

Case Report - Year 2016 - Volume 31 -
Complications in sefel-injection of chemicals to increase muscle
Complicações de autoinjeção de agentes químicos para aumento muscular
ABSTRACT
The number of gym goers who self-inject oily substances to increase muscle volume artificially and thereby improve the aesthetic appearance of their muscles that are unresponsive to training is increasing. Although immediate effects and satisfactory aesthetic results such as increased volume or changes in the contour of several areas of the body might be observed, oil infiltration might cause several short- and long-term complications, which are often irreversible. The awareness and actions of medical and health professional societies are fundamental for the prevention and control of this problem. In this article, possible complications are reviewed, and the case of a patient with severe local complications caused by oil injection is reported.
Keywords: Mineral oil; Vitamin and mineral-based medicines; Adverse reaction.
RESUMO
O número de frequentadores de academia que utilizam injeções de substâncias oleosas para aumentar o volume muscular artificialmente, buscando, com essa prática, uma melhora cosmética dos músculos que não responderiam aos treinamentos, vem aumentando. Apesar dos efeitos imediatos e dos bons resultados estéticos como aumento de volume ou modificação do contorno de várias áreas do corpo, a infiltração de óleo pode levar a diversas complicações a curto e longo prazo, que muitas vezes são irreversíveis. A conscientização e atuação das entidades de classes médicas e sanitárias tornam-se fundamentais na profilaxia e controle deste problema. Neste artigo revisamos as complicações e ainda relatamos o caso de um paciente com complicações locais importantes secundárias a injeção de óleo.
Palavras-chave: Óleo mineral; Medicamentos à base de vitaminas e minerais; Reação adversa.
The injection of liquid chemicals such as oils has been used for several decades as a nonsurgical intervention to increase body contour1,2. This practice may be associated with severe late complications and has been the subject of controversy within the medical community.
This might lead to local and systemic complications that are due to the infiltration of oily substances, especially when these cosmetic procedures are performed by non-physicians. Nowadays, this practice is common among bodybuilders3,4. Disfigurement, erratic migration, tumors, granulomatous and sclerosing lesions, ulcerations, lung diseases, and severe complications such as pulmonary embolism and death have been widely described in the literature1,3,5-10.
Injections of oily substances might also cause foreign body reactions, named paraffinoma and oleoma according to the material injected4.
The areas that are frequently affected are the anterior chest, breasts1,3,4, buttocks9,10, and genitals2,6-8,11,12.
The aim of this study was to revise the complications caused by the self-injection of chemical substances used to increase the volume of specific anatomic areas. Moreover, the objective of this study was to report a case of mineral oil self-injection in the chest and upper limbs, and present the preliminary results of surgical treatment in a series of patients.
REVIEWING COMPLICATIONS
The use of filling substances for reconstruction or aesthetic purposes is an old practice, implemented in 1899 by the Austrian surgeon Robert Gersuny, who injected mineral oil in the scrotum of a patient to mimic his lost testicle13,14.
Since the beginning of its implementation, the adverse effects caused by the application of oily substances have been reported and published in the medical literature. These include skin inflammation, hard edema, sterile abscesses and diffuse lymphangitis15, calcifications in the affected tissues, and vasculitis16. In 1906, Heidingsfeld described disfiguring subcutaneous nodules in two patients who applied paraffin oil to facial rhytides17.
The term paraffinoma or oleoma is used to define a non-allergic reaction to a foreign body that is caused by the injection of oily mineral, vegetable, or animal substances that leads to the formation of irregular and hard plaques in the skin and subcutaneous tissue, which may subsequently favor the development of an ulcer18.
One of the sites of injection for volume increase that is most reported in the literature is the penis. The use of these oils on the penis might cause deformities, necrosis, impaired erectile function, and ulcerations, in addition to paraffinoma19,20.
Despite the adverse effects that have been reported, the number of bodybuilders self-injecting oils to increase their muscle volume artificially increased. Such gym goers see an aesthetic improvement in muscles that otherwise would not respond to training. The first case reported in the Brazilian scientific literature dates back to the end of the 1980s16.
Systematic intramuscular injections of oily substances trigger a local volume increase. However, this increase is not related to muscular hypertrophy or any adaptive physiological event, thus having only a suspicious aesthetic effect, as the result is that muscle appearance may no longer present a normal muscle anatomy. The volume injected occupies space in the application site, that is, within the muscle or in the adjacent subcutaneous tissue, which is not absorbed by the body, thus resulting in a foreign body reaction. Histological analysis would reveal what is called a "Swiss cheese pattern" of the oleoma, as the histological appearance shows the presence of fat lobules surrounded by giant cells, foamy macrophages, and fibrous tissue.
The latency between the infiltration of the substance and the occurrence of this reaction is quite varied and may range from several days to many years after injections18.
Darsow et al.3 reported a case of subcutaneous nodules in a bodybuilder, which were caused by the injection of sesame oil to increase his muscle in the injected site. Koopman et al.21 also reported a case of a patient who was injecting sesame oil in his biceps, shoulders, and lower limbs, which resulted in the development of vasculitis. The individual presented large skin lesions in the application sites, with edema and necrosis in the injected muscles.
Restrepo et al.10 described the case of two bodybuilders and six transsexuals who had severe respiratory complications after silicone fluid injections, which caused the death of two of the individuals. These bodybuilders injected silicone in chest muscles and arms.
Another rare complication, although reported in the literature, is the case of a patient with epidermoid carcinoma of the penis that was caused by injection of mineral oil22.
When possible, the treatment of choice is complete resection of the affected tissue to prevent the recurrence of adverse reactions8,23. The surgical treatment should involve closure without tension and partial, if necessary, conducting more of one intervention.
The injection of these substances is mostly performed by non-physicians who are unaware of the origin of the chemical used and, in particular, unconscious of the deleterious consequences of this illegal practice. Moreover, these patients should undergo controlled psychological monitoring in order to learn how to live with permanent deformities and possible complications caused by the injection of these substances.
CASE REPORT
A 33-year-old male patient reported to have started mineral oil applications upon indication in the gym environment. He had consecutive serial applications for 3 months on the anterior chest and arms, and then suspended the application 2 years prior. Few months after the last injection, the patient already presented extended lesions in the anterior chest and arms, which were characterized as masses, and firm and irregular nodules in the subcutaneous tissue that adhered to the deep planes, in addition to a violet discoloration of the affected skin (Figure 1).

Figure 1. Preoperative appearance: Extended lesions characterized by the presence of masses, firm and irregular nodules in the subcutaneous tissue that adhered to deep planes, and violet discoloration of the skin on the upper limbs and chest. A: Frontal appearance. B: Frontal appearance with upper limbs abducted. C: Posterior appearance. D: Left profile appearance.
An undesired and irregular extravasation into the forearms was also detected, mostly on the left side. The growth of the lesions stabilized, was always painless, and remained stable until now. No compressive symptoms or other complaints were reported by the patient. The patient did not show any comorbidity, although he complained about the damage that this caused to his personal life. He referred to his limbs in his complaints but was unwilling to talk about the thoracic region.
Ultrasonography of the limbs showed a thick and highly echogenic subcutaneous tissue, with oval and elongated cystic areas in between, resembling a foreign body granuloma, cellulite, and/or vascular neoformation. Computed tomography revealed thickening and edema of the subcutaneous tissue and muscles of the arms.
After a preoperative evaluation, the patient underwent surgery. This started in the medial aspect of the left arm, where his main complaint was located, by performing an incision similar to that performed in brachioplasty procedures (from the axillae to the elbow). During surgery, a well-vascularized fibro-adipose tissue, without cleavage plane, was detected in the surgical specimen (Figure 2). The closure was performed by plane, and suction drains were placed (Portovak ¼). The postoperative evolution was satisfactory, without infection or wound dehiscence. The final aspect of the scar was satisfactory.
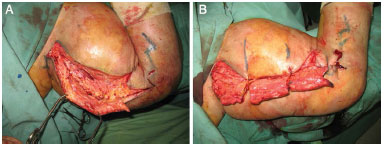
Figure 2. Intraoperative appearance in the first surgery. A: Marking and excess tissue that should be resected. B: Fibro-adipose tissue that is well-vascularized without a cleavage plane.
After 2 months, the patient underwent surgery on his left arm, which was similar to that performed on his right arm. The results of both procedures were quite few but satisfactory. The patient was satisfied with the initial change, although he was aware that the deformed aspect of his lesions was permanent, even after surgery, and knew that further interventions would be necessary in the future (Figure 3).

Figure 3. Outcome 3 months after the second surgery. A: Frontal appearance. B: Frontal appearance with the upper limbs abducted. C: Left profile appearance.
CONCLUSION
The incidence of injection of liquid chemicals such as oils and silicone to improve body contour has shown an increase with a consistent irreversible manifestation of dysmorphic sequelae. Several complications occur after the application of these chemicals, and psychiatric disorders are often diagnosed in these patients. The association of non-medical practice with aesthetic purposes in bodybuilding gyms creates favorable conditions for the occurrence of cases similar to that presented in this study. The awareness and action of medical and health professional societies are crucial for the prophylaxis and control of this problem, as the treatment of these patients has been shown to be complex and poor.
REFERENCES
1. Chen M, Yalamanchili C, Hamous J, Piskun MA, Weis B. Acute inflammatory response of the male breasts secondary to self-injection of petroleum jelly: a case report. South Med J. 2008;101(4):422-4. PMID: 18360333 DOI: http://dx.doi.org/10.1097/SMJ.0b013e3181684ae4
2. Rollins CE, Reiber G, Guinee DG Jr, Lie JT. Disseminated lipogranulomas and sudden death from self-administered mineral oil injection. Am J Forensic Med Pathol. 1997;18(1):1003. DOI: http://dx.doi.org/10.1097/00000433-199703000-00019
3. Darsow U, Bruckbauer H, Worret WI, Hofmann H, Ring J. Subcutaneous oleomas induced by self-injection of sesame seed oil for muscle augmentation. J Am Acad Dermatol. 2000;42(2 Pt 1):292-4. DOI: http://dx.doi.org/10.1016/S0190-9622(00)90144-0
4. Munch IC, Hvolris JJ. Body building aided by intramuscular injections of walnut oil. Ugeskr Laeger. 2001;163(48):6758. PMID: 11768903
5. Chen YC, Chen ML, Chiu YM. A case of mimicking angioedema: chin silicone granulomatous reaction spreading all over the face after receiving liquid silicone injection forty years previously. Chin Med J (Engl). 2011;124(11):1747-50.
6. Bhagat R, Holmes IH, Kulaga A, Murphy F, Cockcroft DW. Self-injection with olive oil. A cause of lipoid pneumonia. Chest. 1995;107(3):875-6. PMID: 7874970 DOI: http://dx.doi.org/10.1378/chest.107.3.875
7. Akkus E, Iscimen A, Tasli L, Hattat H. Paraffinoma and ulcer of the external genitalia after self-injection of vaseline. J Sex Med. 2006;3(1):170-2. DOI: http://dx.doi.org/10.1111/j.1743-6109.2005.00096.x
8. Cohen JL, Keoleian CM, Krull EA. Penile paraffinoma: selfinjection with mineral oil. J Am Acad Dermatol. 2001;45(6 Suppl):S222-4. DOI: http://dx.doi.org/10.1067/mjd.2001.103995
9. Zamora AC, Collard HR, Barrera L, Mendoza F, Webb WR, Carrillo G. Silicone injection causing acute pneumonitis: a case series. Lung. 2009;187(4):241-4. PMID: 19430832 DOI: http://dx.doi.org/10.1007/s00408-009-9150-x
10. Restrepo CS, Artunduaga M, Carrillo JA, Rivera AL, Ojeda P, Martinez-Jimenez S, et al. Silicone pulmonary embolism: report of 10 cases and review of the literature. J Comput Assist Tomogr. 2009;33(2):233-7. PMID: 19346851 DOI: http://dx.doi.org/10.1097/RCT.0b013e31817ecb4e
11. Thomas P, Boussuges A, Gainnier M, Quénée V, Donati S, Ayem ML, et al. Fat embolism after intrapenile injection of sweet almond oil. Rev Mal Respir. 1998;15(3):307-8.
12. Behar TA, Anderson EE, Barwick WJ, Mohler JL. Sclerosing lipogranulomatosis: a case report of scrotal injection of automobile transmission fluid and literature review of subcutaneous injection of oils. Plast Reconstr Surg. 1993;91(2):352-61. PMID: 8430154 DOI: http://dx.doi.org/10.1097/00006534-199302000-00024
13. Best FW, Mason HL, DeWeerd JN, Dahlin DC. Sclerosing lipogranuloma of the male genitalia produced by mineral oil. Proc Staff Meet Mayo Clin. 1953;28(22):623-31.
14. Gersuny R. Harte und weiche paraffin prosthesen. Zentralbl Chir. 1903;30:1.
15. Di Benedetto G, Pierangeli M, Scalise A, Bertani A. Paraffin oil injection in the body: an obsolete and destructive procedure. Ann Plast Surg. 2002;49(4):391-6. DOI: http://dx.doi.org/10.1097/00000637-200210000-00010
16. Figueiredo VC, Silva PRP, Trindade RS, De Rose EH. Doping cosmético: a problemática das aplicações intramusculares de óleos. Rev Bras Med Esporte. 2011;17(1):56-61. DOI: http://dx.doi.org/10.1590/S1517-86922011000100011
17. Heidingsfeld ML. Histopathology of paraffin prosthesis. J Cutan Dis. 1906;24:513-21.
18. Magrin PF, de Oliveira Ribeiro C, Quevedo Filho LP, Barbosa Durães SM, Rochael MC. Oleoma: A case report with good response to tetracycline. Dermatol Online J. 2010;16(10):7.
19. Jeong JH, Shin HJ, Woo SH, Seul JH. A new repair technique for penile paraffinoma: bilateral scrotal flaps. Ann Plast Surg. 1996;37(4):386-93. DOI: http://dx.doi.org/10.1097/00000637-199610000-00007
20. Santucci RA, Zehring RD, McClure D. Petroleum jelly lipogranuloma of the penis treated with excision and native skin coverage. Urology. 2000;56(2):331. PMID: 10925113 DOI: http://dx.doi.org/10.1016/S0090-4295(00)00625-7
21. Koopman M, Richter C, Parren RJ, Janssen M. Bodybuilding, sesame oil and vasculitis. Rheumatology (Oxford). 2005;44(9):1135. DOI: http://dx.doi.org/10.1093/rheumatology/keh712
22. Ciancio SJ, Coburn M. Penile salvage for squamous cell carcinoma associated with mineral oil injection. J Urol. 2000;164(5):1650. PMID: 11025729 DOI: http://dx.doi.org/10.1016/S0022-5347(05)67053-X
23. Hazani R, Engineer N. Surreptitious injection of mineral oil: a case report of sclerosing lipogranulomatosis. Ann Plast Surg. 2008;61(5):555-8. PMID: 18948786 DOI: http://dx.doi.org/10.1097/SAP.0b013e31816d8316
1. Hospital São Lucas da PUCRS, Porto Alegre, RS, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital São Lucas da PUCRS, Porto Alegre, RS, Brazil.
Corresponding author:
Francisco Felipe Laitano
Rua Farnese, 199/501, Bela Vista
Porto Alegre, RS, Brazil Zip Code 90450-180
E-mail: fflpoa@hotmail.com
Article received: February 28, 2013.
Article accepted: April 13, 2013.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter