

Case Report - Year 2025 - Volume 40Issue 1
Breast Tuberculosis in a Patient with a History of Breast Cancer: A Case Report
Tuberculose mamária em paciente com histórico de câncer de mama: Um relato de caso
ABSTRACT
We herein report to the case of a 35-year-old female patient with a history of cancer in the right breast, who presented with breast tuberculosis after a left breast mammoplasty using a submuscular prosthesis. In addition to the standard treatment for tuberculosis, the patient underwent hyperbaric therapy, vacuum-assisted closure therapy, and laser therapy for lesion healing. Breast tuberculosis is a rare disease, and its diagnosis can be complex due to its clinical and radiological similarities to other conditions, such as breast carcinoma. However, especially in the presence of risk factors and in countries with a higher tuberculosis incidence, it is critical to consider this diagnosis.
Keywords: breast; infection; tuberculosis; wound
RESUMO
Relatamos o caso de uma paciente, de 35 anos com antecedente de câncer na mama direita, que apresentou tuberculose mamária após mamoplastia à esquerda com prótese submuscular. Além do tratamento padrão para a tuberculose, a paciente fez uso de terapia hiperbárica, terapia por pressão subatmosférica e laserterapia, técnicas que podem auxiliar na cicatrização das lesões. A tuberculose nas mamas é doença rara e diagnosticá-la pode ser difícil, devido às suas semelhanças clínicas e radiológicas com outras patologias, como o carcinoma de mama. No entanto, sobretudo na presença de fatores de risco, e em países com maior incidência da doença, seu diagnóstico não deve ser descartado.
Palavras-chave: ferida; infecção; mama; tuberculose
Introduction
Tuberculosis is a bacterial infection caused by Mycobacterium tuberculosis. The bacteria spread through the air by coughing, sneezing, or saliva of infected people and inhaled by others.Itis estimated that a quarter oftheglobal population has been infected with the bacteria.1 However, most people do not develop the disease and, as a result, do not transmit it. The risk of becoming ill is higher in immunocompromised patients, diabetics, malnourished subjects, smokers, and HIV-positive patients, reaching 5 to 10% of the general population throughout a lifetime.1
The disease mainly affects the lungs, and its classic symptoms include persistent dry or productive cough, evening fever, night sweats, and weight loss.2 Tuberculosis can also present in an extrapulmonary form, such as pleural, peripheral lymph node, meningoencephalic, pericardial, and bone tuberculosis. The most common diagnostic methods for tuberculosis are clinical, bacteriological, imaging, and histopathological techniques.2
Despite the advances in diagnosis and treatment, tuberculosis still infects more than 10 million people each year, accounting for the death of 1.25 million people worldwide.3 Almost 90% of the cases affect adults, and the mortality rate without treatment reaches 50%.3 Tuberculosis is the main cause of death among HIV-positive subjects, and it plays a relevant role in the development of antimicrobial resistance.3
In Brazil, tuberculosis remains a major public health challenge, and the fight against it suffered a significant blow from the health crisis resulting from the coronavirus disease 2019 (COVID-19) pandemic, which reduced access to its diagnosis and treatment. According to the Brazilian Ministry of Health, pandemic-related interruptions led to a 12.1% drop in the number of people diagnosed with tuberculosis from 2019 to 2020, with a partial recovery in 2021 and 2022, but still without reaching prepandemic levels.4 In 2022, the incidence of the disease was of 36.3 cases per 100 thousand inhabitants (78,057 cases). The mortality rate, which had been slowly decreasing over the last 2 decades, increased in 2021 to 5,072 deaths and a rate of 2.38 deaths per 100 thousand inhabitants,4 representing an 11.9% increase in the total number of deaths from tuberculosis.
Notably, in 2022, Rio de Janeiro was the Brazilian state with the highest risk of death from tuberculosis (5.0 deaths per 100 thousand inhabitants).4 It is also the third state with the highest incidence rate, of 68.6 cases per 100 thousand inhabitants, 1.88 times higher than the national rate.
Objective
The present study aims to report a case of breast tuberculosis in a patient with a history of breast cancer.
Materials and Methods
The current observational descriptive study refers to a 35- year-old woman with a history of breast cancer who received a diagnosis of breast tuberculosis based on the analysis of medical and photographic records from August 2017 to March 2024 at Hospital e Maternidade Santa Lúcia, in Rio de Janeiro. The study was submitted to Plataforma Brasil and approved by the Ethics in Research Committee under opinion number 7.423.804 (CAAE: 85224924.2.0000.0227).
Case Report
A 35-year-old woman was diagnosed with multicentric, triple-negative (without estrogen, progesterone, and human epidermal growth factor receptor type 2 [HER2] receptors) medullary carcinoma in her right breast in 2017. She underwent mastectomy in August 2017, followed by adjuvant treatment with 16 chemotherapy sessions, including 4 sessions with cyclophosphamide and paclitaxel and 12 sessions with doxorubicin from October 2017 to April 2018, as well as 26 radiation therapy sessions in August 2018.
Breast reconstruction was performed in two stages. The first surgery, in April 2019, consisted of a latissimus dorsi muscle flap and silicone implant on the right breast and left mastopexy without prosthesis. The patient developed a suture dehiscence at the mastopexy site and underwent a new suture in the surgical block on the 36th postoperative day.
The second reconstruction surgery, in March 2020, involved left mastopexy and prosthesis placement. Once again, the patient presented a suture dehiscence, which was treated conservatively due to the COVID-19 pandemic. In June of the same year, the patient presented erythema in the left breast. A mastology team performed a surgical biopsy, and the patient received a prescription of amoxicillin and clavulanate potassium (sold in Brazil under the brand name Clavulin BD [GlaxoSmithKline]). The biopsy revealed a mild superficial perivascular lymphocytic infiltrate.
Subsequently, in 2021, we identified the displacement of the submuscular prosthesis to the lateral region of the left breast and decided to perform a new surgical approach for prosthesis replacement.
On February 8, 2023, the patient underwent a left mammoplasty with a submuscular prosthesis in a private hospital in Rio de Janeiro. ►Fig. 1 shows the appearance of the surgical wound at the first dressing change, on February 23, 2023, 15 days after the procedure.
The following day, on February 24, 2023, the patient was readmitted to Hospital e Maternidade Santa Lúcia for wound suture and culture. The patient received a new prescription of amoxicillin and clavulanate potassium (Clavulin BD, 875 mg). Next, we referred the patient for 13 sessions of hyperbaric therapy in the city of Niterói, state of Rio de Janeiro, from February 27 to March 13, 2023. ►Fig. 2 depicts the evolution of the wound.
The culture requested on February 24, 2023, was positive for Pseudomonas aeruginosa, an opportunistic gram-negative bacterium. The patient received a prescription of ciprofloxacin 500 mg every 8 hours for 10 days.
On March 13, 2023, we terminated the hyperbaric therapy and readmitted the patient to a private hospital for vacuumassisted closure (VAC) therapy. ►Fig. 3 shows the wound on this date.
The VAC therapy was performed from March 16 to March 21, 2023. ►Fig. 4 depicts the evolution of the lesion. On March 20, 2023, we received a new report for the culture requested on February 24, 2023, this time indicating the presence of M. tuberculosis. This report established the diagnosis of cutaneous tuberculosis in the left breast, and we referred the patient for treatment at the Municipal Tuberculosis Program of the city of Itaboraí, state of Rio de Janeiro. The first stage of the treatment, with rifampicin, isoniazid, pyrazinamide, and ethambutol, was performed for an extended period of 3 months, instead of the standard 2 months, from March 20 to June 20, 2023. Next, treatment with rifampicin and isoniazid continued for another 6 months. The patient presented hyperuricemia and gout as side effects and was treated with allopurinol 300 mg.
Monitoring of the healing of the left breast lesion was performed in the outpatient clinic at Amil Espaço Saúde, in Niterói. ►Fig. 5 shows the wound dressing. The wound treatment consisted of Aquacel (Convatec), a hydrofiber dressing, Biatain Ag (Coloplast), a silver foam dressing, and Pielsana (BDS), a medication containing essential fatty acids, vitamins A and E, and copaiba and tea tree oils.
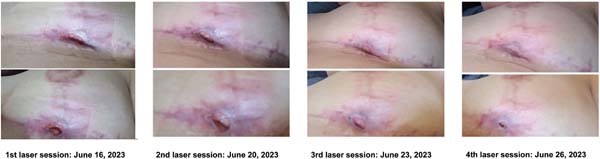
Lastly, the patient underwent 4 laser therapy sessions from June 15 to June 26, 2023, monitored by a stoma care nurse. ►Fig. 6 reveals that the lesion improved during the sessions.
The patient returned 3 months after completing the tuberculosis treatment, presenting good breast healing and the absence of inflammatory signs (►Fig. 7).
Discussion
Breast tuberculosis is a rare extrapulmonary form of the disease. In developed countries, its incidence among breast lesions is of 0.1%, reaching 3 or 4% in regions with a higher incidence of tuberculosis, such as India and African countries.5
The disease mainly affects young women of reproductive age, especially lactating and multiparous women, being rarer in prepubescent girls, postmenopausal women, and men.6 The patient’s general status is good, and most subjects do not present the classic constitutional tuberculosis symptoms, such as fever, weight loss, and night sweats.7
The signs and symptoms may include nodules, ulcers, multiple fistulas with secretion, and recurrent abscesses in the breasts. The nodules are often irregular, poorly-defined, and more commonly painful than those found in carcinoma.8 Skin and nipple retractions, inflammatory features, and axillary lymphadenopathy may occur, while multiple lesions and bilateral involvement are less common.6
Its main presentations are nodular, disseminated, and sclerosing. The nodular variant can be confused with carcinoma or fibroadenoma, while the disseminated form often leads to the formation of fistulas.5 The sclerosing form affects older women, presenting with slower growth and more extensive fibrotic processes.5
The main pillars of diagnosis are clinical examination, radiological evaluations, and histopathological studies.
However, given its rarity and nonspecific clinical and radiological findings, the diagnosis of breast tuberculosis is often complex, as the condition can be easily confused with abscesses or breast tumors, usually requiring a biopsy to exclude the latter differential diagnosis.9
It is critical to consider breast tuberculosis in all patients with abscesses or atypical masses in the breasts, especially when risk factors, such as the female gender, reproductive age, multiparity, and coinfection with HIV are present,10 particularly in regions with a higher incidence of the disease. In addition to the standard treatment with rifampicin, isoniazid, pyrazinamide, and ethambutol for 2 months, followed by rifampicin and isoniazid for 4 months, adjuvant techniques can help in the healing of any wounds, such as hyperbaric therapy, VAC therapy, and laser therapy, which the patient herein reported received. Hyperbaric therapy can help in ulcer healing,11,12 and laser therapy can reduce the size of ulcerated lesions13 and improve wound healing.14 The VAC therapy may be associated with outcomes such as lower rates of mortality,15 recurrence, and treatment failure, shorter length of hospital stay and intensive care unit (UI) stay, and lower treatment cost.16
Conclusion
Diagnosing breast tuberculosis can be a challenge for the healthcare team given the frequent presentation of nonspecific signs and symptoms, which can be confused with other diseases. However, tuberculosis incidence should not be ignored, especially in countries with high rates, such as Brazil, as early identification is essential for the correct management.
References
1. World Health Organization (WHO). WHO consolidated guidelines on tuberculosis Module 1: Prevention - Tuberculosis preventive treatment. 2nd ed. Geneva: World Health Organization; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK607290/
2. Ministério da Saúde. Manual de recomendações para o controle da tuberculose no Brasil. 2nd ed. Brasília: Ministério da Saúde; 2019. Available from: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/svsa/tuberculose/manual-de-recomendacoese-controle-da-tuberculose-no-brasil-2a-ed.pdf/view
3. World Health Organization (WHO). Global Tuberculosis Report 2024. Geneva: World Health Organization; 2024. Available from: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2024
4. Ministério da Saúde. Secretaria de Vigilância em Saúde e Ambiente. Boletim epidemiológico de tuberculose. Brasília: Ministério da Saúde; 2023 Boletim Especial. Available from: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/boletins/epidemiologicos/especiais/2023/boletim-epidemiologico-de-tuberculose-numero-especial-mar.2023/view
5. Shrestha A, Gautam K, Pyakurel D, Pradhan S, Pant V. Breast tuberculosis, a rare entity. IDCases 2019;15:e00530. Doi: 10.1016/j.idcr.2019.e00530
6. Baykan AH, Sayiner HS, Inan I, Aydin E, Erturk SM. Primary breast tuberculosis: imaging findings of a rare disease. Insights Imaging 2021;12(01):19. Doi: 10.1186/s13244-021-00961-3
7. Ghalleb M, Seghaier S, Adouni O, Bouaziz H, Bouida A, Hassouna JB, et al. Breast tuberculosis: a case series. J Med Case Rep 2021;15 (01):73. Doi: 10.1186/s13256-020-02646-9
8. Sen M, Gorpelioglu C, Bozer M. Isolated primary breast tuberculosis: report of three cases and review of the literature. Clinics (Sao Paulo) 2009;64(06):607-610. Doi: 10.1590/s1807-59322009000600019
9. Bouti K, Soualhi M, Marc K, Zahraoui R, Benamor J, Bourkadi JE, Iraqi G. Postmenopausal breast tuberculosis - report of 4 cases. Breast Care (Basel) 2012;7(05):411-413. Doi: 10.1159/000343613
10. Longman CF, Campion T, Butler B, Suaris TD, Khanam A, Kunst H, et al. Imaging features and diagnosis of tuberculosis of the breast. Clin Radiol 2017;72(03):217-222. Doi: 10.1016/j.crad.2016.11.023
11. Golledge J, Singh TP. Systematic review and meta-analysis of clinical trials examining the effect of hyperbaric oxygen therapy in people with diabetes-related lower limb ulcers. Diabet Med 2019;36(07):813-826. Doi: 10.1111/dme.13975
12. Zhang Z, Zhang W, Xu Y, Liu D. Efficacy of hyperbaric oxygen therapy for diabetic foot ulcers: An updated systematic review and meta-analysis. Asian J Surg 2022;45(01):68-78. Doi: 10.1016/j.asjsur.2021.07.047
13. Santos CMD, Rocha RBD, Hazime FA, Cardoso VS. A Systematic Review and Meta-Analysis of the Effects of Low-Level Laser Therapy in the Treatment of Diabetic Foot Ulcers. Int J Low Extrem Wounds 2021;20(03):198-207. Doi: 10.1177/1534734620914439
14. Huang J, Chen J, Xiong S, Huang J, Liu Z. The effect of low-level laser therapy on diabetic foot ulcers: A meta-analysis of randomised controlled trials. Int Wound J 2021;18(06):763-776. Doi: 10.1111/iwj.13577
15. Zhang R, Zhang Y, Hou L, Yan C. Vacuum-assisted closure versus conventional dressing in necrotizing fasciitis: a systematic review and meta-analysis. J Orthop Surg Res 2023;18(01):85. Doi: 10.1186/s13018-023-03561-7
16. Christodoulou N, Wolfe B, Mathes DW, Malgor RD, Kaoutzanis C. Vacuum-assisted closure therapy for the management of deep sternal wound complications: A systematic review and metaanalysis. J Plast Reconstr Aesthet Surg 2024;94:251-260. Doi: 10.1016/j.bjps.2023.09.049
1. Instituto Nacional de Câncer José Alencar Gomes da Silva, Rio de Janeiro, RJ, Brazil
2. Department of Plastic Surgery, Instituto Nacional de Câncer José Alencar Gomes
da Silva, RiodeJaneiro, RJ, Brazil
3. Universidade de São Paulo (USP), São Paulo, SP, Brazil
4. Hospital Vila Nova Star, São Paulo, SP, Brazil
5. Instituto Tocantinense Presidente Antônio Carlos (ITPAC), Palmas, TO, Brasil
Address for correspondence Manoel Vicente Andrade de Souza Junior, Instituto Nacional de Câncer José Alencar Gomes da Silva, Rio de Janeiro, RJ, Brazil (e-mail: vicenteandradeplastica@gmail.com).
Artigo submetido: 03/10/2024.
Artigo aceito: 20/05/2025.
Conflict of Interests
The authors have no conflict of interests to declare.
















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter