

Ideas and Innovation - Year 2025 - Volume 40Issue 1
Breast Implant Explantation and Asterisk Remodeling
Explante de implante mamário e remodelamento em asterisco
ABSTRACT
The use of silicone implants has changed breast augmentation surgery, whether for esthetic or reconstructive reasons. Recently, there have been new discussions about the safety of these implants and increased demands for explant surgery. Reasons include patients' request, device rupture, capsular contracture, fear of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL), squamous cell carcinoma, and the controversial silicone disease. Regardless of the indication for removal or replacement, implants are not definitive devices. Removal causes a critical change in the shape of the breast, which, when performed in isolation, can generate dissatisfaction and often a feeling of mutilation. The explantation technique should involve device removal, surgical treatment of the capsule, and a breast restructuring procedure. This study aimed to report the case of a patient who underwent explantation after implant rupture, followed by fat grafting and tissue restructuring using the Asterisk technique.
Keywords: breast; breast implants; implant capsular contracture; mammaplasty; safety-based medical device withdrawals
RESUMO
O uso dos implantes de silicone mudou a cirurgia de aumento mamário, seja por questões estéticas ou reparadoras. Recentemente ocorreram novas discussões sobre a segurança desses implantes e maior procura pela cirurgia de explante. Os motivos incluem solicitação de pacientes, ruptura dos implantes, contratura capsular, o medo do linfoma anaplásico de células grandes associado a implante mamário (breast implant-associated anaplastic large cell lymphoma, BIA-ALCL, em inglês), carcinoma epidermoide, assimcomo a controversa doença do silicone. Independente da indicação da retirada ou troca, os implantes não são definitivos. A remoção provoca uma mudança importante na forma da mama que, quando realizada de forma isolada, pode gerar insatisfação e muitas vezes sensação de mutilação. A técnica de explante deve envolver a retirada do implante e tratamento cirúrgico da cápsula, associada a um procedimento de reestruturação da mama. Esse relato de caso tem o objetivo de descrever o caso de uma paciente submetida ao explante após ruptura de um implante, sendo feito uma lipoenxertia e reestruturação dos tecidos por meio da técnica em asterisco.
Palavras-chave: contratura capsular em implantes; implante mamário; mama; mamoplastia; retirada de dispositivo médico baseada em segurança
Introduction
Cronin’s introduction of silicone implants in the early 1960s changed breast augmentation surgery.1 Patients who have undergone its placement report a significant improvement in their quality oflife and body image.2-4Recently, the discussion about the safety of implants has returned, increasing the demand for explants.
Reasons for removal include patients’ request, capsular contracture, device rupture, fear of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL), and silicone disease.5 Data linking implants to silicone disease are scarce, with no proposed mechanism. Women with systemic complaints reported receiving little attention fromtheir doctorsandexpressed theirfrustrations on social media, generating significant anxiety and misinformation.4,6 Patients seeking this procedure due to systemic complaints opt for autologous explantation and reconstruction.7
Implant removal causes a dramatic change in the breast, especially in larger ones. Removing implants without remodeling generates dissatisfaction and often a feeling of mutilation.5
Objective
The current report aimed to present the case of a patient who underwent breast implant explantation and to highlight a technical treatment option for subjects seeking definitive breast explantation, an increasingly frequent event in clinical practice.
Materials and Methods
Case Report
A white female patient underwent breast augmentation in 2010. At the time, she was 22 years old, weighing 64 kg, and measuring 1.71 m in height, with complaints of hypomastia. Physical examination revealed hypoplastic, symmetrical breasts with good upper breast coverage. Each breast received a 275 mL, round, textured implant. The approach was at the inframammary fold, and implant placement occurred in the subfascial plane.
In the immediate postoperative period, the patient found her breasts somewhat small. However, she reported subsequent acceptance. In 2018, at age 30, with the same weight and height, and asymptomatic, the patient underwent a routine ultrasound. The test revealed rupture of the right implantand a nodule (0.7 cm) at the quadrant junction of the left breast, which was biopsied and diagnosed as fibroadenoma.
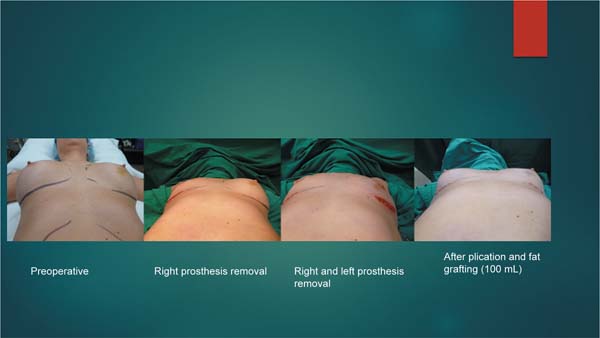
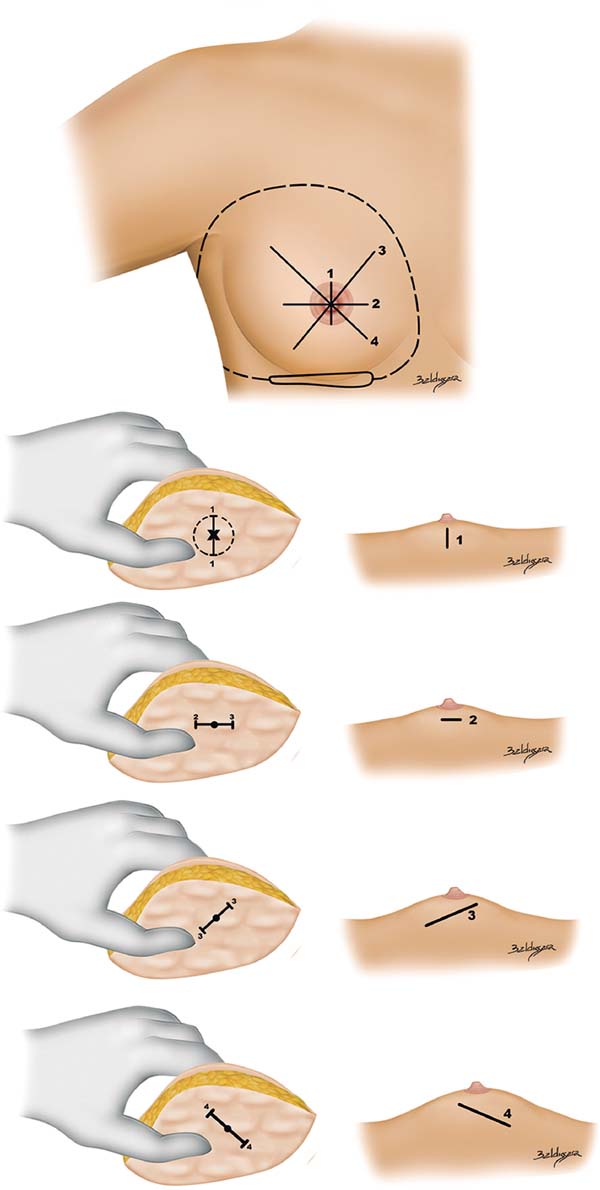
The patient opted for permanent explantation, removing the implants and their capsules using the same incision in the inferior mammary fold, but 2 cm larger than the original one. Each breast received a 100 mL fat graft, both peripherally and subcutaneously, preserving the intact mammary gland. Breast tissue remodeling was performed through an internal asterisk plication in the center of both breasts, starting behind the nipple-areola complex (NAC) region to reconstruct breast projection. After the plication, the internal projection of the NAC was fixed to the chest wall to minimize subsequent breast ptosis (►Fig. 1,3). At a follow-up visit 1 year later, the patient reported satisfaction with the projection and shape of her breasts (►Fig. 2).
Results
Fat grafting and breast assembly with asterisk, concentric sutures in the breast parenchyma resulted in proper NAC projection, with its position fixed in the pectoral fascia to prevent residual ptosis. The case progressed satisfactorily with no outcome loss during the follow-up.
Discussion
The emergence of new questions about the effects of silicone implants and the information disseminated on social media increased the demand for removal. Social media describes a myriad of symptoms attributed to silicone, including malaise, fatigue, fibromyalgia, and headaches. To date, no study has demonstrated a cause-and-effect relationship with the so-called silicone disease. A theory links the disease to an overstimulation of the immune system, potentially representing a type of allergic response, but this is conjecture.5,6,8
Explant planning requires thorough history taking and physical examination. The desired breast volume and shape after explantation, as well as the acceptance of additional scars, are discussed in detail. The degree of ptosis, amount of breast tissue, areola size, volume, implant type and position, and degree of skin elasticity are assessed.1,9 Procedures such as mastopexy and fat grafting are often necessary to achieve satisfactory outcomes.4
Some authors recommend capsule removal for the same reason as prosthesis removal, since it can be intact in selected asymptomaticcases.Theyalsorecommendpartial or complete capsulectomy for grade-III and -IV contractures.5 Histopathological analyses of resected capsules may reveal evidence of silicone, even in intact implants from asymptomatic patients.10 Studies differ on the recurrence of systemic symptoms and capsular contracture after implant replacement.4,5,7,8
The indication for en bloc capsulectomy, that is, implant and capsule removal in a single anatomical piece, occurs only when BIA-ALCL cannot be ruled out, as capsule fragments may result in lesion recurrence and impact patients’ survival.3
We performed a permanent removal of the implants and complete removal of capsules in the subglandular plane. Fat grafting and breast assembly with fan-shaped, concentric sutures in the breast parenchyma resulted in proper NAC projection, with its position fixed in the pectoral fascia to prevent residual ptosis. The case progressed satisfactorily, with no outcome loss at follow-up.
Conclusion
This case highlights an asymptomatic patient with a ruptured implant who requested removal without prosthetic replacement. It is worth emphasizing that achieving satisfactory results is easier with a correct diagnosis and aligned expectations before surgery. The simple technique of fat grafting and breast remodeling should be in the arsenal of anyone performing explants. Clear guidance regarding the surgical limitations and results is essential for these procedures, which require extensive discussion in academic circles as they become increasingly common.
References
1. Rohrich RJ, Beran SJ, Restifo RJ, Copit SE. Aesthetic management of the breast following explantation: evaluation and mastopexy options. Plast Reconstr Surg 1998;101(03):827-837. Doi: 10.1097/00006534-199803000-00039
2. FDA. FDA Strengthens Breast Implant Safety Requirements. Silver Spring, MA: FDA; 2021. Available from: https://www.fda.gov/medical-devices/implants-and-prosthetics/breast-implants
3. Macadam SA, Ho AL, Cook EF Jr, Lennox PA, Pusic AL. Patient satisfaction and health-related quality of life following breast reconstruction: patient-reported outcomes among saline and silicone implant recipients. Plast Reconstr Surg 2010;125(03): 761-771. Doi: 10.1097/PRS.0b013e3181cb5cf8
4. Suh LJ, Khan I, Kelley-Patteson C, Mohan G, Hassanein AH, Sinha M. Breast Implant-Associated Immunological Disorders. J Immunol Res 2022;2022:8536149. Doi: 10.1155/2022/8536149
5. Calobrace MB, Tanna N, Mays C. An Algorithm for the Management of Explantation Surgery. In: Calobrace MB, Kortesis BG, Bharti G, Mays C, editors. Augmentation Mastopexy: Mastering the Art in the Management of the Ptotic Breast. Cham, Switzerland: Springer; 2020:229-246. Doi: 10.1007/978-3-030-48226-8
6. Tang SYQ, Israel JS, Afifi AM. Breast implant illness: symptoms, patient concerns, and the power of social media. Plast Reconstr Surg 2017;140(05):765e-766e. Doi: 10.1097/PRS.00000000 00003785
7. Miseré RML, Van der Hulst RRWJ. Self-Reported Health Complaints in Women Undergoing Explantation of Breast Implants. Aesthet Surg J 2022;42(02):171-180. Doi: 10.1093/asj/sjaa337
8. Shoenfeld Y, Agmon-Levin N. ‘ASIA’ - autoimmune/inflammatory syndrome induced by adjuvants. J Autoimmun 2011;36(01):4-8. Doi: 10.1016/j.jaut.2010.07.003
9. Rohrich RJ, Parker TH III. Aesthetic management of the breast after explantation: evaluation and mastopexy options. Plast Reconstr Surg 2007;120(01):312-315. Doi: 10.1097/01.prs.00002644 00. 42376.e9
10. Azahaf S, Spit KA, de Blok CJM, Bult P, Nanayakkara PWB. Silicone Migration from Intact Saline Breast Implants. Plast Reconstr Surg Glob Open 2024;12(02):e5608. Doi: 10.1097/GOX.0000000 000005608
1. Division of General Surgery, Hospital Moinhos de Vento, Porto Alegre, RS, Brazil
Address for correspondence Sirlei dos Santos Costa, Serviço de Cirurgia Geral, Hospital Moinhos de Vento, Porto Alegre, RS, Brazil (e-mail: sirlei@sirleicosta.com.br).
Artigo submetido: 20/08/2024.
Artigo aceito: 14/07/2025.
Conflict of Interests
The authors have no conflict of interests to declare.







 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter