

Original Article - Year 2011 - Volume 26 -
Early nasal symmetry after rhinoplasty associated with cheiloplasty in children with cleft lip and palate
Simetria nasal após a realização de rinoplastia associada à queiloplastia em crianças com fissura labial e labiopalatal
ABSTRACT
Introduction: Rhinoplasty performed in association with cheiloplasty after the age of 2 months enables reduction of nasal deformities and facilitates minor corrections. Objective: We aimed to assess the nasal symmetry achieved early after rhinoplasty performed concurrently with cheiloplasty in children with unilateral cleft lip or palate. Methods: Forty-one patients with unilateral cleft lip or palate underwent cheiloplasty by Millard's technique and rhinoplasty by the McComb and Salyer technique at the average age of 9.2 months (age range, 2 months to 9 years). The nasal symmetry between the normal and the cleft sides was assessed by using postoperative photographs 6 months after the surgery. Results: The nasal symmetry was considered excellent and good in 53.66% and 46.34% of the patients, respectively. Conclusion: Rhinoplasty performed concurrently with cheiloplasty ensures good early nasal symmetry in children with unilateral cleft lip or palate.
Keywords: Rhinoplasty. Nose/abnormalities/surgery. Cleft Lip/surgery. Fissura Palatina/surgery. Reconstructive Surgical Procedures/methods.
RESUMO
Introdução: A realização da rinoplastia associada à queiloplastia após os dois meses de idade possibilita reduzir as deformidades nasais e facilita correções secundárias. Objetivo: O objetivo deste trabalho é avaliar a simetria nasal após a realização de rinoplastia associada à queiloplastia em crianças com fissura labial e labiopalatal unilateral. Método: Foram avaliados 41 pacientes após os seis meses de cirurgia. Os pacientes foram submetidos à queiloplastia pela técnica de Millard associada à rinoplastia pela técnica de McComb. Utilizando as fotografias do pós-operatório, avaliou-se a simetria nasal entre o lado normal e fissurado. Resultados: A simetria nasal foi considerada excelente em 53,66% dos casos, bom em 46,34% e nenhum paciente foi ruim. Conclusão: A avaliação da rinoplastia propiciou bons e excelentes resultados.
Palavras-chave: Rinoplastia. Nariz/anormalidades/cirurgia. Fenda Labial/cirurgia. Procedimentos Cirúrgicos Reconstrutivos/métodos.
The nasal treatment of patients with cleft lip and palate was always a challenge for plastic surgeons. Because of the fear of interfering with the growth of the nasal structures, nasal defects were corrected only after the full development of these anatomic parts. Consequently, children with these defects grew with the stigma of nasal deformity, and delayed treatment was very difficult.
Stenström and Oberg1 studied the pathogenesis of nasal deformity in patients with cleft lip and found that the loss of continuity of the oral muscular sphincter associated with lateral traction by the facial muscles explained the anomalous position of the columella, nasal septum, alar base, and change in the greater alar cartilage contour on the cleft side.
The first surgical techniques for cleft lip correction focused only on the lip defect, and not the associated nasal changes. With developments in the surgical treatments, the need to correct nasal deformities was evident, because the facial imbalance caused by the nasal changes was a considerable problem despite good lip repair2. Blair3 and Brown and McDowell4 pioneered cleft nose treatment and planted the first seeds for rhinoplasty associated with cheiloplasty. Thereafter, Brown and McDowell4 and Steffensen5 suggested internal and external incisions in the nostril opening, medial rotation of the greater alar cartilage, and removal of any excess cartilage. However, the results of these procedures were unsatisfactory, because the cartilage was malpositioned rather than excessive; moreover, good nasal symmetry was lacking and the scars were conspicuous.
In general, the first results of rhinoplasty associated with cheiloplasty were unsatisfactory, mainly because of the large incisions performed along the nasal contour in association with intercartilaginous incisions or external incisions in the nose, around the greater alar cartilages. Consequently, many patients developed nostril stenosis and deformities due to scar retraction, emphasizing the question of the suitability of primary rhinoplasty.
Berkeley6, a great researcher of the characteristics of patients with nasal cleft, found that delayed rhinoplasty rarely yielded satisfactory results in functional and aesthetic terms. Further, Anastassov et al.7 assessed 54 patients who underwent delayed rhinoplasty by means of rhinomanometry and geometric analysis. Olfactory disorders and nasal patency were verified in most patients, besides inadequate midfacial and nasal development. The authors concluded that rhinoplasty should be performed concurrently with cheiloplasty, because delayed rhinoplasty shows poor esthetic and functional results.
The objectives of rhinoplasty performed concurrently with cheiloplasty after the age of 2 months are rebuilding or relocating the structures to their normal anatomic site, minimizing secondary deformities, and promoting better physical and psychosocial development of children. Of the several techniques of primary rhinoplasty, each surgeon should choose those that best fit the case and provide good correction of nasal deformities and asymmetries. The actual result of rhinoplasty can be observed only in the long term, especially in patients who may undergo additional facial surgeries or in growing patients; therefore, follow-up until adolescence is very important.
In this study, we aimed to assess the nasal symmetry achieved early after rhinoplasty performed concurrently with cheiloplasty in children with unilateral cleft lip or palate.
METHODS
The study included 41 patients (27 boys and 14 girls) operated between February 2004 and November 2007. Eleven of the patients were black, 20 were white, and the remaining were of mixed race. All the children had nonsyndromic unilateral cleft lip or palate: 15 had cleft lip and 26 had cleft palate. Further, all the malformations were corrected (lip, nose, and palate). The patients' parents or legal guardians were thoroughly informed about the treatment and signed a consent form authorizing the surgery as well as the case study and photographs before and after the surgery.
All the patients were operated by the main author and routinely followed for at least 6 months postoperatively. The patients underwent cheiloplasty and rhinoplasty from the age of 2 months, with the average age at the time of the surgery being 9.2 months (age range, 2 months to 9 years).
Cheiloplasty was performed by Millard's technique, type 2 (Figure 1), and rhinoplasty followed the principles described by McComb and Salyer (Figure 2), along with the postoperative use of intranasal silicone molds to assist modeling and repositioning of the nasal structures2,8-12. After 14 days, the stitches and intranasal mold were removed. Septoplasty was not performed in any patient.
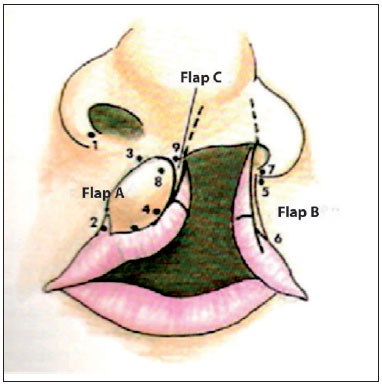
Figure 1 - Cheiloplasty marking in Millard's technique.
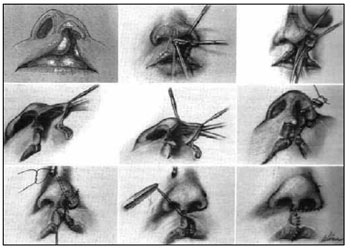
Figure 2 - Primary rhinoplasty by the McComb and Salyer technique.
The patients were recalled after 6 months to be photographed by the surgeon. The photographs included the front, right, and left profiles, half-right and half-left profiles, and the view with the head tilted backward to show the nostrils and nasal tip. All photographs were taken at a distance of 1 m away from the patient and used to analyze the nasal symmetry in the vertical and horizontal planes, and the nasal tip deviation.
In the vertical plane, nasal deviation was measured in relation to the sagittal midline view (Figure 3), and vertical alar dystopia was assessed in relation to the interpupillary line (Figure 4). With the postoperative photographs, reference lines were traced, the existence of nasal deviation was assessed, the angle between the nasal axis and the sagittal midline was calculated, and finally, the distance between the left and right alar bases was measured in relation to the interpupillary plane. From the horizontal aspect, the distances between the midpoint of the base of the columella and the most lateral portion of the left and right alar areas were calculated (Figure 5 and 6)7.
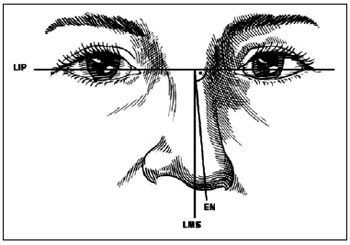
Figure 3 - Nasal axis deviation. LIP, interpupillary line; LMS, sagittal midline; EN, nasal axis. The angle formed between the LMS and the EN is the nasal deviation in relation to the vertical plane.
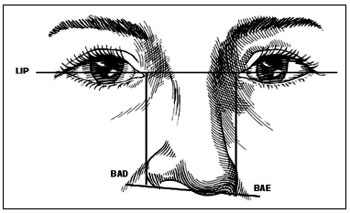
Figure 4 - Vertical position of the alar bases. LIP, interpupillary line; BAD, right alar base; BAE, left alar base.
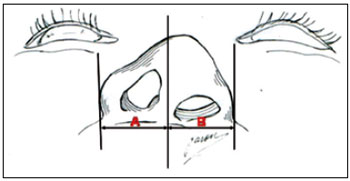
Figure 5 - Assessment in the horizontal plane. A: Distance from the right ala to the columella midline (LMC); B: Distance from the left ala to the columella midline.

Figure 6 - Assessment of nasal symmetry.
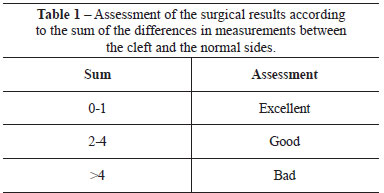
The results were assessed according to a numeric scale related to the differences in the measurements (in millimeters) between the normal and the cleft sides. The sum of the differences in both the vertical and the horizontal planes yielded a number that allowed classification (Table 1). For example, a 1 mm vertical difference and 1 mm horizontal difference totaling 1 + 1 was used to assess the results7.
RESULTS
Table 1 presents the assessment of the results by the sum of the differences in measurements between the cleft and the normal side.
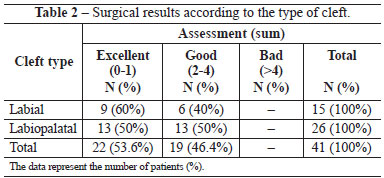
Table 2 shows the surgical results according to the type of cleft. The patients showed good nasal symmetry and contour, and improved nasal tip projection, especially nostril retropositioning and elongation on the cleft side. Another improved feature was the nasal axis deviation with respect to the sagittal midline: half of the patients showed no deviation, while others showed minor changes ranging from 3 to 10 degrees. No complication related to rhinoplasty was observed during the study period. Figure 7 demonstrates some clinical cases, showing the presurgical and postsurgical findings.

DISCUSSION
McComb presented his technique of primary rhinoplasty for the first time at the Sixth International Congress of Plastic and Reconstructive Surgery in 1975, causing a lot of discussion, because many surgeons believed that it harmed the nasal growth in children with facial clefts. McComb followed his patients and after 10 years, and in 1985, published satisfactory results of cases of rhinoplasty associated with cheiloplasty. Subsequently, several studies demonstrated no change in the facial development with McComb's technique, making it a standard surgery in several centers for the treatment of cleft lip and palate2,6,8,13-19.
Early correction of nasal defects enables greater repositioning of the alar cartilages, better nasal tip projection, and better contour of the nostrils. However, with the patient's growth, it may be necessary to make minor corrections to ensure a harmonious and symmetric nose. The greatest benefit of primary rhinoplasty is the possible reduction in the stigma and psychological trauma experienced during this vulnerable phase in the child's life. It also facilitates minor corrections of the nose after adolescence20. Further, Huffman and Lierle21 demonstrated that normal growth and function of the nose usually occur when the tissues are correctly positioned. Moreover, when McComb8,15, Salyer16, Berkeley6, and Boo-Chai19 performed primary rhinoplasty on their patients and followed them until adolescence, they observed no interference with the nasal development.
Primary rhinoplasty can be performed through external incisions in the columella, intercartilaginous or marginal incisions, or incisions in the lips and nostril, with or without preoperative molding methods20. Regardless of the technique, cartilage transection and complete skin and mucosal detachment must be avoided, so that there is no harm to vascularization and, consequently, no stunted development, because the cartilages are very delicate and fragile during childhood.
In our group of patients, we found that primary rhinoplasty did not correct all deformities; we observed a harmonious nose only in few patients, mainly because a nose with symmetric measurements is not necessarily pretty. However, we corrected the most severe alterations and obtained satisfactory results. Although 6 months of postoperative follow-up is insufficient for definitive assessment, the goal is to reduce the deformities without compromising growth, so that the development occurs closer to and follows the normal side, minimizing future defects.
The complications observed in this study were related to cheiloplasty and are compatible with those cited in the literature15- 21. Because of the heterogeneity of the studied sample and variations in the nasal deformities, it would be very difficult to compare the results with a control group of patients who did not undergo rhinoplasty. Therefore, we conducted this prospective clinical study comparing the cleft side with the normal side of each patient. The simplified numeric analysis enabled assessment of the results from the postoperative photographs. We expect to follow these patients through adolescence to assess their nasal growth and determine the percentage of surgeries required for small nasal corrections.
CONCLUSION
Rhinoplasty performed concurrently with cheiloplasty ensures good early nasal symmetry in children with unilateral cleft lip or palate.
REFERENCES
1. Stenström SJ, Oberg TR. The nasal deformity in unilateral cleft lip. Some notes on its anatomic bases and secondary operative treatment. Plast Reconstr Surg Transplant Bull. 1961;28:295-305.
2. Salyer KE, Genecov ER, Genecov DG. Unilateral cleft lip-nose repair: a 33-year experience. J Craniofac Surg. 2003;14(4):549-58.
3. Blair VP. Nasal deformities associated with congenital cleft of lip. JAMA. 1925;84:185.
4. Brown JB, McDowell F. Secondary repair of cleft lips and their nasal deformities. Ann Surg. 1941;114(1):101-17.
5. Steffensen WH. A method for repair of the unilateral cleft lip. Plast Reconstr Surg. 1949;4(2):144-52.
6. Berkeley WT. Correction of the unilateral cleft lip nasal deformity. In: Grabb WC, Rosenstein SW, Bzoch KR, eds. Cleft lip and palate: surgical, dental and speech aspects. 1ª ed. Boston: Little, Brown and Company;1971. p.227-44.
7. Anastassov GE, Joos U, Zöllner B. Evaluation of the results of delayed rhinoplasty in cleft lip and palate patients. Functional and aesthetic implications and factors that affect successful nasal repair. Br J Oral Maxillofac Surg. 1998;36(6):416-24.
8. McComb H. Primary correction of unilateral cleft lip nasal deformity: a 10-year review. Plast Reconstr Surg. 1985;75(6):791-9.
9. McComb H. Treatment of the unilateral cleft lip nose. Plast Reconstr Surg. 1975;55(5):596-601.
10. Millard DR Jr. Earlier correction of the unilateral cleft lip nose. Plast Reconstr Surg. 1982;70(1):64-73.
11. Millard DR Jr., Morovic CG. Primary unilateral cleft nose correction: a 10-year follow-up. Plast Reconstr Surg. 1998;102(5)1331-8.
12. Millard DR Jr. Cleft craft: the evolution of its surgery. Boston:Little, Brown;1976.
13. Sundine MJ, Phillips JH. Treatment of the unilateral cleft lip nasal deformity. J Craniofac Surg. 2004;15(1):69-77.
14. Ortiz-Monasterio F, Olmedo A. Corrective rhinoplasty before puberty: a long-term follow-up. Plast Reconstr Surg. 1981;68(3):381-91.
15. McComb H. Primary repair of the bilateral cleft lip nose: a 10-year review. Plast Reconstr Surg. 1986;77(5):701-16.
16. Salyer KE. Primary correction of the unilateral cleft lip nose: a 15-year experience. Plast Reconstr Surg. 1986;77(4):558-68.
17. Fonseca JLS. Tratamento primário da deformidade nasal do fissurado. In: Mélega JM, ed. Cirurgia plástica fundamentos e arte:cirurgia reparadora de cabeça e pescoço. São Paulo:Medsi;2002. p.166-77.
18. Gomes PRM, Ávila E, Mélega JM. Nariz de fissurado. In: Mélega JM, ed. Cirurgia plástica fundamentos e arte:cirurgia reparadora de cabeça e pescoço. São Paulo:Medsi;2002. p. 197-212.
19. Boo-Chai K. Primary repair of the unilateral cleft lip nose in the Oriental: a 20-year follow-up. Plast Reconstr Surg. 1987;80(2):185-94.
20. Cutting CB, Kamdar MR. Primary bilateral cleft nasal repair. Plast Reconstr Surg. 2008;122(3):918-9.
21. Huffman WC, Lierle DM. Studies on the pathologic anatomy of the unilateral harelip nose. Plast Reconstr Surg. 1949;4(3):225-34.
1. Member of the Brazilian Society of Plastic Surgery, Physician Assistant at Instituto de Cirurgia Plástica Santa Cruz, São Paulo, SP, Brazil.
2. Resident Physician at Instituto de Cirurgia Plástica Santa Cruz, São Paulo, SP, Brazil.
3. Member of the Brazilian Society of Plastic Surgery, Director of the Instituto de Cirurgia Plástica Santa Cruz, São Paulo, SP, Brazil.
Corresponding author:
Rafael Ferreira Pereira da Silva
Av. Doutor Gentil de Moura, 856, apto 13 - Ipiranga
São Paulo, SP, Brazil - CEP 04278-000
E-mail: rafafps04@yahoo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: June 7, 2010
Accepted: March 15, 2011
Work performed at Instituto de Cirurgia Plástica Santa Cruz (Santa Cruz Institute of Plastic Surgery), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter