

Case Reports - Year 2016 - Volume 31 -
Surgical correction of unilateral and bilateral congenital macrostomia: a case report and literature review
Correção cirúrgica da macrostomia congênita unilateral e bilateral: relato de casos e revisão da literatura
ABSTRACT
INTRODUCTION: The incidence of craniofacial microsomia is 1 in 5600 live births. This is the second most common craniofacial anomaly after cleft lip and palate. Tessier cleft 7 is associated with 17% to 62% of cases of hemifacial microsomia. It begins on the labial commissure and may extend to the pre-auricular capillary line. Deformities of the external ear range from excessive pre-auricular skin to complete absence of the ear. Commissuroplasty is indicated in patients with macrostomia or true lateral facial cleft. The objective is to present two cases of macrostomia and perform a review of related literature.
METHODS: In this study, we describe two cases of macrostomia treated with mucous flaps and zetaplasty.
RESULTS: We obtained optimal repositioning of labial commissures in two patients, with excellent aesthetic results.
CONCLUSION: The technique used is easily reproducible, and aesthetically and functionally corrects macrostomia.
Keywords: Macrostomia; Cleft lip; Cleft palate; Craniofacial Abnormalities; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A incidência da microssomia craniofacial é de 1 em 5600 nascidos vivos. É a segunda anomalia craniofacial mais comum após as fissuras labiais e palatinas. A fissura número 7 está associada entre 17 a 62% dos casos de microssomia hemifacial e começa na comissura labial, podendo prolongar-se até a linha capilar pré-auricular. As deformidades da orelha externa vão desde excesso de pele pré-auricular até ausência completa da orelha. A comissuroplastia está indicada em pacientes com macrostomia ou fissura facial lateral verdadeira. O objetivo é demonstrar dois casos de macrostomia e fazer uma revisão da literatura sobre o tema.
MÉTODOS: Em nosso estudo descrevemos dois casos de macrostomia tratados com retalhos de mucosa e plástica em Z.
RESULTADOS: Obtivemos um ótimo reposicionamento das comissuras nos dois pacientes, com excelente resultado estético.
CONCLUSÃO: A técnica utilizada é de fácil reprodutibilidade e corrige a macrostomia estética e funcionalmente.
Palavras-chave: Macrostomia; Fenda labial; Palato; Anormalidades craniofaciais; Procedimentos cirúrgicos reconstrutivos.
Congenital macrostomia, also called transverse, horizontal, or lateral facial cleft, is a relatively rare entity1,2. Various terms have been used to describe this cleft, including the following: hemifacial microsomia, microtia, otomandibular dysostosis, unilateral facial agenesis, facial side cleft, and syndrome of the first and second branchial arches. It corresponds to cleft No. 7 of the classification of Tessier. This atypical form represents 1.5% of all clefts, being frequently associated with craniofacial microsomia (syndromes of the first and/or second branchial arches)3,4.
The incidence of bilateral macrostomia is not well defined, but varies from 1:50,000 to 1:175,0005. The etiopathogenesis of this disease is complex and multifactorial, and involves an interaction between genetic and environmental factors. As in other types of facial clefts, congenital macrostomia results from failure of the mesoderm migration between the mandibular and maxillary prominences during the fourth and fifth weeks of embryonic life (gestational period)2,6-8.
This malformation is not limited to the labial commissure, also affecting its muscular portion. Sometimes, deeper facial structures are involved, and complete facial division may occur 9. Deformities of the external ear may be present, ranging from excess skin to the absence of the pinna. In the affected side, the parotid gland or its duct may be absent. The V and VII cranial nerves, and the muscles that they innervate may be affected. The soft ipsilateral palate is generally hypoplastic. The mandibular branch can be hypoplastic, varying in three grades according to Prusanski10.
Grade I represents a smaller mandibular branch than that on the normal side, but with maintenance of form. In grade II, anatomic distortion occurs, but one can still observe the structures of the mandibular branch. Grade III is characterized by the absence or severe hypoplasia of the region of the condyle and mandibular branch. The occlusal plan is asymmetrical, reflecting the hypoplastic maxilla and lower vertical dimension of the affected mandibular branch11. In Goldenhar syndrome, a rare congenital autosomal dominant defect, in addition to the cleft, vertebral abnormalities are also present. The variable clinical expression, ranging from a forme fruste to severe cases with disfiguring malformations, obliges us to examine the children carefully1.
Some of the goals of the repair of macrostomia are the reconstruction of the orbicularis oris muscle, labial symmetry, and well-positioned scars. Surgery can be performed after 3 months of age. The position of the labial commissure should be defined by using the contralateral commissure as a parameter in unilateral cases, and the position of the pupil can be the parameter in bilateral deformities1-3,12.
The objective of this work was to report a case of unilateral left macrostomia and a case of bilateral macrostomia, and to evaluate the aesthetic and functional results of surgical treatment.
METHODS
Patient 1 (Figure 1): Male patient, 3 years old, presenting with hemifacial microsomia together with a left unilateral Tessier 7 cleft. Surgery was performed under general anesthesia. The marking of the new commissure was drawn by transferring the contralateral mucocutaneous zone, but with a 2-mm increase at the upper point. Infiltration with 2% xylocaine and epinephrine (1:200,000) was performed. The incision was performed on the mucocutaneous zone with dissection of quadrangular mucosal flaps, these being reversed to the oral cavity. The orbicularis oris muscle was dissected (Figure 2), reoriented, and sutured with nylon 4.0. The skin is then sutured after zetaplasty (Figure 3). Figure 3 was designed and drawn by the author.

Figure 1. Unilateral left macrostomia.
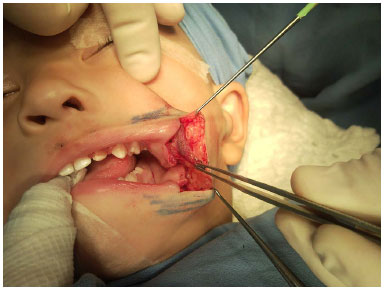
Figure 2. Dissection of the orbicularis oris muscle.
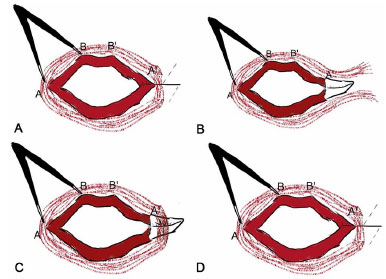
Figure 3. A: Schematic drawing: Transfer of the distance between points A and B, and marking of points A' and B' for the construction of a new commissure. The line in blue shows the location to be incised at the cutaneous mucosal transition; B: Schematic drawing: Intraoral inversion of mucosal flaps; C: Schematic drawing: Dissection, repositioning, and suture of the orbicularis oris muscle; D: Schematic drawing - Reorientation of transverse scar in the direction of the nasolabial groove through a zetaplasty.
Patient 2 (Figure 4): Male patient, 3 years old, with microsomia together with bilateral Tessier 7 cleft. Surgery was performed under the same conditions by using the same technique. The new labial commissures were marked according to the equation: distance between the commissures = x + x/2, where x represents the length of the nasal base. The quadrangular flaps and zetaplasty were similar to those used on patient 1.

Figure 4. Bilateral macrostomia.
An informed consent form was signed by parents or guardians.
RESULTS
Good aesthetic results were obtained, with the scars in good condition (Figures 5 and 6). Masticatory function and buccal opening were adequate. No ischemia was observed on the sutures, and the repositioning of the orbicularis oculi favored the functional outcome. The occlusion was improved, and the repositioning of the labial commissure was symmetrical. Neither surgical wound infection nor other complications occurred in the postoperative period. After 5 years of follow-up, the patients maintained satisfactory results.
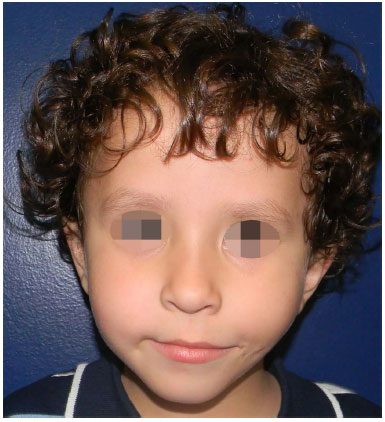
Figure 5. Five years after bilateral macrostomia correction.
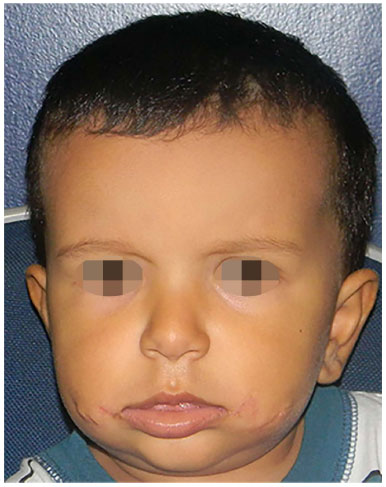
Figure 6. Two-years after correction of bilateral macrostomia.
DISCUSSION
The pathological anatomy of this deformity is well known, but the existence of different corrective techniques demonstrates the lack of consensus as to which procedure presents the best results. It is recommended to correct the defect between 3 and 12 months of life to prevent impairment of the speech process4. Early intervention is advocated for patients who present pronounced nutritional deficiency. However, at 12 months, concurrent correction of other possible associated facial changes could be attained, and thus, is preferred by most authors. When macrostomia is associated with a cleft lip, the repair of macrostomia should be performed after cheiloplasty because the balance of the upper and lower lips should be taken into account in the repair of macrostomia2.
With regard to the unilateral commissuroplasty, published data are more elaborate and the marking of the new commissure can be performed according to Mathes' method. The author used the distance between the philtrum and the commissure contralateral to the defect. This distance is then transferred to the malformed side with an overcorrection, as a scar contraction is expected.
This overcorrection is not well established, but in patient 1, we used a difference of 2 mm, which was satisfactory and reproducible. To achieve a natural labial commissural form, muscle bundles are overlain, with the upper part positioned anteriorly, and the bottom part positioned posteriorly. Thus, the muscle is reanimated, and sphincter function is achieved.
Despite being performed at an unusual age, the results were not impaired owing to the proper use of the technique. The marking with a 2-mm difference to the contralateral labial commissure favored the proper positioning of the scar. This invariably undergoes some contraction, however small. Kaplan13 reported commissuroplasty with a quadrangular flap of the upper lip, but its end does not include the vermillion and leaves a scar in the lower lip.
The scar in the lower lip and borderless vermillion become more evident over time because of the tension that is created when the mouth is open. For this reason, a mucocutaneous flap of the vermillion of the lower lip was used. The use of quadrangular flaps allowed the correct orientation of the oral mucosa. Therefore, it should be a supplementary procedure to zetaplasty. Besides fixing the orbicularis oculi, it assured that even after 5 years, the masticatory function of the patient remained adequate.
Two controversial opinions exist regarding the skin suture. One favors the use of zetaplasty, and the other states that only a linear suture of the wound should be performed5. An advantage of zetaplasty is that the position of the labial commissure may be adjusted to be similar to that of the non-affected side, while more natural facial expression is an advantage for the simple method with linear suture.
Nevertheless, with this method, the commissure of the mouth tends to be retracted due to contracture and it is difficult to adjust the position of the commissure of the mouth. Thus, some authors recommend a small zetaplasty performed together with the nasolabial groove or multiple Zs as a miscellany that has the beneficial aspects of the two methods.
Currently, the methods with zetaplasty are widely used because better aesthetic results can be expected. However, the last two methods also have a shortcoming in that they make adjustment of the location of the commissure of the mouth in a symmetrical manner difficult. As a result, the commissure tends to be positioned inferiorly as compared with that in the unchanged side.
With respect to the bilateral clefts and with the need for bilateral commissuroplasty, the marking of a new commissure is hampered by lack of a contralateral reference. Some authors use the mid pupillary line as a reference, but we applied the equation for the total length of the lip in patient 2. It consists of x + x/2, in which x refers to the length of the nasal base12,13. With this calculation of the labial length, we can achieve an appropriate oral opening without changing the aesthetic units of the face.
CONCLUSION
The use of quadrangular mucosal flaps and skin zetaplasty allowed the goals of an optimal surgical treatment to be achieved. As proposed, a functional restoration of labial muscles was achieved, besides a symmetrical, natural, and aesthetic contour, without evidence of significant cicatricial retraction. Thus, we believe that the technique used can be a standard in the treatment of macrostomia.
COLLABORATIONS
GGAT Literature search, design of figures, analysis of results, and surgeries.
DMP Revision of the manuscript and literature search.
REFERENCES
1. McCarthy JG, Grayson BH, Coccaro PJ, Wood-Smith D. Craniofacial Microstomia. In: McCarthy JG (Ed.). Plastic Surgery. Philadelphia: Saunders; 1990. p.3054-100.
2. Melega JM, Viterbo F, Mendes FH, eds. Cirurgia Plástica - Os Princípios e a Atualidade. Rio de Janeiro: Guanabara Koogan; 2011.
3. Blackfield HM, Wilde NJ. Lateral facial clefts. Plast Reconstr Surg. 1946;6(1):68-78.
4. Grabb WC. The first and second branchial arch syndrome. Plast Reconstr Surg. 1965;36(5):485-508. PMID: 5320180 DOI: http://dx.doi.org/10.1097/00006534-196511000-00001
5. Oghale OP, Chris-Ozoko Nee Ebite LE. Asyndromic bilateral facial cleft. Ann Med Health Sci Res. 2013;3(1):122-4.
6. Mathes SJ. Pediatric Plastic Surgery. In: Mathes SJ, Hentz VR, eds. Plastic Surgery. Philadelphia: Saunders; 2006.
7. Boo-Chai K. The transverse facial cleft: its repair. Br J Plast Surg. 1969;22(2):119-24. PMID: 5785531 DOI: http://dx.doi.org/10.1016/S0007-1226(69)80052-4
8. Nagai I, Weinstein I. Surgical repair of horizontal facial cleft: Report of case. J Oral Sur Anest Hosp Dent Serv.1963;21:251-4.
9. May H. Transverse facial clefts and their repair. Plast Reconstr Surg Transplant Bull. 1962;29:240-9. PMID: 14471646 DOI: http://dx.doi.org/10.1097/00006534-196203000-00002
10. Pruzansky S. Not all dwarfed mandibles are alike. Birth Defects. 1969;5:120-9.
11. Longarcre JJ, Destefano GA, Holmstrand KE. The surgical management of first and second branchial arch syndromes. Plast Reconstr Surg. 1963;31(6):507-20. DOI: http://dx.doi.org/10.1097/00006534-196306000-00002
12. Stark RB, Saunders DE. The first branchial syndrome. The oral-mandibular-auricular syndrome. Plast Reconstr Surg. 1962;29:229-39. PMID: 13916321 DOI: http://dx.doi.org/10.1097/00006534-196203000-00001
13. Kaplan EN. Commissuroplasty and myoplasty for macrostomia. Ann Plast Surg. 1981;7(2):136-44. DOI: http://dx.doi.org/10.1097/00000637-198108000-00010
1. Hospital dos Defeitos da Face, São Paulo, SP, Brazil
2. Hospital Municipal Infantil Menino Jesus, São Paulo, SP, Brazil
3. Instituto de Cirurgia Plástica Santa Cruz, São Paulo, SP, Brazil
4. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital dos defeitos da face, São Paulo, SP, Brazil.
Corresponding author:
Guilherme Gurgel do Amaral Teles
Rua Dr. Samuel Porto, 237 Ap. 154, Saúde
São Paulo, SP, Brazil Zip Code 04054-010
E-mail: guilhermeteles77@yahoo.com.br
Article received: May 11, 2013.
Article accepted: September 1, 2013.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter