

Ideas and Innovation - Year 2025 - Volume 40Issue 1
Intergender Anthropometric Comparison of the Nipple-Areola Complex
Comparação antropométrica intergêneros do complexo areolopapilar
ABSTRACT
Introduction The nipple-areola complex (NAC) plays a fundamental role in the esthetic and functional harmony of the thoracic region, with direct implications for procedures such as gender-affirming surgeries, postbariatric breast reconstructions, and gynecomastia treatments. Although the literature contains several reports on female parameters, data on male NAC remain scarce, hindering proper surgical planning.
Materials and Methods The present cross-sectional study included 440 male subjects aged 18 to 47 years with a bodymass index (BMI) from 18 to 30 kg/m2. The measurements included the internipple distance, the nipple-to-sternal notch distance, the NAC-to-inframammary fold (NAC-IMF) distance, and the horizontal and vertical dimensions of the NAC. We compared the data with the female parameters reported in the literature using descriptive and inferential statistics to assess significant differences.
Results Themale NAC exhibited a greater internipple distance and amore inferior and lateralized positioning than the female NAC. The oblong shape of the male NAC contrasted with the circular pattern observed in females. The NAC-IMF distance was shorter in men than in women.
Conclusion The observed differences reinforce that female parameters are not suitable to guide male surgeries. The current study establishes specific guidelines for the male NAC, contributing to more precise and individualized outcomes in genderaffirming surgeries, breast reconstructions, and gynecomastia treatments, offering an innovative foundation for the clinical practice.
Keywords: anthropometry; gender dysphoria; gynecomastia; mammaplasty; transsexualism
RESUMO
Introdução O complexo areolopapilar (CAP) desempenha papel fundamental na harmonia estética e funcional da região torácica, com implicações diretas em procedimentos como cirurgias de gênero, reconstruções mamárias pós-bariátricas e tratamentos de ginecomastia. Apesar de os parâmetros femininos estarem amplamente descritos na literatura, os dados masculinos permanecem escassos, o que dificulta o planejamento cirúrgico adequado.
Materiais e Métodos Foi realizado um estudo transversal com440 indivíduos do sexo masculino, com idades entre 18 e 47 anos e índice de massa corporal (IMC) entre 18 e 30 kg/m2. Foram coletadas medidas como distância entre os mamilos, distância mamilo-fúrcula, distância CAP-sulco inframamário (SIM) e dimensões horizontal e vertical do CAP. Os dados foram comparados com os parâmetros femininos descritos na literatura, e estatísticas descritivas e inferenciais foram utilizadas para avaliar diferenças significativas.
Resultados O CAP masculino apresentou maior distância entre os mamilos e um posicionamento mais inferior e lateralizado em relação ao feminino. O formato oblongo do CAP masculino contrastou com o padrão circunferencial feminino. A distância CAP-SIM foi menor nos homens comparada à das mulheres.
Conclusão As diferenças observadas reforçam que os parâmetros femininos não são adequados para orientar cirurgias masculinas. Este estudo estabelece diretrizes específicas para o CAP masculino, o que contribui para resultados mais precisos e individualizados em cirurgias de gênero, reconstruções mamárias e tratamentos de ginecomastia, e oferece uma base inovadora para a prática clínica.
Palavras-chave: antropometria; ginecomastia; identidade de gênero; mamoplastia; transexualidade
Introduction
The analysis of the nipple-areola complex (NAC) is a plastic surgery mainstay, playing a significant role ranging from esthetic procedures to complex reconstructions. Although the anthropometric parameters of female NAC are widely documented and used as a reference in the clinical practice, data regarding male NAC remain limited and scattered in the literature. This disparity highlights the need for studies that clarify male morphological characteristics, contextualizing these measurements regarding the widely-established female values.
The anthropometric standards of the female NAC are fundamental guides in breast augmentation, reduction, and reconstruction surgeries,1–3 and they have undergone validation in different populations. These studies have identified specific proportions, such as the ideal distances from the nipple to the sternal notch and to the inframammary fold (IMF), which are widely used in the surgical practice. In contrast, the male NAC presents unique challenges, requiring an approach considering the lack of breast volume and the need for harmony in a flat chest. Recent work4,5 suggests using predictive algorithms to optimize male NAC positioning and dimensions based on individual measurements.
The present study aims to fill a critical gap by comparing, for the first time, male anthropometric parameters and female standards established in the literature. Our methodology associates original data from a representative male sample with the most cited female references, facilitating an intergender analysis with implications that extend beyond traditional surgical applications. In addition to contributing to the improvement of anatomical knowledge, the data provide support for advances in gender affirmation surgeries, postbariatric breast reconstructions, and gynecomastia correction.
The integration of comparative analyses between genders enables the formulation of updated guidelines for esthetic and restorative interventions, meeting the growing demand for evidence-based practices that consider individual and gender-specific needs. Thus, we propose a critical review and redefine metrics to support excellent practice in contemporary plastic surgery.
Objective
The current study aims to perform a comparative analysis of the anthropometric parameters of the male NAC obtained from original data and the references established in the literature on the female NAC.
Materials and Methods
Study Design
The present is an observational, descriptive, and cross-sectional study. The investigation included primary data collection among male subjects and a systematic literature review to consolidate the female parameters widely used in the clinical practice.
Literature Review
We performed a systematic review in the PubMed, Scopus, and Web of Science databases with the descriptors female nipple-areola complex anthropometry, breast measurements, reconstruction surgery, and mammaplasty. We included studies from the last 20 years containing clear information on NAC distances to the sternal notch and IMF, areolar diameter, and intermammary distance. We excluded studies presenting non-quantitative data or non-representative samples.
Established Standards for the Female NAC
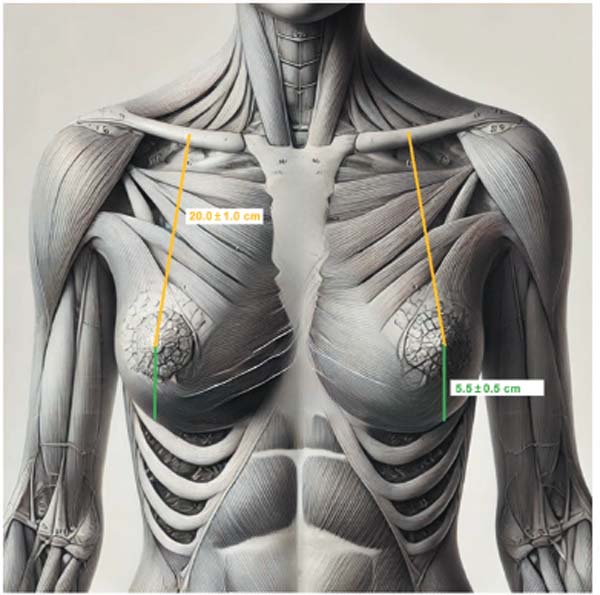
Vandeput and Nelissen6 (2002) reported the distance from the nipple to the sternal notch as ranging from 19 to 21 cm and the internipple distance, from 18 to 22 cm.
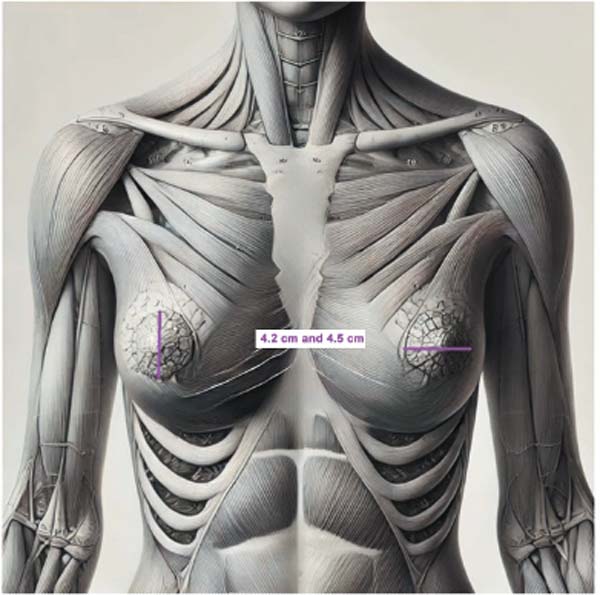
Tepper et al.2 (2010) described the average diameter of the areola ranging from 4.2 to 4.5 cm.
De la Torre and Davis7 (2015) reported the distance between the nipple and IMF ranging from 5 to 6 cm.
Collected Measurements
NAC measurements
Vertical diameter of the areola (in centimeters).
Horizontal diameter of the areola (in centimeters).
Body Proportions and Distances
Internipple distance
Distance from the nipple to the clavicle, sternal notch, and IMF (right and left sides)
Humerus length (right and left sides)
Distance from the sternal notch to the umbilicus
Circumference of the chest, waist, neck, biceps, forearm, and wrist (right and left sides)
Height and body weight.
Statistical Analysis
We tabulated the data in Microsoft Excel (Microsoft Corp.) spreadsheets and analyzed it using the IBM SPSS Statistics for Windows (IBM Corp.) software.
We calculated means, standard deviations, and 95%CIs for each variable.
The comparison between the male data and the female data described in the literature used the Student’s t-test for independent samples.
The Mann-Whitney U test was used to compare nonparametric variables or those with asymmetric distribution.
The significance level was set at p < 0.05.
Ethical Considerations
All participants signed an informed consent form in accordance with the ethical guidelines for research involving human beings.
The study was approved by the Central Army Hospital Study Center, which waived the need for review by a formal ethics committee due to the descriptive and noninterventionist nature of the study.
Results
Study Participants
The sample consisted of 440 male participants aged 18 to 47 years and with a BMI ranging from 18 to 30 kg/m2.
After excluding subjects with chest or nipple deformities, we included 401 participants in the analysis.
Thoracic Deformities
Male Data Segmentation
NAC-related Patterns:
NAC Distances
NAC (Horizontal and Vertical) Dimensions
Patterns per Group:
BMI
◦ Subjects with higher BMI often have greater internippledistance and larger chestcircumference (►Table 2).
◦ Differences in the nipple-sternal notch or nipple-IMF distances are smaller, suggesting that these measurements remain stable across BMIs.
Age Range
Measurement Correlations:
Applications:
Based on these patterns:
Measurement standardization: The stability in NAC dimensions across different subgroups suggests the feasibility of creating reference values.
Predictive modeling: It is possible to develop models based on variables such as height, BMI, and chest width to estimate NAC measurements.
Clinical impact: These standards can guide reconstructive or cosmetic surgeries, especially in cases of gynecomastia or gender-affirming procedures.
| Height range | Clavicle-NAC distance (R): mean±SD | Clavicle-NAC distance (L): mean±SD | Sternal notch-NAC distance (R): mean±SD | Sternal notch-NAC distance (L): mean±SD | Vertical NAC diameter (R): mean±SD | Vertical NAC diameter (L): mean±SD | Horizontal NAC diameter (R): mean±SD | Horizontal NAC diameter (L): mean±SD | Inter-NAC distance: mean±SD | NAC-IMF distance (R): mean±SD | NAC-IMF distance (L): mean±SD | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 1,67 | 17, 8±1,4 | 17,9±1,3 | 17,8 ±1,1 | 17,9±1,2 | 2±0,3 | 2±0,3 | 2,8 ±0,5 | 2,8±0,5 | 20,7±1,5 | 3,4±0,6 | 3.6±0,6 | |||||||||||
| 1,67–1,76 | 18,3±1,5 | 18,5±1,4 | 18, 4±1,3 | 18, 5±1,3 | 2±0,4 | 2±0,4 | 2,9 ±0,4 | 2,9±0,4 | 21, 5±1,5 | 4±0,8 | 4±0,9 | |||||||||||
| 1,77–1,87 | 19,1±1,6 | 19,4±1,5 | 19, 2±1,4 | 19, 4±1,4 | 2,1±0,4 | 2.1±0,4 | 3±0,4 | 3±0,4 | 22, 1±1,7 4,3±1 | 4,3±0,9 | 0.9 | |||||||||||
| > 1,87 | 19±1,5 | 19,1±1,5 | 19,2 ±1,5 | 19,3±1,7 | 2,1±0,2 | 2±0,3 | 2.8±0,3 | 2.9±0,3 | 23, 4±3,2 | 4,5±0,7 | 4,5±0,9 |
| Thorax circumference | Clavicle-NAC distance (R): mean ± SD | Clavicle-NAC distance (L): mean ±SD | Sternal notch-NAC distance (R): mean ± SD | Sternal notch-NAC distance (L): mean ±SD | Inter-NAC distance: mean ± SD | NAC-IMF distance (R): mean ± SD | NAC-IMF distance (L): mean ±SD | Vertical NAC diameter (R): mean ± SD | Vertical NAC diameter (L): mean ± SD | Horizontal NAC diameter (R): mean ± SD | Horizontal NAC diameter (L): mean ±SD | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 83 | 16.7 ± 1 | 16.9 ±0.9 | 17.1 ±0.8 | 17.2 ±0.9 | 19.5 ±1.2 | 3.5 ±0.6 | 3.5 ± 0.6 | 2 ±0.2 | 2 ±0.3 | 2.7 ±0.4 | 2.8 ±0.4 | |||||||||||
| 83-90 | 18 ±1.2 | 1 8.2 ±1.1 | 1 8.4 ±1.2 | 1 8.2 ±1.1 | 21 ±1.3 | 4.1 ±0.9 | 4.1 ±0.9 | 2 ±0.4 | 2 ±0.4 | 2.8 ±0.4 | 2.8 ±0.4 | |||||||||||
| 91-100 | 19.2 ± 1.4 | 19.3 ±1.2 | 19.3 ±1.2 | 19.3 ±1.2 | 22.3 ±1.5 | 4.1 ±0.9 | 4.1 ±0.9 | 2.1 ±0.4 | 2.1 ±0.4 | 3 ±0.4 | 3 ±0.4 | |||||||||||
| > 100 | 20 ±1.2 | 20.2 ±1.2 | 20.1 ±1.1 | 20.2 ±1.2 | 24 ±1.5 | 4.5 ±0.8 | 4.5 ±1 | 2.3 ±0.4 | 2.3 ±0.4 | 3.2 ±0.5 | 3.2 ±0.5 |
| Thorax width | Clavicle-NAC distance (R): mean ± SD | Clavicle- | Clavicle-NAC distance (L): mean ±SD | Sternal notch-NAC distance (R): mean ±SD | Sternal notch-NAC distance (L): mean ± SD | Inter-NAC distance: mean ±SD | NAC-IMF distance (R): mean ±SD | NAC-IMF distance (L): mean ± SD | Vertical NAC diameter (R): mean ± SD | Vertical NAC diameter (L): mean ± SD | Horizontal NAC diameter (R): mean ± SD | Horizontal NAC diameter (L): mean ±SD | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 27 | 16.2 ±0.3 | 16.3 ±0.6 | 16.8 ±0.3 | 16.8 ±0.8 | 20.8 ±0.8 | 4.5 ±0.3 | 4.3 ±0.3 | 2.1 ±0.4 | 2 ±0.3 | 2.8 ±0.3 | 2.8 ±0.3 | |||||||||||
| 27-31 | 17.9 ±1.3 | 18.1 ±1.3 | 18.1 ±1.1 | 18.2 ±1.1 | 20.9 ±1.3 | 3.9 ±0.9 | 3.9 ±0.9 | 2 ±0.4 | 2 ± 0.^4 | 2.8 ±0.4 | 2.8 ±0.4 | |||||||||||
| 32-37 | 19 ± 1.4 | 19.1 ±1.3 | 19 ± 1.3 | 19.1 ±1.3 | 22.1 ±1.7 | 4.2 ±0.9 | 4.2 ±0.9 | 2.1 ±0.4 | 2.1 ±0.4 | 2.9 ±0.4 | 2.9 ±0.4 | |||||||||||
| > 37 | 20.1 ±1.4 | 20.3 ±1.4 | 20.1 ±1.3 | 20.4 ±1.2 | 24.2 ±1.3 | 4.3 ±1 | 4.4 ±1 | 2.2 ±0.3 | 2.1 ±0.4 | 3.2 ±0.5 | 3.2 ±0.4 |
Discussion
The results of the current study highlight the need for an intergender anthropometric approach to the NAC, emphasizing fundamental differences between male and female standards and their implications for the surgical practice. Comparing the male data from the present study with the female parameters established in the literature, it is evident that the morphology of the male NAC requires specific guidelines for esthetic and reconstructive interventions.1–3,8
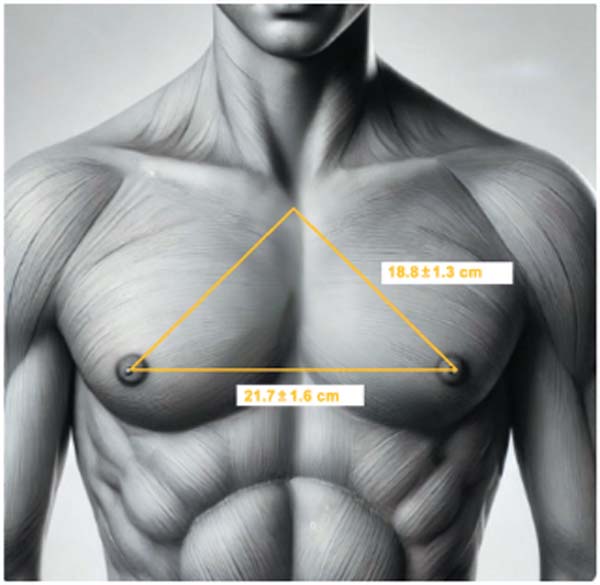
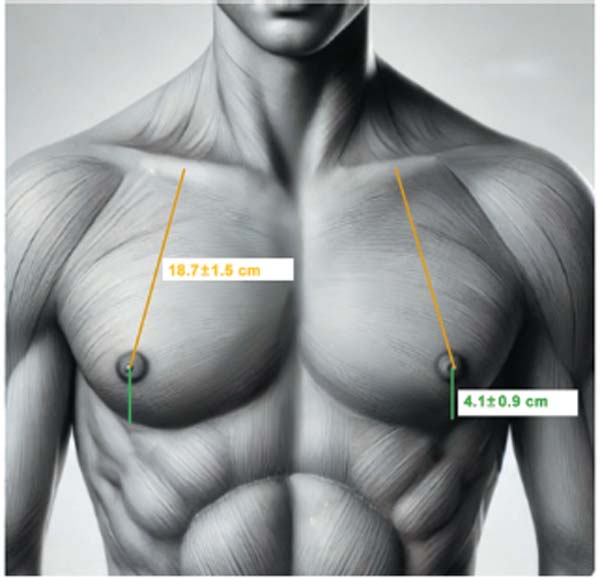
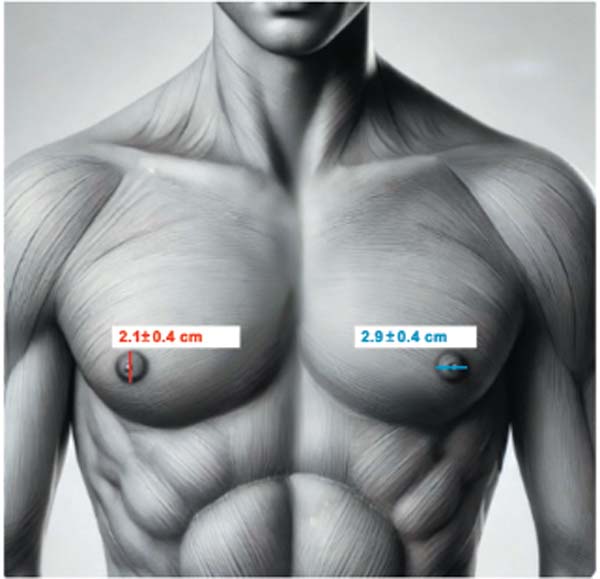
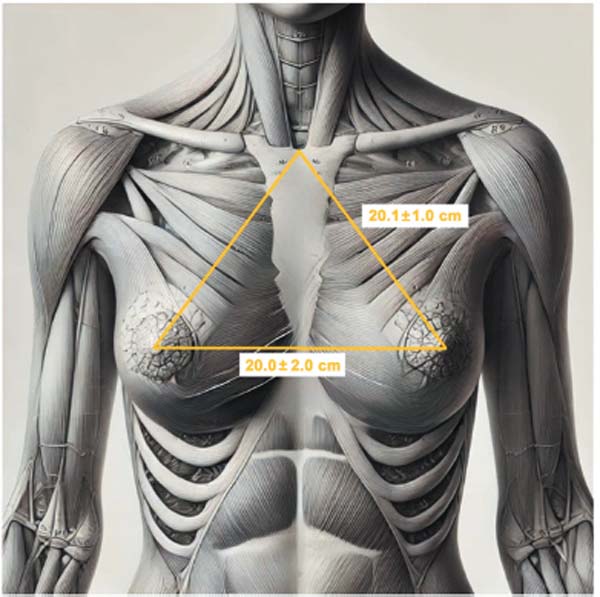
The comparative analysis revealed statistically significant differences between genders in terms of several variables. The mean internipple distance was greater in males (21.7±1.6 cm) (►Fig. 1) than in females (18 – 22 cm) (►Fig. 4).1,2 The mean nipple-sternal notch distance was shorter in men (18.8±1.3 cm) (►Fig. 1) than in women (19,1 – 21,1 cm) (►Fig. 4),7 with p < 0.001. The mean NAC-IMF distance was also significantly shorter in the male group (4.1±0.9 cm) (►Fig. 2) than in women (5–6 cm) (►Fig. 5).7 The mean NAC diameter showed lower values in men, with a mean horizontal diameter of 2.9 ± 0.4 cm and a mean vertical diameter of 2.1±0.4 cm (►Fig. 3), compared with the mean female measurements of 4,2 cm and 4,5 cm respectively (►Fig. 6).1,2 Furthermore, the mean clavicle-NAC distance was shorter in men (18.7±1.5 cm) (►Fig. 2) than in women (19 – 21 cm) (►Fig. 5).1,7
In addition to the distance measurements, the shape of the male NAC was predominantly oblong, contrasting with the circumferential pattern observed in women.9,10 This difference is crucial, as male surgeries often use instruments and techniques based on female standards, potentially leading to unsatisfactory outcomes, such as asymmetries and disproportions.
Studies in women often indicate NACs centered on the breast, while the data herein presented show that the male NAC positioning tends to be more inferior and lateralized.11,12 This discrepancy reinforces the inadequacy of adopting female standards as a reference for male interventions and highlights the significance of establishing specific and validated male parameters.
The choice of a sample composed of healthy, mixed-race Brazilian subjects with no thoracic deformities provided the study with methodological robustness and clinical relevance, enabling the identification of consistent patterns with potential international applicability. Additionally, we observed the influence of variables such as height and BMI on NAC positioning and dimensions, indicating the need for personalized surgical procedures.
The findings contribute significantly to improving approaches in gender surgery, postbariatric reconstructions, and gynecomastia treatments, highlighting the importance of individualized planning based on male anthropometric evidence. Future studies are recommended to expand sampling and explore ethnic and morphological variations to refine clinical guidelines applicable to the contemporary surgical practice.
Conclusion
The present comparative study of the anthropometric parameters of the male NAC and the female references established in the literature revealed essential differences and similarities applicable to the surgical practice. While both genders share general proportions that ensure thoracic harmony, they present significant differences regarding NAC distances, shapes, and positioning.
The male NAC had a greater internipple distance and a more inferior and lateralized positioning than the female NAC. Additionally, the oblong shape of the male NAC contrasted with the circumferential female pattern, emphasizing the inadequacy of applying female measurements as a direct reference in male surgeries. These findings reinforce the need for specific guidelines for the male NAC respecting its unique anatomical characteristics.
By exploring the implications of these differences, the current study contributes significantly to the improvement in surgical practices in contexts such as gender surgery, postbariatric breast reconstruction, and gynecomastia treatments. The adoption of evidence-based male anthropometric parameters can improve esthetic and functional outcomes, promoting greater accuracy and patient satisfaction.
Therefore, the present study not only fills a gap in the literature by presenting a robust comparative model but also provides an innovative foundation for advances in the clinical practice, highlighting the importance of tailored and evidence-based approaches for excellence in plastic surgery.
REFERENCES
1. Liu X, et al. Anthropometric measurements of the breast region in young women of different body types. J Plast Reconstr Aesthet Surg 2011;64(01):38–44
2. Tepper OM, Small KH, Unger JG, Feldman DL, Choi NKM, Karp NS. 3D analysis of breast augmentation defines operative changes and their relationship to implant dimensions. Ann Plast Surg 2009;62 (05):570–575 10.1097/SAP.0b013e31819faff9
3. Liu X, et al. Dimensions of the nipple-areola complex in normal young women. J Plast Reconstr Aesthet Surg 2011;64(04):528–534
4. Maas SM, et al. Anthropometric analysis of male chest and breast anatomy: Implications for surgical correction of gynecomastia. Plast Reconstr Surg 2019;143(02):363–370
5. Timmermans F, et al. A systematic review of male chest aesthetic parameters: Implications for surgery and body contouring. Plast Surg (Oakv) 2021;29(01):1–9
6. Vandeput JJ, Nelissen M. Considerations on anthropometric measurements of the female breast. Aesthetic Plast Surg 2002;26(05): 348–355 10.1007/s00266-002-2039-1
7. De la Torre JI, Davis MR. Anatomia em cirurgia plástica da mama. In: Neligan PC, editor. Cirurgia plástica volume 5: mama. Amsterdã: Elsevier; 2015
8. Tanini S, et al. Anthropometric study of the male nipple-areola complex: Its position and dimensions for optimal aesthetic outcome. J Plast Surg Hand Surg 2018;52(01):29–34
9. Agarwal S, et al. Male breast surgery: A review of the techniques and outcomes. Aesthet Surg J 2017;37(06):654–662
10. Hassanpour S, et al. Anatomy and aesthetics of the male chest wall: Proposals for surgical improvement. Eur J Plast Surg 2018;41 (05):545–553
11. Yue C, et al. A comprehensive analysis of male nipple-areola complex placement: Implications for gynecomastia and reconstructive surgery. Aesthetic Plast Surg 2018;42(04):941–948
12. Quieregatto PR, et al. Anthropometric analysis of the nippleareola complex in the female breast. Aesthet Surg J 2014;34 (02):237–242
1. Universidade Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil
2. Hospital Central do Exército (HCE), Rio de Janeiro, RJ, Brazil
Address for correspondence Mariana Brandão Miqueloti Inglez, (e-mail: miqueloti@gmail.com).
Article received: January 09, 2025.
Article accepted: March 20, 2025.
Study performed at the Department of Plastic and Reparative Surgery, Hospital Central do Exército, Rio de Janeiro, RJ, and at the Department of Surgery, Escola Paulista de Medicina, Universidade Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil.
Conflict of Interests
The authors have no conflict of interests to declare.










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter