

Case Report - Year 2012 - Volume 27 -
Use of a composite auricular graft in nasal alar reconstruction
Enxerto composto auricular na reconstrução da asa nasal
ABSTRACT
Since the nose is located in the center of the face, small asymmetries and imperfections are easily recognized. One subunit of the nose is the nasal ala, a region that, when reconstructed, requires the achievement of esthetic and functional results. This poses a challenge to the plastic surgeon. In this article, we describe 3 cases of composite auricular grafts used for nasal alar reconstruction. The grafts presented total integration and provided satisfactory esthetic and functional results. A literature review revealed no differences in the complication rates between grafts and local flaps. Moreover, the shape of the auricular cartilage was maintained over time, showing rare distortions and no or minimal absorption, contrary to costal cartilage and bone grafts. The use of composite auricular grafts is versatile and safe. This procedure ensures excellent results in nasal alar reconstruction and guarantees low morbidity within the donor areas. Therefore, the use of this technique efficiently enables the repair of nasal defects.
Keywords: Nose/surgery. Reconstructive surgical procedures. Ear, external/transplantation.
RESUMO
O nariz ocupa o centro da face, o que torna pequenas assimetrias e imperfeições evidentes. Uma de suas subunidades é a asa nasal, região que exige não apenas resultados estéticos, mas também funcionais, em sua reconstrução, tornando-se um desafio ao cirurgião plástico. Neste artigo são descritos 3 casos em que foi utilizado enxerto composto auricular para reconstrução da asa nasal. Os enxertos apresentaram integração total, com resultados estéticos e funcionais adequados. Segundo revisão da literatura, não há diferença nos índices de complicação comparando-se os enxertos com os retalhos locais e, a longo prazo, a cartilagem auricular tende a manter-se no formato moldado, sofrendo raras distorções e mínima ou nenhuma absorção, diferentemente das cartilagens costais e dos enxertos ósseos. O enxerto composto auricular é uma técnica versátil e segura, com excelentes resultados na reconstrução da asa nasal e com baixa morbidade das áreas doadoras, cumprindo com eficiência seu objetivo reparador.
Palavras-chave: Nariz/cirurgia. Procedimentos cirúrgicos reconstrutivos. Orelha externa/transplante.
The nose is located in the center of the face, and therefore, the presence of small asymmetries and imperfections are easily recognized. One of the subunits of the nose is the nasal ala, a region that, when reconstructed, requires the achievement of esthetic and functional results. Thus, nasal alar reconstruction poses challenges for plastic surgeons.
The 4 layers that compose the nasal alar unit include the nasal lining, dense connective tissue, cartilage, and skin. The complex contour of the nose and the free margin that contributes to the external nasal valve enable the use of several procedures for nasal reconstruction including local nasal flaps, skin grafts, composite auricular grafts, and pedicle flaps, among others1-4.
The first case of the use of a composite auricular graft for nasal alar reconstruction was reported by Koenig in 1902 4. In 1943, Gillies described the use of forehead flaps combined with composite skin and an auricular cartilage graft, whereas in 1946, Bronx demonstrated their specific use for nasal alar areas4.
In this article, we describe 3 patients presenting with nasal alar post-traumatic sequelae, 2 of which were caused by human bites, and their surgical reconstruction using composite skin and auricular cartilage grafts. The lack of scientific articles regarding the avulsion of nasal tissue and its etiology encouraged us to perform this study.
CASES REPORT
Case 1
A 39-year-old female patient experienced burns on 45% of her body surface area, including her face, while trying to commit suicide. She experienced partial right nasal alar loss among other sequelae (Figure 1A).

Figure 1 - Case 1. In A, preoperative appearance of a post-burn sequela. In B, composite skin and auricular cartilage graft. In C, intraoperative appearance. In D, appearance at 30 days after surgery. In E, appearance at 6 months after surgery.
In the following months, the patient underwent 9 reconstructive procedures. Fourteen months later, a right nasal alar reconstruction was performed using a composite graft from the antihelix of the right ear (dorsal skin and cartilage) (Figures 1B and 1C). Although viable, the graft was purple-red during the first week. It then integrated completely and the surgical wound presented a satisfactory appearance (Figure 1D).
Six months after the surgery, the patient was satisfied with the result obtained (Figure 1E).
Case 2
A 23-year-old female patient was the victim of physical aggression consisting of a human bite. She presented with right nasal alar deformities, a 1 cm × 0.5 cm nasal alar defect and some alar cartilage imperfections (Figures 2A and 2B). The patient was a smoker.
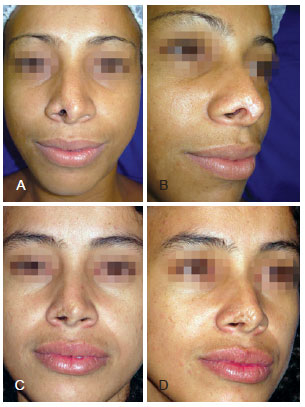
Figure 2 - Case 2. In A and B, preoperative appearance of nasal alar sequelae caused by a human bite. In C and D, appearance at 1 year and 4 months after surgery showing maintenance of the esthetic result.
Five months later, the patient underwent nasal alar reconstruction using a composite graft (skin and cartilage) from the helix of the left ear, without complications. One year and 4 months after surgery, the patient was satisfied with the esthetic results (Figures 2C and 2D).
Case 3
A 50-year-old female patient was the victim of physical aggression consisting of a human bite that had occurred 19 years prior. The deformity she presented with on the right nasal alar regions was reconstructed by another division before she requested the expertise of our team. She complained about her nasal esthetic appearance due to a scar and abnormal contour of the right ala of the nose (Figure 3A). The patient also presented with scar retraction of the right ear, which had served as the donor area for the first graft (Figure 3D). The patient was a smoker.
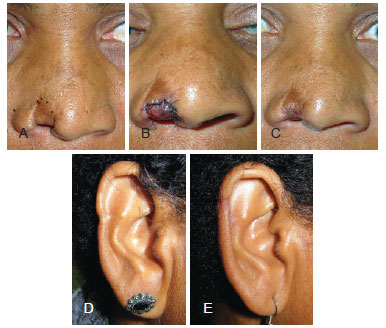
Figure 3 - Case 3. In A, preoperative appearance of nasal alar sequelae caused by a human bite. In B, recent postoperative appearance (sixth postoperative day) showing a purple-red composite graft. In C, appearance at 1 year after surgery. In D, ear sequelae caused by a previous surgery. In E, postoperative appearance upon new composite graft donation of the indicated region and repair of the defect using a skin helix advancement flap.
In 2006, the patient underwent right nasal alar reconstruction using a composite graft (skin and cartilage) from the helix of the right ear. An advancement skin flap was created from the helix of the right ear to correct auricular deformities. The graft was purple-red until almost 6 days after surgery (Figure 3B). After that point, the surgical wound presented a satisfactory appearance, although moderate final hyperchromia of the graft was observed 1 year after the surgery (Figure 3C).
The patient was satisfied with the final result in the nasal alar region and with the auricular contour (Figure 3E).
DISCUSSION
According to the concepts of nasal reconstruction by contour subunits5, the presence of delicate cartilage and thin skin enables consideration of the ala of the nose as the first choice as a donor area for nasal alar reconstructions4. The most common regions used for this purpose are the anti-helix and the auricular upper pole6. These composite grafts should be used to repair 1 cm - 1.5 cm defects1 and provide more satisfactory esthetic results in defects of up to 0.8 cm5.
For major defects of the nasal ala (i.e., > 1.5 cm), local or free flaps may be used. However, microvascular flaps should be correctly designed to restore the size and volume of the lost tissue since, due to their retraction, a volume of 50% more than the defect to be covered should be considered when using this technique. The possibility of employing cartilage grafts to shape and reduce flap retraction should be considered7. To achieve more satisfactory esthetic results, the flap should then be carved.
According to Rustemeyer et al.8, no statistically significant difference was observed when the number of complications was compared between grafts (G) and local flaps (LF). The authors showed that the advantage of local flaps lies in a lower infection rate (LF 2.6% vs. G 5.4%) and a decreased percentage of partial or complete loss (LF 5.2% vs. G 8.5%). Concerning the aesthetic results, the grafts showed better results than local flaps, with percentage of unsatisfactory aesthetic results of 2.1% for G and 6.8 for LF8.
The ear and the nose are highly vascularized tissues; as such, they present a dense endothelial network. Compared to other features, this anatomic feature efficiently enables composite auricular graft imbibition supply toward the nasal region4 until the formation of a new capillary network. The pale appearance of the graft in the first few hours changes to a purple-red appearance, which indicates that erythrocyte invasion occurs between 6 and 24 hours after surgery. Then, due to graft congestion, it becomes cyanotic and, if it remains viable, turns pink after 3-7 days. In 1963, Reese et al. observed that 94% of composite grafts were viable when preserved at 5ºC-10ºC, a temperature that decreases their metabolism in the first 72 hours4. This procedure was used in case 1 described above.
Approximately 20% of composite grafts display central or superficial necrosis, which enables the construction of a new composite graft 3 months later5. Regarding long-term results, it is known that the shape of the auricular cartilage is maintained, showing rare distortions and no or minimal absorption, contrary to costal cartilage and bone grafts (which are less commonly used in rhinoplasties)9.
In the cases reported here, total integration of the composite grafts was observed, although they appeared cyanotic in the first few days after the surgery. The esthetic results were considered satisfactory by both the patients and the medical team.
Our literature review showed that the use of a composite auricular graft is versatile and safe. This procedure ensures excellent nasal alar reconstruction results and guarantees low morbidity in the donor areas10. Therefore, the use of this technique efficiently enables the repair of nasal defects as observed in the cases reported in this study.
REFERENCES
1. Heppt W, Gubisch W. Principles of nasal defect repair. HNO. 2007;55(6):497-510.
2. Thiêry G, Coulet O, Guyot L. Reconstruction of a transfixing partial loss of substance from the wing of nose with the upper pedicled nasolabial flap. Rev Laryngol Otol Rhinol (Bord). 2008;129(1):49-51.
3. Driscoll BP, Baker SR. Reconstruction of nasal alar defects. Arch Facial Plast Surg. 2001;3(2):91-9.
4. Barton Jr. FE, Byrd HS. Acquired deformities of the nose. In: McCarthy JG, ed. Plastic surgery. The face. vol. 3. Philadelphia: Saunders;1990. p.1924-2008.
5. Burget GC. Aesthetic reconstruction of the nose. In: Mathes SJ, ed. Plastic surgery. The head and neck. vol. 2. 2nd ed. Philadelphia: Elsevier; 2006. p.573-648.
6. Ishida LH, Ishida LC, Passos AP, Ishida J. Enxertos de músculo, fáscia tendão e enxertos compostos. In: Melega JM, Baroudi R, eds. Cirurgia plástica fundamentos e arte: princípios gerais. Rio de Janeiro: Medsi; 2002. p.99-106.
7. Burget GC, Walton RL. Optimal use of microvascular free flaps, cartilage grafts, and a paramedian forehead flap for aesthetic reconstruction of the nose and adjacent facial units. Plast Reconstr Surg. 2007;120(5):1171-207.
8. Rustemeyer J, Gunther L, Bremerich A. Complications after nasal skin repair with local flaps and full-thickness skin grafts and implications of patients' contentment. Oral Maxillofac Surg. 2009;13(1):15-9.
9. Bastos JAV. Rinoplastia a longo prazo. In: Melega JM, Baroudi R, eds. Cirurgia plástica fundamentos e arte: cirurgia estética. Rio de Janeiro: Medsi; 2002. p.389-94.
10. Haug MD, Rieger UM, Witt P, Gubisch W. Managing the ear as a donor site for composite graft in nasal reconstruction: update on technical refinements and donor site morbidity in 110 cases. Ann Plast Surg. 2009;63(2):171-5.
1. Plastic surgeon with residency training at Division of Plastic Surgery, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), associate member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), assistant professor of Faculdade de Medicina de Jundiaí (Faculty of Medicine of Jundiaí), Jundiaí, SP, Brazil.
2. Plastic surgeon with residency training at Division of Plastic Surgery, FMRP-USP, associate member of the SBCP, Ribeirão Preto, SP, Brazil.
3. Doctor, plastic surgeon, assistant physician at Division of Plastic Surgery of FMRP-USP, full member of the SBCP, regent of the Plastic Surgery Service of FMRP-USP, Ribeirão Preto, SP, Brazil.
4. Doctor, plastic surgeon, full member of the SBCP, chief at Division of Plastic Surgery of FMRP-USP, Ribeirão Preto, SP, Brazil.
Correspondence to:
Av. Bandeirantes, 3.900 - Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo - 9º andar - Monte Alegre
Ribeirão Preto, SP, Brasil - CEP 14049-9
E-mail: tiagoceratti@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: May 21, 2011
Article accepted: February 22, 2012
This study was performed at the Division of Plastic Surgery of the Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (Faculty of Medicine of Ribeirão Preto, University of São Paulo), Ribeirão Preto, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter