

Case Report - Year 2015 - Volume 30 -
Cutaneous pilar leiomyoma: case report and analysis of therapeutic possibilities
Leiomioma cutâneo piloeretor: relato de caso e análise de possibilidades terapêuticas
ABSTRACT
INTRODUCTION: Cutaneous pilar leiomyoma (CPL) is a rare benign skin tumor arising from arrector pili muscles. Its most common clinical manifestation is the appearance of nodules that may either be isolated or clustered. In general, these tumors are painful and sensitive to cold, touch, pressure, and emotional stimuli. Several pharmacological agents have been used with some success to reduce local pain and discomfort. However, in cases with intensely painful symptoms or that cause social constraints to the patient, surgery becomes an alternative approach. Here, we report the case of a male patient with multiple cutaneous leiomyomas in the left anterior chest wall and abdomen, and the therapeutic approaches used for this case.
METHODS: The treatment included a complete surgical resection of the tumor and wound closure with partial skin graft taken from the anterolateral region of the right thigh.
RESULTS: The immediate reconstruction of the resulting defect with a partial skin graft ensured healing without complications. After the treatment, complete remission of the pain symptoms occurred, in addition to an acceptable aesthetic outcome, which allowed the full social reintegration of the patient.
CONCLUSION: CPL is a disease that is difficult to treat; however, several therapeutic approaches can be used. The complete surgical resection of multiple cutaneous leiomyomas can prevent the recurrence of the disease, although some local recurrences have been reported in the literature.
Keywords: Leiomyoma; Skin graft; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: O leiomioma cutâneo piloeretor (LCP) é um tumor benigno de pele, de incidência rara, proveniente do músculo eretor do pelo. Sua apresentação clínica mais frequente é o aparecimento de nódulos isolados ou em grande número. Em geral, são dolorosos, sensíveis ao frio, toque, pressão e à emoção. Vários agentes farmacológicos têm sido utilizados com algum sucesso para redução da dor e do desconforto local. Entretanto, em casos nos quais os sintomas dolorosos são intensos ou causam restrição social, a cirurgia torna-se uma abordagem alternativa a ser considerada. Neste artigo relatamos o caso de um paciente do sexo masculino, portador de múltiplos leiomiomas cutâneos na parede torácica anterior à esquerda e no abdome, bem como a terapêutica utilizada para seu caso.
MÉTODOS: O tratamento compreendeu a ressecção cirúrgica total da lesão, com fechamento da ferida com o uso de enxerto de pele parcial, retirado da região anterolateral da coxa direita.
RESULTADOS: A reconstrução imediata do defeito resultante, com enxerto de pele parcial, assegurou a cicatrização sem intercorrências. Após o tratamento, houve completa remissão do quadro doloroso, o que permitiu completa reintegração social do paciente, tendo sido alcançado ainda resultado estético aceitável.
CONCLUSÃO: O LCP constitui patologia de difícil tratamento, embora tenha várias possibilidades terapêuticas. A ressecção cirúrgica completa de múltiplos leiomiomas cutâneos pode impedir a recorrência da doença, embora alguma recidiva local seja relatada na literatura.
Palavras-chave: Leiomioma; Enxerto de pele; Procedimentos cirúrgicos reconstrutivos.
Leiomyomas are benign soft tissue tumors arising from smooth muscle. These tumors can be classified into three types: piloleiomyoma, when it originates in the arrector pili muscle; dartoid leiomyoma, when it arises from the dartos muscles of the genitalia, areola, and nipple; or angioleiomyoma, when it affects the smooth muscle of the vessels (tunica media)1,2.
Initially described by Virchow in 18543, the most common type of cutaneous leiomyoma is the piloleiomyoma, which most often appears during the second or third decade of life4.
The usual clinical manifestation is the presence of papules or nodules with a diameter of < 2 cm, reddish-brown color, smooth surface, and firm consistency. These tumors remain attached to the skin without invading the deep planes and present a high number of soft lesions on palpation5.
Multiple lesions occur in 80% of the cases6, and commonly affect the face, trunk, or extremities. Several distribution patterns have been found, of which the asymmetrical pattern is the most common1. However, bilateral symmetrical presentations, i.e., dermatomes distributed in rows and linearly, are reported. Isolated cutaneous pilar leiomyoma (CPL) more commonly affects the lower extremities. As CPL develops in the superficial dermis, these tumors are attached to the skin. However, CPLs can also develop in deeper subcutaneous planes1.
The inherited form, which causes multiple fibroids in women, was first observed by Kloepfer et al.7 in 1958. Cases of familiar multiple cutaneous leiomyomas are described as an autosomal dominant inheritance, with incomplete penetrance6.
CPL has an equal incidence in men and women, and no specific preference for ethnicity has been described in the literature3. Women who have multiple CPLs may also have uterine leiomyomas. The combination of familiar multiple piloleiomyomas with uterine leiomyomas is called cutis et uteri leiomyomatosis or Reed's syndrome8. Reed's syndrome is an autosomal dominant inheritance with incomplete penetrance; therefore, not all women in the same family are affected, and those who are affected may present only cutaneous or uterine manifestations, or both3.
Malignant transformation seems not to occur. However, an article published in 20065 reported a case in which the patient developed a leiomyosarcoma with myxoid change, found in the scar of a surgically resected CPL 3 years previously. However, it was confirmed that the case was a malignant transformation of the initial injury.
The most common symptom in patients with CPL is pain, which can be spontaneous or induced by cold, pressure, friction, or emotional or tactile stimulation. Pain or tenderness may be secondary to the pressure exerted on nerve fibers within the tumor, although some authors believe that it may be caused exclusively by the contraction of muscle fibers3. Pain may also be worsened by contact with cold objects or during the winter. Although rare, concomitant erythrocytosis has also been described2. The differential diagnosis should include painful nodular skin tumors such as leiomyosarcoma, angiolipoma, glomus tumors, eccrine spiradenoma, neurofibroma, lipoma, and blue nevus3,6.
OBJECTIVE
Here, we report the case of a male patient with multiple cutaneous leiomyomas on the left anterior chest wall and abdomen, and the therapeutic approaches used for this case. The clinical examination revealed multiple skin lesions that manifested as brownish papular erythematous eruptions. The lesions increased gradually during the last 2 years, extending to the abdominal region as isolated lesions with small nodules, thus causing extreme pain and, consequently, important social limitations.
CASE REPORT
A 36-year-old male patient sought the services of the Ivo Pitanguy Clinic in 2011. He presented with multiple skin lesions, presenting as papules that were erythematous-brownish with a firm consistency, clustered in the upper left chest region. The lesions increased gradually during the past 2 years, becoming painful in the last year, and causing the patient important social constraints. The lesions extended to the abdominal region in a clustered pattern with small nodules. In the thoracic region, the lesions with a diameter of about 20 cm invaded the entire upper left area, from the clavicle line to the fifth intercostal space, sparing only the region of the left nipple (Figure 1). In the last year, he started to experience even more severe pain in the affected region. On clinical examination, he reported severe pain only with a gentle palpation of the site.

Figure 1. Preoperative aspect of the affected left chest region.
An excisional biopsy confirmed the diagnosis of CPL. The preoperative laboratory examination produced normal results.
A trial with botulinum toxin and topical corticotherapy with triamcinolone was carried out as a clinical treatment; however, the application of this treatment caused intense pain. As the therapy was not well tolerated by the patient, it was terminated. After 1 year, he opted for the surgical approach. He underwent surgical resection of the thoracic area affected by the tumors, and the entire dermis was removed to reach the subcutaneous tissue. Simple advancement flaps were placed on the edges of the defect, to reduce the area to be grafted (Figure 2). A partial skin graft, obtained from the anterior face of the left thigh, was used in the thoracic region and then the wound was closed with Brown bandages. Occlusive dressing was applied to the donor region. Most of the abdominal lesions were infiltrated with triamcinolone acetate, and the largest were dried.

Figure 2. Postoperative aspect at 18 months after surgery.
A biopsy of the lesions was also performed, the histopathological findings from which revealed a possible leiomyoma (Figure 3). On anatomopathological examination, the macroscopic finding revealed an irregular, brownish elastic fragment. Under light microscopy, a nodular lesion composed of relatively organized smooth muscle bundles, interspersed with thick wall vessels formed by smooth muscle cells arranged concentrically, with partially patent lumens, was observed.
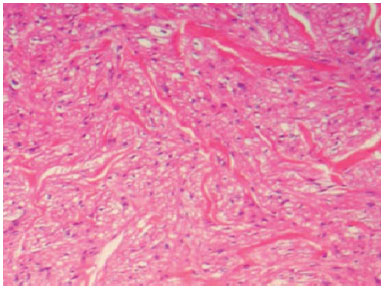
Figure 3. Spindle cell neoplasm with multidirectional beams formed by spindle cells with elongated nuclei and blunt edges. Hematoxylin and eosin stain, x100.
The postoperative course was uneventful, with a full integration of the graft. The outcome of the surgery was functionally and aesthetically evaluated. Functionally, there was a complete resolution of the clinical condition in the thoracic region, with partial but significant improvement of the painful condition and elevation of the papules in the abdominal region, which allowed the full restoration of the patient's social capabilities. Aesthetically, the chest scars were acceptable and continuously improving.
A new local infiltration with triamcinolone was carried out in two small high healing areas of the graft edges. No relapse of the lesion was observed to date.
Anatomical and histopathological findings
The histopathological examination revealed a solid, brownish tumor, with a diameter of 12 cm and regular edges.
The microscopic examination revealed the proliferation of elongated cells, presenting a low degree of histological aggressiveness, which suggested a leiomyoma. Histological sections showed the proliferation of smooth muscle fibers without atypia, which were arranged in longitudinal and transverse beams, separated by a poor fibro-connective vascularized stroma.
As an immunohistochemical evaluation, the streptavidin-biotin/horseradish peroxidase complex method was used to detect antigens such as vimentin, PS100, actin ML, CD34, and enolase. The tumor cells were positive against vimentin and actin ML stains, but negative for PS 100, CD34, and enolase. The histological pattern corresponded to a mesenchymal neoplasm of smooth muscle origin.
DISCUSSION
Leiomyomas are benign smooth muscle tumors most commonly found in the uterus (95%), skin (3%), and gastric and gastrointestinal tracts (1.5%). Their development in head and neck structures accounts for < 1% of cases. The exact origin of the tumors is still uncertain, and the most accepted theories state that they arise from the proliferation of muscle cells from vessel walls, arrector pili muscles, or aberrant undifferentiated mesenchyme.
According to the histological classification of tumors by the World Health Organization, leiomyomas can be divided into three groups: leiomyoma, angioleiomyoma (vascular leiomyoma or angiomyoma), and epithelioid leiomyoma (bizarre leiomyoma and leiomyoblastoma). Angiomyomas may stem from the surface or deep tissue. In both cases, the tumors seem to develop from the smooth muscle of vessels. Vascular leiomyomas are formed from smooth muscle cell bundles, relatively organized, and interspersed with thick-walled vessels. The superficial lesions consist predominantly of vessels with thick walls associated with proliferative muscle tissue. Deeper lesions are typically larger, probably owing to a delayed detection. Deeper lesions frequently present different histological changes that are not detected in superficial lesions, including increased cellularity and myxoid substance accumulation. Fibrosis, calcifications, and giant cell reaction may also be noted. Morimoto, in 1973, histologically classified these tumors into three types: (i) capillary or solid, (ii) cavernosum, and (iii) venous. In the extremities, these tumors are predominantly solid, whereas in the head and neck, they are mostly venous7,9. The histopathological differential diagnosis includes hemangioma, angiofibroma, fibroids, leiomyoblastoma, angiomyolipoma, and vascular leiomyosarcoma9.
Some reports have described the malignant tumor variants of this lineage; however, they are rare. The absence of mitosis appears to be the best indicator of the benignity of the lesion9.
Angioleiomyomas are more common in women than in men (ratio, 2:1). Although the solid subtype occurs predominantly in women (3:1), the venous subtype develops more frequently in men, and the least common of the three-the cavernous subtype-is four times more common in men3,9. Concerning angioleiomyomas of the oral region, the average age of patients was 45 years old, with a sex ratio of 3:1 (men vs. women). The most commonly affected site was the lip (in 48.6% of patients), followed by the palate (21.1%), oral mucosa and tongue (9.2%), and mandible (8.3%)10.
Cutaneous leiomyomas are rare benign skin tumors that present in a disseminated, segmental, or isolated form. The pathogenesis of skin segmental leiomyomatosis is not fully known. Two types of autosomal dominant inheritance manifestations have been postulated: type 1 reflects a heterozygous mutation, whereas type II reflects the presence of a homozygous gene mutation with a pronounced expression of segmental defects in the affected segment11-13.
Rarely, leiomyoma can arise from the arrector pili muscle of the skin. These tumors affect teenagers or young adults, usually on the extensor surfaces of the extremities.
One characteristic of mammals is having a body covered by hairs. The hairs are protective structures; they become erect in the presence of a stimulus indicating a need for protection. This phenomenon occurs at low temperatures or in situations in which fear is elicited. The arrector pili muscles, which are responsible for the erection of the hairs, are generally located at the base of the hair shafts.
The lesions are often multiple and very painful. Approximately 90% of patients report a condition associated with pain, which is typically caused by cold temperatures, trauma, or a simple touch to the skin. Several theories have been postulated to explain the physiopathogenesis of the pain, including pressure on the nerve fibers and abnormal muscle contraction. It is also known that the autonomic sympathetic nervous system stimulates the arrector pili muscle. Norepinephrine, secreted by postganglionic nerve fibers, activates the alpha-receptors of the muscle. This causes muscle contraction, which is triggered by the influx of ions and, more specifically, calcium. Understanding the underlying physiopathological process can be relevant for the medical treatment of symptomatic leiomyomas14.
Surgical removal is always advocated as a treatment option in the case of isolated cutaneous leiomyomas or when the total number of lesions is small. In symptomatic patients, surgical excision can be considered also for larger lesions. Although benign, these tumors can relapse after excision.
Cosmetically, the excision of multiple CPLs is a bigger problem and is less effective than the excision of isolated leiomyomas. The recurrence of these lesions is also more common in cases of multiple CPLs. After excision, a 50% recurrence rate occurs within a period ranging from 6 months to 15 years3.
CPL is histologically characterized by multidirectional beams formed by spindle-shaped cells, which resemble smooth muscle bundles. The tumor has no capsule and is usually located in the middle and deep dermis. The nuclei are elongated, monomorphic, and with blunt ends6. The smooth muscle differentiation markers desmin and actin may be detected by means of immunohistochemical analysis3,6.
Several dyes and immunohistochemical tests have been used to identify vascular leiomyomas, including desmin, vimentin, Masson trichrome, actin, and myosin. However, these methods are not necessary for the diagnosis.
The treatment of these tumors is based on local resection, with no reports of recurrence after a total excision1,3.
In this case, the choice of excision resulted from the failure of medical treatment and the worsening of the painful condition presented by the patient. Previous literature reports have demonstrated total excision of multiple CPLs, followed by grafting with artificial grafts, also obtaining successful results15.
Another option is abrasion with a carbon dioxide laser, for which pain relief after a follow-up of 3-9 months has been reported. The procedure is performed under local anesthesia. Cryosurgery is another treatment option. However, these two options, in general, do not allow for the removal of the lesion, but only decrease its thickness16.
Concerning clinical treatment, several medications can be used for relieving the symptoms. In cases of numerous and painful CPLs, medication is recommended; however, its effectiveness is limited. The medication options include analgesics, nifedipine, phenoxybenzamine, and an alpha-adrenergic blocker reported to be a useful analgesic, including against cold-induced pain, in some cases17.
Gabapentin also seems to play a role in pain relief, with varying results. However, randomized studies have not been conducted thus far18.
Hyoscine can reduce the pain associated with the lesions, through the induction of muscle relaxation mechanisms. The inhibition of nicotinic receptors induces a ganglionic block, which is responsible for the effect. It is a relatively safe medication; however, high doses can lead to anticholinergic effects such as dry mouth and blurred vision19.
There are two cases in the literature that describe the use of botulinum toxin for the relief of pain associated with CPL, although they also suggest the possibility of a placebo effect20,21. The authors report that the use of botulinum toxin resulted in a decreased intensity and frequency of pain, with no adverse effects observed. The use of botulinum toxin, however, might cause significant pain episodes in certain patients, making this indication questionable. The need for general anesthesia or sedation and analgesia for a short period of therapy (approximately 4 months) may also be unsatisfactory20,21. The combination of medication with analgesics can be performed without the concern for drug interactions. However, the economic condition of the country is an important consideration, because the high cost of the medication restricts its use for treatment.
CONCLUSION
A complete surgical resection of multiple cutaneous leiomyoma prevents the recurrence of the disease. The immediate reconstruction of the resulting overall thickness defect, with a partial skin graft, ensures healing without complications, with the optimal achievement of functional and aesthetic results, as well as a total relief from the discomfort caused by the CPL.
REFERENCES
1. Lun KR, Spelman LJ. Multiple piloleiomyomas. Australas J Dermatol. 2000;41(3):185-6. PMID: 10954993 DOI: http://dx.doi.org/10.1046/j.1440-0960.2000.00427.x
2. Holst VA, Junkins-Hopkins JM, Elenitsas R. Cutaneous smooth muscle neoplasms: clinical features, histologic findings, and treatment options. J Am Acad Dermatol. 2002;46(4):477-90. PMID: 11907496 DOI: http://dx.doi.org/10.1067/mjd.2002.121358
3. Virchow R. Über Makroglossie und pathologische Neubildung quergestreifter Muskelfasern. Virchows Arch. 1854;7:126-38. DOI: http://dx.doi.org/10.1007/BF01936233
4. Christenson LJ, Smith K, Arpey CJ. Treatment of multiple cutaneous leiomyomas with CO2 laser ablation. Dermatol Surg. 2000;26(4):319-22. DOI: http://dx.doi.org/10.1046/j.1524-4725.2000.99250.x
5. Utikal J, Haus G, Poenitz N, Koenen W, Back W, Dippel E, et al. Cutaneous leiomyosarcoma with myxoid alteration arising in a setting of multiple cutaneous smooth muscle neoplasms. J Cutan Pathol. 2006;33 Suppl 2:20-3. DOI: http://dx.doi.org/10.1111/j.1600-0560.2006.00491.x
6. Alper M, Parlak AH, Kavak A, Aksoy KA. Bilateral multiple piloleiomyomas on the breast. Breast. 2004;13(2):146-8. DOI: http://dx.doi.org/10.1016/S0960-9776(03)00134-6
7. Kloepfer HW, Krafchuk J, Derbes V. Hereditary multiple leiomyoma of the skin. Am J Hum Genet. 1958;10(1):48-52. PMID: 13520698
8. Pacheco AP, Ramos AMO, Rolim MLM, Oliveira FMD, Lopes JG, Rocha KF. Piloleiomioma múltiplo: relato de caso com diagnóstico diferencial. An Bras Dermatol. 1995;70(1):43-6.
9. Ramesh P, Annapureddy SR, Khan F, Sutaria PD. Angioleiomyoma: a clinical, pathological and radiological review. Int J Clin Pract. 2004;58(6):587-91. DOI: http://dx.doi.org/10.1111/j.1368-5031.2004.00085.x
10. Brooks JK, Nikitakis NG, Goodman NJ, Levy BA. Clinicopathologic characterization of oral angioleiomyomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(2):221-7. PMID: 12221390 DOI: http://dx.doi.org/10.1067/moe.2002.125276
11. Lang K, Reifenberger J, Ruzicka T, Megahed M. Type 1 segmental cutaneous leiomyomatosis. Clin Exp Dermatol. 2002;27(8):649-50. PMID: 12472537 DOI: http://dx.doi.org/10.1046/j.1365-2230.2002.01089.x
12. Badeloe S, van Geel M, van Steensel MA, Bastida J, Ferrando J, Steijlen PM, et al. Diffuse and segmental variants of cutaneous leiomyomatosis: novel mutations in the fumarate hydratase gene and review of the literature. Exp Dermatol. 2006;15(9):735-41. DOI: http://dx.doi.org/10.1111/j.1600-0625.2006.00470.x
13. Garman ME, Blumberg MA, Ernst R, Raimer SS. Familial leiomyomatosis: a review and discussion of pathogenesis. Dermatology. 2003;207(2):210-3. PMID: 12920381 DOI: http://dx.doi.org/10.1159/000071802
14. Horner KL. Leiomyoma [Citado 12 Out 2015]. Available from: http://www.emedicine.com/DERM/topic217.htm
15. Gravvanis A, Kakagia D, Papadopoulos S, Tsoutsos D. Dermal skin template for the management of multiple cutaneous leiomyomas. J Cutan Med Surg. 2009;13(2):102-5. DOI: http://dx.doi.org/10.2310/7750.2008.07074
16. Christenson LJ, Smith K, Arpey CJ. Treatment of multiple cutaneous leiomyomas with CO2 laser ablation. Dermatol Surg. 2000;26(4):319-22. DOI: http://dx.doi.org/10.1046/j.1524-4725.2000.99250.x
17. Batchelor RJ, Lyon CC, Highet AS. Successful treatment of pain in two patients with cutaneous leiomyomata with the oral alpha-1 adrenoceptor antagonist, doxazosin. Br J Dermatol. 2004;150(4):775-6. PMID: 15099382 DOI: http://dx.doi.org/10.1111/j.0007-0963.2004.05880.x
18. Scheinfeld N. The role of gabapentin in treating diseases with cutaneous manifestations and pain. Int J Dermatol. 2003;42(6):491-5. PMID: 12786883 DOI: http://dx.doi.org/10.1046/j.1365-4362.2003.01831.x
19. Clissold SP, Heel RC. Transdermal hyoscine (Scopolamine). A preliminary review of its pharmacodynamic properties and therapeutic efficacy. Drugs. 1985;29(3):189-207. PMID: 3886352 DOI: http://dx.doi.org/10.2165/00003495-198529030-00001
20. Sifaki MK, Krueger-Krasagakis S, Koutsopoulos A, Evangelou GI, Tosca AD. Botulinum toxin type A--treatment of a patient with multiple cutaneous piloleiomyomas. Dermatology. 2009;218(1):44-7. PMID: 19001802 DOI: http://dx.doi.org/10.1159/000173695
21. Onder M, Adişen E. A new indication of botulinum toxin: leiomyoma-related pain. J Am Acad Dermatol. 2009;60(2):325-8. DOI: http://dx.doi.org/10.1016/j.jaad.2008.05.044
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Pontifícia Universidade Católica do Rio de Janeiro, Rio de Janeiro, RJ, Brazil
3. Instituto PMG Carlos Chagas, Rio de Janeiro, RJ, Brazil
4. Instituto Ivo Pitanguy, Rio de Janeiro, RJ, Brazil
Institution: Instituto Ivo Pitanguy, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Bárbara Helena Barcaro Machado
Rua Dona Mariana, 65, Botafogo
Rio de Janeiro, RJ, Brazil Zip Code 22221-000
E-mail: barbara@barbaramachado.com.br
Article received: March 5, 2012.
Article accepted: September 15, 2012.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter