

Original Article - Year 2015 - Volume 30 -
Review of 150 cases of mandible fracture between 2010 and 2013 at the Cajuru University Hospital, Curitiba, PR
Revisão de 150 casos de fratura de mandíbula entre os anos de 2010 e 2013 no Hospital Universitário Cajuru - Curitiba, PR
ABSTRACT
INTRODUCTION: Mandible fractures are the second most frequent type of facial injury according to most studies. However, the epidemiological data on mandible fractures may vary between countries, or according to the trauma mechanism and the period of injury evaluation, owing to the influence of cultural, technological, environmental, and socioeconomic factors. This type of trauma comprises an important cost and morbidity factor. The aim of this study was to outline the epidemiological profile of mandible fractures treated at the Cajuru University Hospital from 2010 to 2013.
METHODS: A retrospective, descriptive, observational study was performed with 236 patients hospitalized in the Cajuru University Hospital, from January 2010 to July 2013, in whom mandible fracture was diagnosed. Only patients with complete records were included in the study, resulting in a total of 150 patients.
RESULTS: From the 150 records analyzed, it was found that mandible fractures were more prevalent in males, and the average age of patients was 29.9 years. Concerning the trauma-causing mechanisms, the most common were interpersonal violence (36.7%), traffic accidents (36.7%), and wounds caused by firearms (16%). Plate and screw fixation was the most frequently used treatment (111 patients).
CONCLUSIONS: Mandible fractures were mainly caused by interpersonal violence, and were more frequent in young males. Multiple fractures were present in almost half of the patients. In single fractures, the condyle and parasymphysis regions were the most affected. Open treatment was most commonly performed, with reconstruction with a titanium plate being the most common approach.
Keywords: Mandible; Maxillomandibular fracture; Face; Treatment.
RESUMO
INTRODUÇÃO: As fraturas mandibulares correspondem ao segundo tipo de lesões faciais mais frequentes na maioria dos estudos. Contudo, os dados epidemiológicos desta fratura podem variar conforme o país, o mecanismo de trauma e a época em que foram avaliadas, uma vez que são influenciadas por fatores culturais, tecnológicos, ambientais e socioeconômicos. Consistem em importante fator de custo e morbidade. Delinear o perfil epidemiológico dos casos de fratura de mandíbula tratados no Hospital Universitário Cajuru no período entre 2010 e 2013.
MÉTODO: Foi realizado um estudo retrospectivo, observacional e descritivo de 236 pacientes internados no Hospital Universitário Cajuru, no período de janeiro de 2010 a julho de 2013, diagnosticados com fratura de mandíbula. Foram incluídos no trabalho apenas os pacientes que apresentavam os prontuários contendo informações completas, totalizando 150 pacientes.
RESULTADOS: Dos 150 prontuários analisados, encontrou-se prevalência das fraturas de mandíbula no sexo masculino, média de idade de 29,9 anos. Em relação ao mecanismo de trauma, as mais comuns foram a agressão interpessoal (36,7%), acidentes automobilísticos (36,7%), ferida por arma de fogo (16%). Com relação ao tratamento, o uso de placa e parafuso foi a forma mais realizada (111 pacientes).
CONCLUSÕES: As fraturas de mandíbula são causadas principalmente por agressão interpessoal, são mais incidentes em homens e jovens. As fraturas múltiplas estão presentes em quase metade dos pacientes. Nas fraturas únicas, a região do côndilo e parassínfise foram, ambas, as mais acometidas. O tratamento cruento foi o mais empregado, sendo a reconstrução com placa de titânio a forma mais comum.
Palavras-chave: Mandíbula; Fraturas maxilomandibulares; Face; Tratamento.
The mandible is a U-shaped bone that joins with the temporal bone and has the following as anatomical units: the condylar process, coronoid process, ramus, angle, and body. It comprises the mental foramen, which gives way to the mental nerves and vessels, just below the second premolar teeth. The mandibular symphysis corresponds to the region where there is a fusion between the two body regions of the mandible. The mental protuberance is below the symphysis, and forms a triangular prominence1.
According to most studies, mandible fractures are the second most frequent type of facial injury2,3; however, the epidemiological data for this type of fracture may vary between countries, or according to the trauma mechanism and period of injury evaluation, owing to the influence of cultural, technological, environmental, and socioeconomic factors4.
The trauma mechanism has an influence on the fractured site of the mandible. Fractures caused by interpersonal violence result in lesions that are more frequently in the angle, whereas traffic accidents cause lesions that are more frequently in the parasymphyseal and condylar regions. When the trauma mechanism is falling, condylar fractures are the most frequently observed injury5.
OBJECTIVE
The objective of this study was to evaluate the epidemiological profile of patients with mandible fracture hospitalized at the Cajuru University Hospital (Curitiba, PR), between January 2010 and July 2013, and to analyze the main etiologies, most commonly affected anatomical sites, treatment types, hospitalization times, and possible complications in these patients.
METHODS
A retrospective, descriptive observational study was performed with 236 patients hospitalized at the Cajuru University Hospital, from January 2010 to July 2013, in whom mandible fracture was diagnosed and who were attended at the Maxillofacial Surgery Service of the hospital.
Only patients with complete records of age, sex, trauma mechanism, affected anatomical region, hospitalization time, and type of treatment received were included in the study, resulting in a total of 150 patients. The data were tabulated by using the collected information.
Multiple fractures were defined as the association of two or more fractures that affected the mandibular bone in different regions. Comminuted fracture was defined as a situation in which a single region was affected in multiple ways, presenting one or more fragments closely related to the fracture site. Complex fractures involved situations in which the locoregional noble anatomic structures were affected, with exposure and loss of bone substance or/and soft and dental tissues.
RESULTS
From the 150 records analyzed, 133 patients were male, corresponding to 88.66% of the total patients, and only 17 were female, corresponding to 11.33%.
The patients' age ranged between 6 and 75 years, with an average of 30 years for males and 28.6 years for females. The overall average age of the patients from this study was 29.9 years.
The ages were also divided by decades, with patients in the age range from 20 to 29 years being the most affected (n = 65), followed by the 30-39-yearold group and the 10-19-year-old group. The younger patients were less affected, with only one record of a patient between 0 and 9 years old.
Concerning the trauma mechanisms, the following causes were observed, in decreasing order of incidence: interpersonal violence (36.7%) and traffic accidents (36.7%) as the main trauma mechanisms, wounds caused by firearms (16%), falling (6.7%), sports-related accidents (2.7%), and other causes (1.3%) (Table 1).
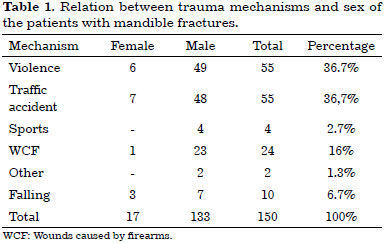
Concerning traffic accidents, motorcycle accidents corresponded to 14%, followed by car accidents (12%), bicycle accidents (6%), and being run over by a vehicle (4.7%).
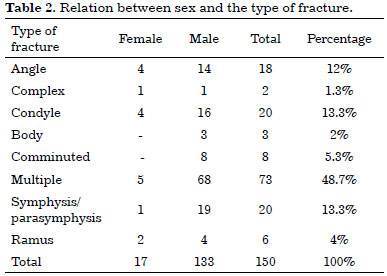
Multiple fractures were found in almost half of the patients (48.7%), followed by simple fractures in the condyle and symphysis/parasymphysis, each corresponding to 13.3% of the cases. The angle of the mandible was fractured in 12% of the patients, comminuted fractures were present in 5.3%, fracture of the ramus of the mandible was observed in 4%, and fractures in the body were found in 2%. Complex fractures were the least common, with only two cases recorded, corresponding to 1.3% of the patients.
When comparing the type of fracture by sex, multiple fractures were the most common injury in both males and females.
Concerning isolated fractures, 19 cases in the symphysis/parasymphysis regions, 16 cases in the condylar region, and 14 cases in the angle were observed, all occurring in males (Table 2).
Among the different forms of multiple fractures that were more common, involvement of the angle in association with the parasymphysis was observed in a total of 20 patients. Concomitant condylar and parasymphysis fractures were recorded in 16 patients, and angle with body fractures were present in 10 patients.
The most prevalent isolated anatomical region in the cases with multiple fractures was the angle (33%), followed by the parasymphysis (30.2%), condyle (16%), body (14%), and ramus (6.7%) (Figure 1).
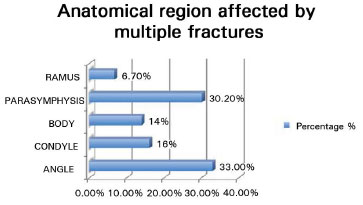
Figure 1. Relation between the anatomical regions in multiple fractures.
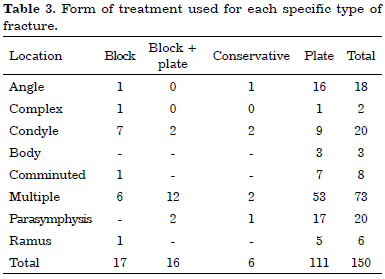
The treatment used was directly related to the type of fracture (multiple, comminuted, or complex) and to the involved anatomical region.
Mandibular reconstruction with the use of plates and screws was performed on 111 patients, whereas a block was used in 17 patients, and a combination of the two forms (block + plate) was used in 16 cases. Conservative treatment was chosen in only six cases. The treatment used for each type of fracture is described in table 3.
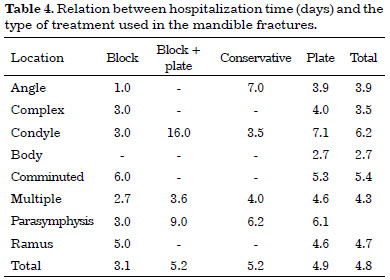
The average hospitalization time of the patients was 4.8 days, varying according to the anatomical site affected and the treatment used (Table 4).
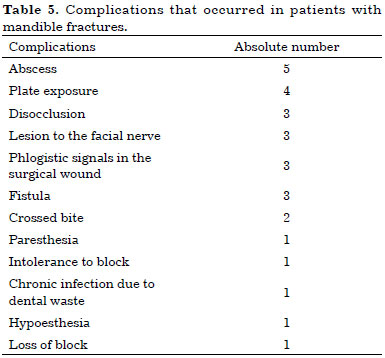
From the 150 patients studied, 28 (18.6%) showed progression to one or more complications, as described in table 5.
DISCUSSION
The literature shows that mandible fractures are, on the basis of incidence, the second most common type of fracture affecting the face, and mostly occurs in males.
The male predominance is probably due to cultural and social factors, such as the higher number of male drivers and the higher proportion of alcohol and drug users among males4,6-12.
There is a consensus in the literature about the age group more affected by mandible fractures, i.e., the 20-29-year age group4,6-12.
The results of the present study are in agreement with the literature data in terms of both sex (being male) and age predominance.
Interpersonal violence and traffic accidents were the most frequent trauma mechanisms in the patients in this study; this is corroborated by international studies, but is in contrast to some of the studies performed in Brazil6,7,10,11,13,14. In a review performed in a London hospital6 between 2005 and 2010, which evaluated mandible fractures in 1261 patients, the most common cause found was interpersonal violence (72%), followed by falling (18%). In another study, performed with 1067 patients with mandible fractures, interpersonal violence was also the most common trauma mechanism7.
However, Brazilian studies suggest that traffic accidents are the predominant cause of mandible fractures. Silva et al.13 showed that motorcycle accidents were the main cause of fractures in more than half of the patients (55.7%), followed by interpersonal violence (11.45%) and being run over by a vehicle (7.17%). Similarly, Costa et al.14 reported that traffic accidents corresponded to almost half (48.8%) of the analyzed causes.
In the present study, single fractures of the mandible had a higher incidence in the condyle and parasymphysis, and secondly, in the angle. On the other hand, in multiple fractures, the angle was the most affected anatomical site, followed by the parasymphysis, condyle, and body.
Similarly, in an epidemiological study on mandible fractures performed at a public hospital in São Paulo, almost half of the mandible fractures were observed in the body of the mandible (47.4%), followed by the condyle region (30.7%)10.
Concerning treatment, the data found here correlated with data from the literature3,4,8,12, in which mandible reconstructions with titanium plates were the most commonly performed method. Conservative treatment was chosen for only six patients in the present study.
The average hospitalization time of the patients was 4.8 days, varying according to the treatment used and the fracture site. In general, patients with fractures in the condyle and parasymphysis remained in the hospital for longer periods (6.2 and 6.1 days, respectively), whereas patients with single fractures in the body of the mandible remained hospitalized, on average, for only 2.7 days. The use of a maxillomandibular block with a titanium plate caused a more prolonged hospitalization time for the patients, in general 5.2 days, whereas the exclusive use of a maxillomandibular block was associated with a lower average hospitalization time.
The increase in hospitalization days may have been due to the need for observation and treatment of associated lesions, according to the complexity of the trauma.
Among the complications, abscess formation and plate exposure were the most common. Patients who developed some kind of complication corresponded to 18.6% of the total, which was a result similar to that found in the literature3,4,8.
Andrade Filho et al.12 described that 15.6% of patients had some complication, among which the development of an infection was the most common. Furthermore, Costa et al.14 reported a rate of complication of 10%, with osteomyelitis being the most frequent.
CONCLUSION
Mandible fractures represent an important cause of morbidity and cost related to facial trauma. They are mainly caused by interpersonal violence, firearms-related injury, and traffic accidents, and are more common in young males.
Multiple fractures were present in almost half of the patients (48.7%), with fractures of the angle associated with the parasymphysis being the most common type. In single fractures, the condyle and parasymphysis were equally the most affected regions (13.3%).
Open treatment was the most commonly used method, with reconstruction with a titanium plate being the most common approach. Conservative treatment was used in only six patients.
REFERENCES
1. Moore KL, Dalley AF. Anatomia Orientada para a Clínica. 4a ed. Rio de Janeiro: Guanabara Koogan; 2001.
2. Brook IM, Wood N. Aetiology and incidence of facial fractures in adults. Int J Oral Surg. 1983;12(5):293-8.
3. van Hoof RF, Merkx CA, Stekelenburg EC. The different patterns of fractures of the facial skeleton in four European countries. Int J Oral Surg. 1977;6(1):3-11.
4. Zix JA, Schaller B, Lieger O, Saulacic N, Thorén H, Iizuka T. Incidence, aetiology and pattern of mandibular fractures in central Switzerland. Swiss Med Wkly. 2011;141:w13207. PMID: 21618147
5. King RE, Scianna JM, Petruzzelli GJ. Mandible fracture patterns: a suburban trauma center experience. Am J Otolaryngol. 2004;25(5):301-7.
6. Rashid A, Eyeson J, Haider D, van Gijn D, Fan K. Incidence and patterns of mandibular fractures during a 5-year period in a London teaching hospital. Br J Oral Maxillofac Surg. 2013;51(8):794-8.
7. Fridrich KL, Pena-Velasco G, Olson RA. Changing trends with mandibular fractures: a review of 1,067 cases. J Oral Maxillofac Surg. 1992;50(6):586-9.
8. Atanasov DT. A retrospective study of 3326 mandibular fractures in 2252 patients. Folia Med (Plovdiv). 2003;45(2):38-42.
9. Larsen OD, Nielsen A. Mandibular fractures. I. An analysis of their etiology and location in 286 patients. Scand J Plast Reconstr Surg. 1976;10(3):213-8. PMID: 1053451
10. Leporace AAF, Paulesini Júnior W, Rapoport A, Denardin OVP. Estudo epidemiológico das fraturas mandibulares em hospital público da cidade de São Paulo. Rev Col Bras Cir. 2009;36(6):472-7.
11. Montovani JC, de Campos LM, Gomes MA, de Moraes VR, Ferreira FD, Nogueira EA. Etiology and incidence facial fractures in children and adults. Braz J Otorhinolaryngol. 2006;72(2):235-41. PMID: 16951858
12. Andrade Filho EF, Fadul Júnior R, Azevedo RAA, Rocha MAD, Santos RA, Toledo SR, et al. Fraturas de mandíbula: análise de 166 casos. Rev Assoc Med Bras. 2000;46(3):272-6.
13. Silva JJL, Lima AAAS, Dantas TB, Frota MHA, Parente RV, Lucena ALSPN. Fratura de mandíbula: estudo epidemiológico de 70 casos. Rev Bras Cir Plást. 2011;26(4):645-8.
14. Patrocínio LG, Patrocínio JA, Borba BHC, Bonatti BDS, Pinto LF, Vieira JV, et al. Fratura de mandíbula: análise de 293 pacientes tratados no Hospital de Clínicas da Universidade Federal de Uberlândia. Braz J Otorhinolaryngol. 2005;71(5):10-7.
1. Hospital Universitário Cajuru, Curitiba, PR, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
3. Pontifícia Universidade Católica do Paraná, Curitiba, PR, Brazil
Institution: Hospital Universitário Cajuru. Curitiba, PR, Brazil.
Corresponding author:
Alexandre Tieppo Zarpellon
Rua Euclides da Cunha, 1295, Bigorrilho
Curitiba, PR, Brazil Zip Code 80730-360
E-mail: alexandretzplastica@gmail.com
Article received: April 17, 2014.
Article accepted: December 13, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter