalent to 71.43% of the maximum possible value.
It is important to consider that symmetry is a variable that suffers more directly from interference of the healing process. Surface irregularity of the operated quadrant and position of the nipple areolar complex, which depend on the excision stage of the oncological specimen, may in turn affect the assessment of symmetry.
Average scores for volume and shape were greater than those for symmetry. Considering overall results in the group, the proposed technique had better results in the aspects of volume (average score: 2.81, corresponding to 93.66% of the maximum grade) and shape (average score: 2.76, corresponding to 92.06% of the maximum grade). Symmetry achieved an average of 2.14, equivalent to 71.33% of the maximum grade.
In only 2 cases, the scar was apparent and of poor quality. None of the factors that influenced the healing result is exclusively a result of the reconstructive surgery. Moreover, even scars of aesthetic surgeries may show visible change, and that the procedures for handling of the tissues during surgery remains the same, regardless of the type of operation performed.
Considering nipple areolar complex positioning, alterations occurred in only 5 cases. The nipple areolar complex, let alone the entire breast, may not be symmetric with the contralateral breast, even in non-operated women and in those who have never had breast disease. Considering that this asymmetry is regularly found in all women, it is acceptable that the nipple areolar complex is located distant from its usual positioning, particularly in cases of removal of an entire breast quadrant and quadrant reconstruction.
The presence of surface irregularities in the reconstructed quadrant may occur due to resection of a greater amount of adipose tissue to increase the safety margin of the tumor. To avoid this effect, the adipose tissue of the lamellar layer was used, which remains overlying the muscle. Irregularities in the reconstructed quadrant surface, characterized by bulging or retraction, were observed in 7 cases. In general, irregularities were located at area of quadrant contouring, probably due to the superficiality of the resection, which is generally the only option for the mastologist.
In a joint analysis, excellent results were observed in 33.33% of patients and good results in 57.94% of patients. The absence of unsatisfactory results demonstrates the quality of the procedure. Complications related to the plastic surgery were reduced.
No studies have reported the reconstruction described herein; this is another determining factor for the relevance of the applied technique.
CONCLUSIONS
The use of the latissimus dorsi myoadipose flap segment in a single decubitus position is beneficial and feasible for volume and shape replacement of breast substance lost secondary to quadrantectomy of the external quadrant of the breast for treatment of breast cancer.
With respect to the effectiveness of the technique proposed in this study, it is possible to infer that this technique will provide good aesthetic results.
REFERENCES
1. Ferlay J, Bray F, Pisani P, Parkin DM. Cancer incidence, mortality and prevalence worldwide. Lyon: IARC Press; 2004.
2. Instituto Nacional do Câncer. Câncer de mama. Rev Bras Cancerol. 2001;47(1):9-19.
3. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233-41.
4. Hasteld WS. The results of operations for the cure of cancer of the breast performed at the Johns Hopkins Hospital from June, 1889, to January, 1894. Ann Surg. 1894;20(5):497-555.
5. Escudero FJ. Evolución histórica de la reconstrucción mamaria. An Sist Sanit Navar. 2005;28(Suppl. 2):7-18.
6. Baildam AD. Oncoplastic surgery of the breast. Br J Surg. 2002;89(5):532-3.
7. Uroskie TW, Colen LB. History of breast reconstruction. Semin Plast Surg. 2004;18(2):65-9.
8. Bostwick J 3rd, Jones G. Why I choose autogenous tissue in breast reconstruction. Clin Plast Surg. 1994;21(2):165-75.
9. Hochberg J. Manual de retalhos miocutâneos. Porto Alegre: AMIRGS; 1984.
10. McCraw JB, Papp CTH. Latissimus dorsi myocutaneous flap. In: Hartrampf CR, ed. Breast reconstruction with living tissue. Norfolk: Hampton Press; 1991. p. 211-48.
11. Calabrese C, Distante V, Orzalesi L. Immediate reconstruction with mammaplasty in conservative breast cancer treatment: long-term cosmetic results. Osp Ital Chir. 2001;7(1/2):38-46.
12. Urban CA. Resultados da oncoplástica no tratamento conservador em câncer de mama [tese de doutorado]. Curitiba: Setor de Ciências da Saúde, Universidade Federal do Paraná; 2004. 204 p.
1. Master in Tocogynecology by the School of Medicine of Universidade Federal do Ceará (UFC), full member of the Brazilian Society of Plastic Surgery (SBCP), Fortaleza, CE, Brazil.
2. Doctor of surgery, School of Medicine of Universidade Federal de Pernambuco, associate professor of the Department of Surgery of the School of Medicine of UFC, Fortaleza, CE, Brazil.
3. Plastic Surgeon, specialist member of SBCP, Fortaleza, CE, Brazil.
4. Undergraduate student of medicine in the School of Medicine of UFC, scientific initiation scholarship student at the Experimental Surgery Laboratory Dr. Saul Goldenberg of UFC, Fortaleza, CE, Brazil.
5. Undergraduate student of medicine in the School of Medicine of UFC, member of the Studies Group and Education in Oncology of the School of Medicine of UFC, Fortaleza, CE, Brazil.
6. Undergraduate student of medicine in Universidade de Fortaleza (UNIFOR), Fortaleza, CE, Brazil.
Correspondence to:
João Batista Fortaleza de Araújo
Rua Paula Ney, 827 - ap. 702 - Aldeota
Fortaleza, CE, Brazil - CEP 60140-200
E-mail: jbfortaleza@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: July 3, 2011
Paper accepted: October 2, 2011
Study conducted at the Mastology Department of Maternidade Escola Assis Chateaubriand (MEAC), School of Medicine of Universidade Federal do Ceará (UFC), Fortaleza, CE, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter