

Original Article - Year 2025 - Volume 40Issue 1
Epidemiology and Multidisciplinary Approach in Orofacial Clefts: Clinical Features and Rehabilitation Patterns
Epidemiologia e abordagem multidisciplinar nas fissuras orofaciais: Características clínicas e padrões de reabilitação
ABSTRACT
Introduction Orofacial clefts are congenital malformations that affect craniofacial development and represent a significant public health concern. The present study aimed to investigate the frequency, distribution, and characteristics of these clefts in patients treated at a specialized center, also evaluating the rehabilitation patterns employed.
Materials and Methods The research involved 59 patients diagnosed with different types of orofacial clefts, including both simple and complex cases, with or without surgical history. We analyzed variables such as sex, age group, and procedures performed. The statistical analysis was conducted using multivariate methods, including principal component analysis (PCA) and cluster analysis (CA), with the SAS (SAS Institute Inc.) software, version 9.2.
Results Cleft right (CRT) or left transforamen (CLT) were the most prevalent, particularly among male patients. Most cases involved infants and young children, reflecting the practice of early intervention. Approximately 59.3% of the patients had already undergone surgeries such as cheiloplasty and palatoplasty, often in combination. More complex cases, such as those of cleft bilateral transforaminal (CBT), required multiple surgeries and extended follow-up.
Conclusion The current study highlights the need for early and continuous interventions, as well as regional epidemiological surveys to guide public policies and optimize resource allocation. Multidisciplinary care and personalized treatment planning are essential to improving the quality of life of the patients and their families.
Keywords: cleft lip; cleft palate; craniofacial abnormalities; epidemiology; surgery, plastic
RESUMO
Introdução As fissuras orofaciais são malformações congênitas que afetam o desenvolvimento craniofacial e configuram um problema relevante de saúde pública. Este estudo buscou investigar a frequência, a distribuição e as características dessas fissuras em pacientes atendidos em um centro especializado, além de avaliar os padrões de reabilitação adotados.
Materiais e Métodos A pesquisa envolveu 59 pacientes diagnosticados com diferentes tipos de fissuras orofaciais, incluindo casos simples e complexos, com ou sem histórico cirúrgico. Foram analisadas variáveis como sexo, faixa etária e procedimentos realizados. A análise estatística foi realizada por métodos multivariados, incluindo análise de componentes principais (PCA, do inglês principal component analysis) e análise de agrupamento (CA, do inglês cluster analysis), com o programa SAS (SAS Institute Inc.), versão 9.2. Resultados As fissuras transforaminais direitas (CRT, do inglês cleft right transforamen) ou esquerdas (CLT, do inglês cleft left transforamen) foram as mais prevalentes, especialmente em pacientes do sexo masculino. A maior parte dos atendimentos foi feita em bebês e crianças pequenas, o que reflete a prática de intervenção precoce. Cerca de 59,3% dos pacientes já haviam passado por cirurgias, como queiloplastia e palatoplastia, muitas vezes em combinação. Fissuras mais complexas, como as transforaminais bilaterais (CBT, do inglês cleft bilateral transforaminal), demandaram múltiplas cirurgias e acompanhamento prolongado.
Conclusão Este estudo ressalta a necessidade de intervenções precoces e contínuas, bem como de levantamentos epidemiológicos regionais para orientar políticas públicas e otimizar a alocação de recursos. O manejo multidisciplinar e o planejamento personalizado são fundamentais para melhorar a qualidade de vida dos pacientes e de suas famílias.
Palavras-chave: anormalidades craniofaciais; cirurgia plástica; epidemiologia; fenda labial; fissura palatina
Introduction
Orofacial clefts are congenital malformations that impair craniofacial development and represent a significant public health issue in various regions worldwide. The prevalence of these conditions is estimated to be of approximately 1 in every 700 live births, underscoring their clinical and epidemiological importance.1 Between 1990 and 2019, the global incidence of these clefts declined, particularly in regions with high sociodemographic index (SDI) levels. However, some low-income countries have reported significant increases in occurrence rates.2
Orofacial clefts result from a combination of genetic and environmental factors. The genetic factors include mutations in genes that regulate facial and palate development. Additionally, exposure to certain medications and chemicals during pregnancy can interfere with fetal development, increasing the risk ofthesemalformations.3 There is also evidence that maternal nutrition plays a crucial role in the etiology of cleft lip and palate, along with epigenetic modifications that contribute to its pathogenesis.4,5
These clefts range from isolated lip clefts to complete palatal involvement, impacting facial esthetics as well as essential functions such as feeding, speech, and breathing. These impairments significantly affect the quality of life of the patients and their families.6,7
Given the complexity of these conditions, managing orofacial clefts requires a multidisciplinary approach involving surgeons, speech therapists, orthodontists, psychologists, and other healthcare professionals.8Early intervention is crucial to optimize the long-term outcomes, as procedures such as cheiloplasty and palatoplasty, performed in early childhood, minimize functional difficulties and facilitate psychosocial development.9 However, the need for multiple surgeries over time makes continuous follow-up essential to ensure effective rehabilitation.10
The epidemiology of orofacial clefts varies according to genetic, environmental, and regional factors, making it necessary to map these variables to guide more effective interventions.11 Although significant advances have been made in diagnosis and treatment, gaps remain in the literature, particularly regarding the distribution of cleft types and the impact of surgical history on outcomes across different populations.12 Such information is critical to optimize resource allocation and improve the quality of care provided by specialized centers.
Objective
The present study aims to investigate the frequency, distribution, and characteristics of orofacial clefts in patients treated at Pró-Sorriso Center for Cleft Lip and Palate Treatment, located in the city of Alfenas, state of Minas Gerais, Southeastern Brazil. Furthermore, it seeks to assess the rehabilitation patterns employed, considering variables such as sex, age, and surgical history, with the goalof contributing to the development of more effective treatment strategies and public policies focused on patient rehabilitation.
Materials and Methods
The current study included 59 patients with orofacial clefts, with or without a clinical history of orofacial surgery, treated between February 2019 and February 2020. The patients’ ages ranged from 3 months to 58 years (mean: 10.1 ± 14.6 years), encompassing both sexes (17 female subjects, with a mean age of 16.3 ± 19.3 years; and 42 male subjects, with a mean age of 7.6 ± 11.6 years). All patients were clinically indicated for surgical rehabilitation and were diagnosed according to the clinical classification of orofacial clefts.13,14 They received continuous medical and dental care at Pró- Sorriso Center.
The patient population was stratified by age group, sex, type of orofacial cleft, surgical history, and type of previous surgical rehabilitation. These variables were statistically analyzed to assess trends and associations. The present research adhered to the ethical principles outlined in Resolution no. 466/2012 of the Brazilian National Health Council and was approved by the Research Ethics Committee of Faculdade de Odontologia de Piracicaba, Universidade Estadual de Campinas (FOP/UNICAMP), under protocol No. 093/2014, CAAE 34875614.0.0000.5418.
Data were subjected to multivariate statistical analysis using the SAS (SAS Institute Inc.) software, version 9.2. The analytical methods included principal component analysis (PCA) and interactive biplot construction, along with cluster analysis (CA) and dendrogram interpretation (threshold ≤0.5) to identify patterns and relationships within the data.15
Results
The present study analyzed 59 patients diagnosed with various types of orofacial clefts, encompassing anatomical variations and associated syndromic conditions, as shown in ►Table 1 and ►Fig. 1. A clear predominance of transforamen clefts (cleft right transforamen [CRT] and cleft left transforamen [CLT]) was observed, with a higher incidence among male patients, reflecting an epidemiological profile characteristic of these malformations.
| Types of orofacial clefts | Female | Male | Σ | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| CBT | 2 | 3.4 | 7 | 11.9 | 9 | 15.3 |
| CRT or CLT | 4 | 6.8 | 18 | 30.5 | 22 | 37.3 |
| CPo-FC | 1 | 1.7 | 1 | 1.7 | 2 | 3.4 |
| CPo-FI | 2 | 3.4 | 2 | 3.4 | 4 | 6.8 |
| CP-FRC or CP-FLC | 4 | 6.8 | 1 | 1.7 | 5 | 8.5 |
| CP-FRI or CP-FLI | 1 | 1.7 | 6 | 10.2 | 7 | 11.9 |
| CSPo-FI | 1 | 1.7 | 0 | 0.0 | 1 | 1.7 |
| DG-G | 1 | 1.7 | 0 | 0.0 | 1 | 1.7 |
| CP-FRI or CP-FLI þ CPo-FI | 1 | 1.7 | 4 | 6.8 | 5 | 8.5 |
| CRT or CLT þ CP-FRI or CP-FLI | 0 | 0.0 | 3 | 5.1 | 3 | 5.1 |
| Σ | 17 | 28.8 | 42 | 71.2 | 59 | 100.0 |
Abbreviations: CBT, cleft bilateral transforaminal; CLT, cleft left transforamen; CP-FLC, cleft preforamen left complete; CP-FLI, cleft preforamen left incomplete; CP-FRC, cleft preforamen right complete; CP-FRI, cleft preforamen right incomplete; CPo-FC, cleft postforamen complete; CPo-FI, cleft postforamen incomplete; CRT, cleft right transforamen; CSPo-FI, cleft submucosa postforamen incomplete; DG-G, deformity groove-gingival.
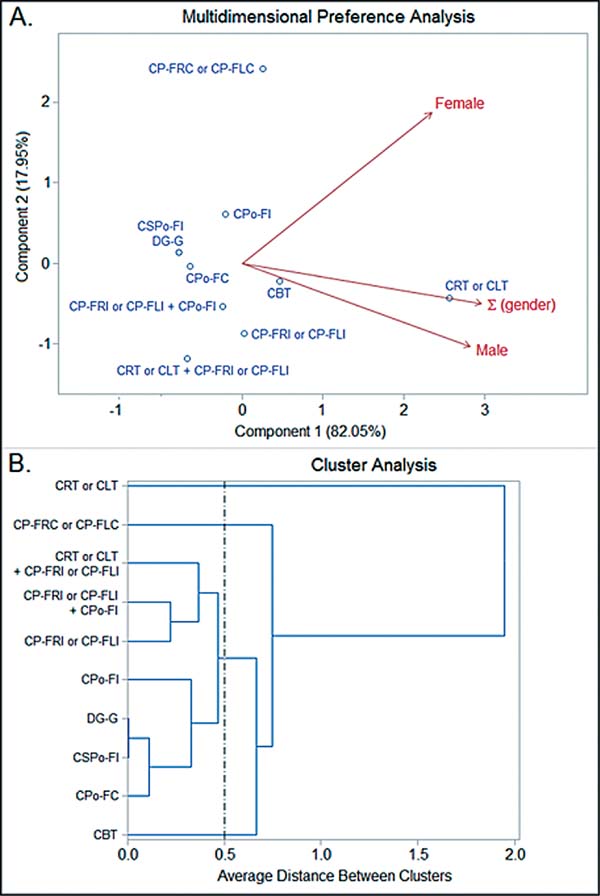
The findings revealed that males were more frequently affected by CRT and CLT. In contrast, more complex clefts, such as cleft preforamen complete (CP-FC) or cleft preforamen incomplete (CP-FI), exhibited a more balanced distribution across both sexes. This suggests potential variations in the etiological or environmental factors influencing different cleft types. The stratificationby sex and cleft type provides insights that may assist in tailoring clinical interventions according to demographic patterns.
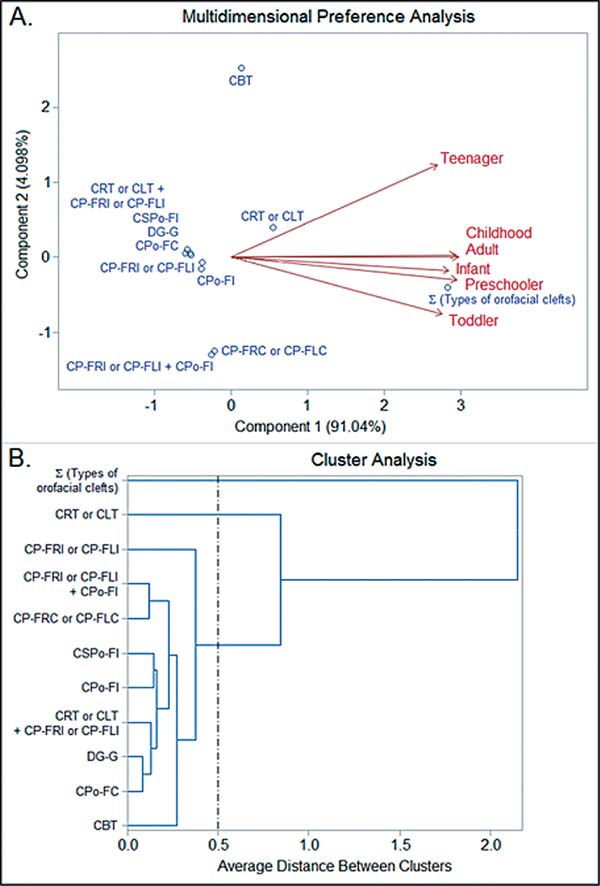
Additionally, patients with clefts associated with other malformations (such as a combination of transand preforamen clefts) exhibited a notable distribution across age groups, as shown in ►Table 2 and ►Fig. 2. The analysis of age groups revealed that infants (up to 1 year old) and toddlers (1-3 years) were most frequently hospitalized for initial surgical interventions, indicating an established practice of early intervention. These interventions aim to minimize functional and esthetic impairments, promoting social and psychosocial development.
| Types of orofacial clefts | Infant | Toddler | Preschooler | Childhood | Teenager | Adult | Σ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| CBT | 1 | 1.7 | 1 | 1.7 | 1 | 1.7 | 2 | 3.4 | 2 | 3.4 | 2 | 3.4 | 9 | 15.3 |
| CRT or CLT | 10 | 16.9 | 1 | 1.7 | 2 | 3.4 | 4 | 6.8 | 1 | 1.7 | 4 | 6.8 | 22 | 37.3 |
| CPo-FC | 1 | 1.7 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 2 | 3.4 |
| CPo-FI | 1 | 1.7 | 0 | 0.0 | 1 | 1.7 | 2 | 3.4 | 0 | 0.0 | 0 | 0.0 | 4 | 6.8 |
| CP-FRC or CP-FLC | 0 | 0.0 | 2 | 3.4 | 1 | 1.7 | 1 | 1.7 | 0 | 0.0 | 1 | 1.7 | 5 | 8.5 |
| CP-FRI or CP-FLI | 5 | 8.5 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 0 | 0.0 | 1 | 1.7 | 7 | 11.9 |
| CSPo-FI | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 |
| DG-G | 1 | 1.7 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 |
| CP-FRI or CP-FLI þ CPo-FI | 1 | 1.7 | 2 | 3.4 | 1 | 1.7 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 5 | 8.5 |
| CRT or CLT þ CP-FRI or CP-FLI | 2 | 3.4 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 0 | 0.0 | 0 | 0.0 | 3 | 5.1 |
| Σ | 22 | 37.3 | 6 | 10.2 | 6 | 10.2 | 12 | 20.3 | 3 | 5.1 | 10 | 16.9 | 59 | 100.0 |
Abbreviations: CBT, cleft bilateral transforaminal; CLT, cleft left transforamen; CP-FLC, cleft preforamen left complete; CP-FLI, cleft preforamen left incomplete; CP-FRC, cleft preforamen right complete; CP-FRI, cleft preforamen right incomplete; CPo-FC, cleft postforamen complete; CPo-FI, cleft postforamen incomplete; CRT, cleft right transforamen; CSPo-FI, cleft submucosa postforamen incomplete; DG-G, deformity groove-gingival.
Notes: Infant (from birth to 1 year of age); toddler (1-3 years of age); preschooler (3-5 years of age); childhood (6-11 years of age); teenager (12-17 years of age); and adult (older than 18 years).
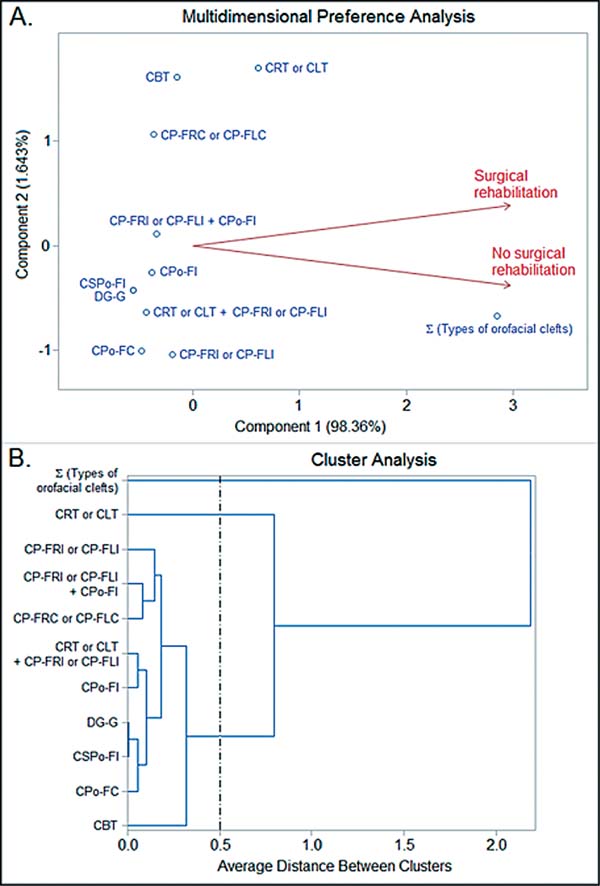
Approximately59.3%ofthepatients,asshown in ►Table 3 and ►Fig. 3, had undergone at least 1 surgical intervention. The most common procedures included cheiloplasty, palatoplasty, and combined surgeries, such as cheiloplasty with palatoplasty. More complex cases, such as those of cleft bilateral transforaminal (CBT), required multiple surgeries over time, underscoring the importance of long-term planning and continuous follow-up to ensure effective rehabilitation.
| Types of orofacial clefts | Surgical rehabilitation | No surgical rehabilitation | Σ | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| CBT | 7 | 11.9 | 2 | 3.4 | 9 | 15.3 |
| CRT or CLT | 15 | 25.4 | 7 | 11.9 | 22 | 37.3 |
| CPo-FC | 0 | 0.0 | 2 | 3.4 | 2 | 3.4 |
| CPo-FI | 2 | 3.4 | 2 | 3.4 | 4 | 6.8 |
| CP-FRC or CP-FLC | 4 | 6.8 | 1 | 1.7 | 5 | 8.5 |
| CP-FRI or CP-FLI | 3 | 5.1 | 4 | 6.8 | 7 | 11.9 |
| CSPo-FI | 0 | 0.0 | 1 | 1.7 | 1 | 1.7 |
| DG-G | 0 | 0.0 | 1 | 1.7 | 1 | 1.7 |
| CP-FRI or CP-FLI þ CPo-FI | 3 | 5.1 | 2 | 3.4 | 5 | 8.5 |
| CRT or CLT þ CP-FRI or CP-FLI | 1 | 1.7 | 2 | 3.4 | 3 | 5.1 |
| Σ | 35 | 59.3 | 24 | 40.7 | 59 | 100.0 |
Abbreviations: CBT, cleft bilateral transforaminal; CLT, cleft left transforamen; CP-FLC, cleft preforamen left complete; CP-FLI, cleft preforamen left incomplete; CP-FRC, cleft preforamen right complete; CP-FRI, cleft preforamen right incomplete; CPo-FC, cleft postforamen complete; CPo-FI, cleft postforamen incomplete; CRT, cleft right transforamen; CSPo-FI, cleft submucosa postforamen incomplete; DG-G, deformity groove-gingival.
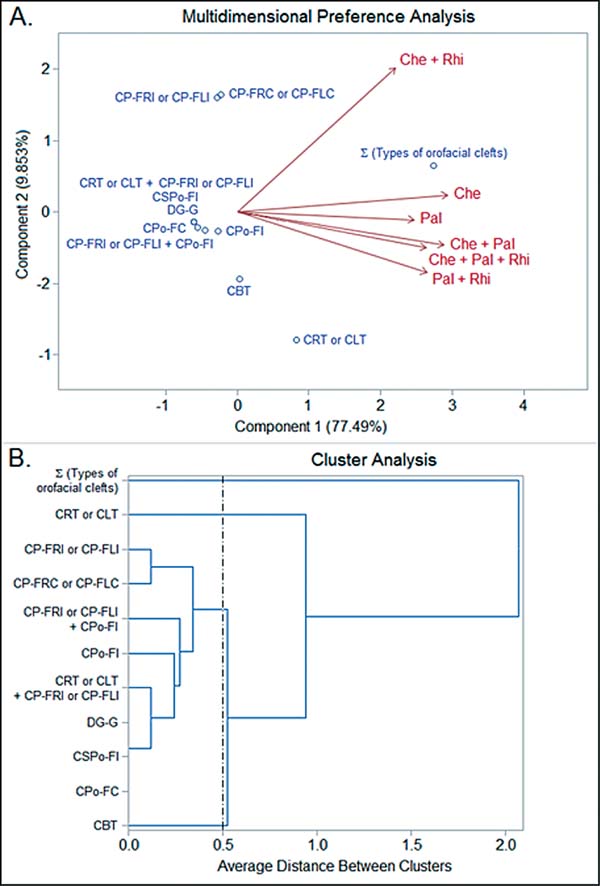
The multivariate analysis, performed using the SAS software, version 9.2, enabled the construction of biplots and dendrograms to interpret clustering patterns and similarities between cleft types and their epidemiological characteristics. ►Table 4 and ►Fig. 4 highlight the relationship between cleft types and the surgical interventions performed. We observed that patients with simpler clefts, such as CRT or CLT, often underwent isolated cheiloplasty or a combination of cheiloplasty and palatoplasty. In contrast, more complex cases, such as those of clefts associated with other malformations, required additional procedures, including rhinoseptoplasty.
| Types of orofacial clefts | Surgical rehabilitation | No surgical rehabilitation | Σ | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Che | Pal | Rhi | Che þ Pal | Che þ Rhi |
Pal þ Rhi |
Che þ Pal þ Rhi | Σ | |||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| CBT | 1 | 1.7 | 0 | 0.0 | 0 | 0.0 | 4 | 6.8 | 0 | 0.0 | 0 | 0.0 | 2 | 3.4 | 7 | 11.9 | 2 | 3.4 | 9 | 15.3 |
| CRT or CLT | 7 | 11.9 | 1 | 1.7 | 0 | 0.0 | 5 | 8.5 | 0 | 0.0 | 1 | 1.7 | 1 | 1.7 | 15 | 25.4 | 7 | 11.9 | 22 | 37.3 |
| CPo-FC | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 3.4 | 2 | 3.4 |
| CPo-FI | 0 | 0.0 | 2 | 3.4 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 3.4 | 2 | 3.4 | 4 | 6.8 |
| CP-FRC or CP-FLC | 3 | 5.1 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 0 | 0.0 | 0 | 0.0 | 4 | 6.8 | 1 | 1.7 | 5 | 8.5 |
| CP-FRI or CP-FLI | 2 | 3.4 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 0 | 0.0 | 0 | 0.0 | 3 | 5.1 | 4 | 6.8 | 7 | 11.9 |
| CSPo-FI | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 1 | 1.7 |
| DG-G | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 1 | 1.7 |
| CP-FRI or CP-FLI þ CPo-FI |
1 | 1.7 | 0 | 0.0 | 0 | 0.0 | 2 | 3.4 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 3 | 5.1 | 2 | 3.4 | 5 | 8.5 |
| CRTor CLT þ CP-FRI or CP-FLI | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.7 | 2 | 3.4 | 3 | 5.1 |
| Σ | 14 | 23.7 | 3 | 5.1 | 0 | 0.0 | 12 | 20.3 | 2 | 3.4 | 1 | 1.7 | 3 | 5.1 | 35 | 59.3 | 24 | 40.7 | 59 | 100.0 |
Abbreviations: CBT, cleft bilateral transforaminal; Che, cheiloplasty; CLT, cleft left transforamen; CP-FLC, cleft preforamen left complete; CP-FLI, cleft preforamen left incomplete; CP-FRC, cleft preforamen right complete; CP-FRI, cleft preforamen right incomplete; CPo-FC, cleft postforamen complete; CPo-FI, cleft postforamen incomplete; CRT, cleft right transforamen; CSPo-FI, cleft submucosa postforamen incomplete; DG-G, deformity groove-gingival; Pal, palatoplasty; Rhi, rhinoseptoplasty.
Discussion
The predominance of CLT over CRT is a striking trend in the epidemiology of lip and palate clefts, particularly among male patients. Studies16 indicate that males are significantly more affected by these clefts, with a male-to-female ratio of 1.34:1. In a cohort from West Bengal,16 69.59% of the patients were male, reinforcing this sex disparity.
The left side of the face is more frequently affected, with left unilateral clefts being the most common, as observed in several studies.17,18 In Brazil, Rollemberg et al.19 (2019) found that 20.5% of patients presented with CLT, supporting this trend.
The high frequency of CRT and CLT highlights the importance of early surgical interventions to ensure proper orofacial function, such as feeding and speech.18 More complex clefts, such as CBT and cleft postforamen incomplete (CPoFI), exhibit a more balanced sex distribution, contrasting with the male predominance in other types.20 These complex clefts require more elaborate surgical approaches and long-term multidisciplinary planning.21
The success of interventions also depends on continuous follow-up, as multiple surgeries may be necessary throughout the patient’s life.10 In this context, advanced diagnostic tools can enhance early detection and management, positively impacting therapeutic outcomes.22 Additionally, it is crucial to consider the psychological and socioeconomic impacts on both patients and their families.4
In the current study, 59.3% of patients had undergone some form of surgical intervention, with cheiloplasty and palatoplasty being the most frequent. Cheiloplasty, performed between 3 and 6 months of age, aims to restore lip structure and function by aligning its components and reestablishing muscular continuity.23,24 Palatoplasty, typically performed around 10 months of age, seeks to restore palatal integrity using techniques such as intravelar veloplasty and vomer flap closure.23,25 These procedures are fundamental in restoring both functionality and esthetics, promoting psychosocial development.6
Beyond improving facial appearance, these surgeries enhance speech and feeding capabilities, which are essential for social integration and quality of life.14,26 Studies27 suggest that the timing and techniques of interventions can significantly impact long-term outcomes.
Personalizing treatment plans is essential, particularly in more complex cases, such as CRT or CLT combined with other anomalies. A quantified classification of clefts assists in planning individualized strategies, ensuring greater treatment efficacy.28 Patients with seemingly similar conditions may respond differently to interventions, underscoring the need for personalized approaches.29
A study30 involving 2,475 patients found that comorbidities often require more comprehensive rehabilitation, highlighting the need for continuous specialized care. Multidisciplinary management is essential to achieve satisfactory outcomes, as the lack of integrationamongspecialtiescan compromise treatment effectiveness.10 While individualized treatment is a priority, it is also important to address the risk of patient fatigue, which may affect adherence and long-term therapeutic success.
The multidisciplinary approach, often emphasized in the literature,31 is indispensable for effective rehabilitation. Collaboration among speech therapists, psychologists, and orthodontists is crucial to ensure that functional, emotional, and social aspects are comprehensively addressed.9 This holistic approach is essential to promote psychosocial development and enhance patient quality of life.32
Finally, the current study highlights the importance of regional epidemiological surveys as a basis for the development of more effective public policies. Analyzing the distribution of cleft types and the impact of surgical interventions provides valuable insights to optimize the services offered by specialized centers.33These data are essential to efficiently allocate resources and develop prevention and treatment strategies aligned with the needs of the patients.
Conclusion
The present study identified the predominance of CRT and CLT, particularly among male patients, highlighting the need for early interventions and continuous follow-up, especially in more complex cases. We observed that 59.3% of the patients had already undergone surgical procedures, such as cheiloplasty and palatoplasty, indicating that many of them begin rehabilitation during the first months of life. These findings reinforce the importance of a multidisciplinary approach, which is essential to address functional and psychosocial aspects in an integrated manner, thereby promoting comprehensive recovery.
The results underscore the significance of regional epidemiological surveys to guide public policies and optimize specialized care, ultimately improving the quality of life of the patients and their families.
References
1. Kantar RS, Hamdan US, Muller JN, Hemal K, Younan RA, Haddad M, et al. Global prevalence and burden of orofacial clefts: A systematic analysis for the Global Burden of Disease Study 2019. J Craniofac Surg 2023;34(07):2012-2015. Doi: 10.1097/ SCS.0000000000009591
2. Wang D, Zhang B, Zhang Q, Wu Y. Global, regional and national burden of orofacial clefts from 1990 to 2019: an analysis of the Global Burden of Disease Study 2019. Ann Med 2023;55(01): 2215540. Doi: 10.1080/07853890.2023.2215540
3. Garland MA, Reynolds K, Zhang S, Sun B, De Frates R, Zhou CJ. Fundamental mechanisms of orofacial clefts. In: Meyer U. Fundamentals of Craniofacial Malformations. Vol. 1; Disease and Diagnostics Cham: Springer International Publishing; 2021: 99-142
4. Nasreddine G, El Hajj J, Ghassibe-Sabbagh M. Orofacial clefts embryology, classification, epidemiology, and genetics. Mutat Res Rev Mutat Res 2021;787:108373. Doi: 10.1016/j.mrrev.2021. 108373
5. Watanabe M, Zhou CJ. Introduction to the special issue on orofacial clefts. Birth Defects Res 2020;112(19):1555-1557. Doi: 10.1002/bdr2.1833
6. Yohana N, Handoko H. Understanding of speech production in cleft lip/palate: A review. Jurnal Arbitrer 2023;10(04):437-446. Doi: 10.25077/ar.10.4.437-446.2023
7. Babai A, Irving M. Orofacial clefts: Genetics of cleft lip and palate. Genes (Basel) 2023;14(08):1603. Doi: 10.3390/genes 14081603
8. Castilho JF, Ribeiro IC, Andrade ALCA, Oliveira DD, Lima IL. Multidisciplinary treatment in a patient with Bilateral cleft lip and palate: A case report. Iran J Orthod 2024;19(02):1-12. Doi: 10.32592/ijorth.19.2.1148
9. Arcila LVC, Gomes LCL, Travassos A, Fernandes VVB, Nascimento RD, Ursi W. Multidisciplinary action in a patient with cleft lip and palate: Esthetic-functional dentofacial treatment for more than two decades. Braz Dent Sci 2023;26(02):e3801. Doi: 10.4322/ bds.2023.e3801
10. Kaiser JK, Kamble RH, Nambiar K, Nerurkar S, Suchak D. Comprehensive multidisciplinary management of bilateral cleft lip and palate. Cureus 2024;16(01):e52643. Doi: 10.7759/cureus.52643
11. Oliveira ACBd, Silva AMd, Amorim M, Pires ALPV, Lisboa LdJ, Calumby RT, Freitas VS. Epidemiological profile and prevalence of live-borns with orofacial fissures in Brazil between 1999 and 2017. Oral Surg Oral Med Oral Pathol Oral Radiol 2022;134(03): e210. Doi: 10.1016/j.oooo.2022.01.654
12. Alcon A, Verzella A, Brydges H, Laspro M, Cassidy M, Chaya B, et al. The impact of geographic and socio-demographic factors on the incidence of orofacial clefts in the United States. Plast Reconstr Surg Glob Open 2023;11(10 Suppl):59-60. Doi: 10.1097/01. GOX.0000992176.49718.6a
13. Rodrigues R, Fernandes MH, Monteiro AB, Furfuro R, Sequeira T, Silva CC, Manso MC. SPINA classification of cleft lip and palate: A suggestion for a complement. Arch Pediatr 2018;25(07):439-441. Doi: 10.1016/j.arcped.2018.08.001
14. Worley ML, Patel KG, Kilpatrick LA. Cleft lip and palate. Clin Perinatol2018;45(04):661-678.Doi:10.1016/j.clp.2018.07. 006
15. Boriollo MFG, Oliveira MC, Bassinello V, Aníbal PC, Silva TAd, Silva JJd, et al. Candida species biotypes and polyclonality of potentially virulent Candida albicans isolated from oral cavity of patients with orofacial clefts. Clin Oral Investig 2022;26(03):3061-3084. Doi: 10.1007/s00784-021-04290-z
16. Saha N, Das M, Zahir S, Santra A. A retrospective study on clinical and epidemiological profile of nonsyndromic cleft lip and palate patients admitted in a large comprehensive cleft care centre in West Bengal, India. J Cleft Lip Palate Craniofacial Anomalies 2023; 10(01):9-13. Doi: 10.4103/jclpca.jclpca_19_22
17. Ashwinirani SR, Suragimath G. Association of cleft lip and palate with predisposing factors. BLDE Univ J Health Sci. 2022;7(01): 110-114. Doi: 10.4103/bjhs.bjhs_122_21
18. Vendramin AV, Steinkirch CLV, Czarnobay GT, Rebello MGRM, Ton WS, Gamborgi MA, Nisihara R. Epidemiological profile of children and adolescents with oral cleft treated at a referral center in Curitiba, PR, Brazil. Rev Bras Cir Plást 2017;32(03):321-327. Doi: 10.5935/2177-1235.2017RBCP0054
19. Rollemberg EV, Pires TO, Moraes GN, Rios LR, Machado LG, Da- Silva MD, Parreira DR. Epidemiological profile of patients with cleft lip and palate in a reference service in the Federal District. Rev Bras Cir Plást 2019;34:94-100. Doi: 10.5935/2177-1235.2019RBCP0014
20. Chauhan JS, Sharma S. Morphological presentation of orofacial clefts: An epidemiological study of 5004 patients in a tertiary care hospital of Central India. Cleft Palate Craniofac J 2023;60(02): 219-224. Doi: 10.1177/10556656211057739
21. Gustafsson C, Heliövaara A, Rautio J, Leikola J. Long-term followup of bilateral cleft lip and palate: Incidence of speech-correcting surgeries and fistula formation. Cleft Palate Craniofac J 2023;60 (10):1241-1249. Doi: 10.1177/10556656221102816
22. Baeza-Pagador A, Tejero-Martínez A, Salom-Alonso L, Camañes- Gonzalvo S, García-Sanz V, Paredes-Gallardo V. Diagnostic methods for the prenatal detection of cleft lip and palate: A systematic review. J Clin Med 2024;13(07):2090. Doi: 10.3390/ jcm13072090
23. Dhooghe N, Verhelst P, Vandenbosch K, Engelen B, Vanderhaeghe F, Nagy K, et al. Chirurgische behandeling lip-en verhemeltespleet. Tijdschrift voor Geneeskunde en Gezondheidszorg 2023;79(06): 493-502. Doi: 10.47671/TVG.79.23.045
24. Fell M, Davies A, Davies A, Chummun S, Cobb ARM, Moar K, Wren Y. Current surgical practice for children born with a cleft lip and/or palate in the United Kingdom. Cleft Palate Craniofac J 2023;60 (06):679-688. Doi: 10.1177/10556656221078151
25. Ardouin K, Davis N, Stock NM. Expanding support services for adults born with cleft lip and/or palate in the United Kingdom: An exploratory evaluation of the Cleft Lip and Palate Association Adult Services Programme. Cleft Palate Craniofac J 2022;59 (4_suppl2, suppl2)S48-S56. Doi: 10.1177/10556656211025415
26. Umedjonovich LJ, Dastamovich ID. The use of modern orthodontic and surgical technologies in the comprehensive rehabilitation of children with congenital cleft of the upper lip, alveolar process, and palate. Eur Int J Multidiscip Res Manag Stud. 2024;4(04): 21-26. Doi: 10.55640/eijmrms-04-04-04
27. Tiaraningrum RRK, Dharmawan MS, Yatindra IACD, Rooseno RRN. The effects of early and delayed palatal repair on maxillary growth and speech outcome in unilateral cleft lip and palate patients: A systematic review. J Anestesi 2024;2(03):146-155. Doi: 10.59680/anestesi.v2i3.1211
28. Gutierrez-Sanchez B, Maya-Behar J, Cerda RM, Ortiz-Posadas MR. A surgical complexity factor for clefts of primary and secondary palates. Annu Int Conf IEEE Eng Med Biol Soc 2023;2023:1-4. Doi: 10.1109/EMBC40787.2023.10340486
29. Van der Horst C. Personalized health care for orofacial cleft patients. In: Nico Van Weert N, Hazelzet J, editors. Personalized Specialty Care: Value-Based Healthcare Frontrunners from the Netherlands. 1st ed. Cham: Springer International Publishing; 2021:41-47
30. Rogozhina YS, Blokhina SI, Bimbas ES. On the issue of surgical treatment of patients with congenital orofacial clefts combined with other organ and system comorbidities. Pediatr Dent Dent Prophylaxis 2023;23(03):281-294. Doi: 10.33925/1683-3031-2023-658
31. Matos JDMd, Nakano LJN, Rodrigues AG, Pinto AD, Grande MFB, Lopes GdRS, Andrade VC. Orofacial clefts: Treatment based on a multidisciplinary approach. Arch Health Invest. 2020;9(05): 468-473. Doi: 10.21270/archi.v9i5.4804
32. Bous RM, Kumar A, Valiathan M. Multidisciplinary rehabilitation of an adult with a cleft lip and palate: An illustration of a dental substitution approach for the management of unilateral agenesis of central and lateral incisors. FACE 2021;2(01):30-38. Doi: 10.1177/2732501621992440
33. Parham MJ, Simpson AE, Moreno TA, Maricevich RS. Updates in cleft care. Semin Plast Surg 2023;37(04):240-252. Doi: 10.1055/ s-0043-1776733
1. Department of Health II, Course of Medicine, Universidade Estadual do Sudoeste
da Bahia, Jequié, BA, Brazil
2. Department of Health Sciences, Course of Medicine, Universidade Estadual do Sudoeste
da Bahia, Vitória da Conquista, BA, Brazil
3. Department of Oral Diagnosis, Faculdade de Odontologia de Piracicaba, Universidade
Estadual de Campinas (FOP/UNICAMP), Piracicaba, SP, Brazil
4. Department of Morphology and Pathology, Centro de Ciências Biológicas e da Saúde
(CCBS), Universidade Federal de São Carlos (UFSCar), São Carlos, SP, Brazil
5. Biotechnology Postgraduate Program (PPGBiotec), Centro de Ciências Biológicas e
da Saúde (CCBS), Universidade Federal de São Carlos (UFSCar), São Carlos, SP, Brazil
6. Department of Health I, Course of Dentistry, Universidade Estadual do Sudoeste
da Bahia, Jequié, BA, Brazil
7. Postgraduate Program in Nursing and Health, Universidade Estadual do Sudoeste da
Bahia, Jequié, BA, Brazil
Address for correspondence Mateus Cardoso Oliveira, PhD, Postgraduate Program in Nursing and Health, Universidade Estadual do Sudoeste da Bahia, Jequié, BA, Brazil (e-mail: mateus_oc1@hotmail.com).
Artigo submetido: 13/10/2024.
Artigo aceito: 20/05/2025.
Conflict of Interests
The authors have no conflict of interests to declare.










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter