

Original Article - Year 2011 - Volume 26 -
Ear reconstruction after traumatic injuries
Reconstruções auriculares após lesões traumáticas
ABSTRACT
Background: Congenital or traumatic ear deformities are difficult and complex issues in plastic surgery due to the increasing number of cases and high degree of difficulty involved in surgeries to restore facial harmony. The authors assessed the techniques used in ear reconstruction, their complications, and the degree of esthetic and functional satisfaction. Methods: A retrospective cross-sectional study was performed, including cases of post-traumatic ear reconstruction in which costal cartilage graft was employed; the study took place at Hospital Geral de Goiânia Dr. Alberto Rassi and a private clinic from February 2005 to March 2010. Patient satisfaction with respect to esthetic and functional aspects was recorded during postoperative visits. Results: Thirty-four cases were analyzed including 14 (41.1%) women and 20 (58.9%) men (range, 13-56 years). The average time for reconstruction after trauma was 6-8 months, and the average interval between surgeries was 6 months. Five patients had complications; only 1 required re-intervention due to posterior atrial contraction. Of all patients, 30 reported being satisfied with both the esthetic and functional results; 4 were dissatisfied, and 1 of them underwent subsequent retouching. Conclusions: Ear reconstruction after trauma is a complex issue in plastic surgery; however, with the standardization and systematization of techniques and a well-established learning curve, the results are very satisfactory; facial harmony can be restored with low complication rates.
Keywords: Ear/surgery. Ear, external/surgery. Cartilage/transplantation. Plastic surgery/methods.
RESUMO
Introdução: As deformidades auriculares congênitas ou traumáticas representam um tema de expressividade e complexidade em cirurgia plástica, pelo aumento de casos e pelo alto grau de dificuldade observado nos procedimentos de reparação, necessários para a restauração da harmonia facial do indivíduo. Os autores avaliam a técnica utilizada nas reconstruções auriculares e suas complicações, bem como o grau de satisfação estética e funcional. Método: Foi realizado um estudo retrospectivo, transversal, analisando os casos de reconstrução de orelha pós-trauma, operados no Hospital Geral de Goiânia Dr. Alberto Rassi e em clínica particular, de fevereiro de 2005 a março de 2010, em que foi empregado enxerto de cartilagem costal. O grau de satisfação dos pacientes foi aferido nas consultas de pós-operatório com relação aos aspectos estéticos e funcionais. Resultados: Foram analisados 34 casos, sendo 14 (41,1%) mulheres e 20 (58,9%) homens, com faixa etária entre 13 e 56 anos. O tempo médio para a reconstrução após o trauma foi de cerca de seis meses a oito meses e de um ato cirúrgico para outro, de seis meses. Cinco pacientes apresentaram complicações, e apenas um deles necessitou reintervenção em decorrência de retração auricular posterior. Do total de pacientes avaliados, 30 se definiram como satisfeitos com o resultado tanto estético como funcional e os outros 4, como insatisfeitos, sendo um deles submetido a retoque posterior. Conclusões: A reconstrução auricular após trauma é um tema complexo da cirurgia plástica, mas com a padronização e a sistematização de técnicas e uma curva de aprendizagem bem executada os resultados são muito satisfatórios, devolvendo harmonia facial ao indivíduo, com baixa taxa de complicações.
Palavras-chave: Orelha/cirurgia. Orelha externa/cirurgia. Cartilagem/transplante. Cirurgia plástica/métodos.
Ear deformities can be congenital or develop after traumatic events such as burns, accidents, bites, or accidental amputation by sharp elements1.
In the case of post-traumatic ear injuries, the first action taken must be to ensure that the patient is in good health, by minimizing damage and the possibility of complications in the deformed area. The reuse of damaged cartilage is controversial; the amputated tissue is usually disposed of, and the reconstruction is carried out with costal cartilage or cartilage from the contralateral ear, depending on the extent of the injury and after the recovery of the patient's clinical condition and healing of the wound (6 months after the accident on average).
Ear reconstruction is one of the biggest challenges in plastic surgery. Works by authors such as Converse2, Tanzer3, Avelar4, Brent5, and Nagata6 highlight the complexity of reconstructive surgeries and how they are essential for the esthetic and functional balance of an individual.
This study assessed patients who underwent ear reconstruction after trauma to determine the employed technique, complications, and the degree of esthetic and functional satisfaction.
METHODS
Patients who underwent ear reconstruction after trauma involving the loss of ear cartilage without the possibility of using the contralateral ear to remove the graft performed at Hospital Geral de Goiânia Dr. Alberto Rassi and a private clinic from February 2005 to March 2010 were analyzed. Costal cartilage was preferably used. All cases of traumatic injuries operated on in the aforementioned interval were included in the analysis without exclusion criteria. An additional 16 patients who underwent ear reconstruction as a result of congenital malformations were not included in the case selection of this study and will be included in another report due to some peculiarities.
The degree of patient satisfaction with respect to esthetic and functional aspects was measured during postoperative visits.
RESULTS
A total of 34 patients were analyzed: 14 (41.1%) women and 20 (58.9%) men with a mean age of 33.2 years (range, 13-56 years) (Figures 1 to 3). One patient underwent simultaneous reconstruction of both ears using only costal arc cartilage (Figures 4 to 9).

Figure 1 - Pre- and postoperative periods of reconstruction of the upper pole of the right ear after traumatic injury.

Figure 2 - Pre- and postoperative periods of reconstruction of the left ear after traumatic injury due to burns.

Figure 3 - Final result after release of the upper pole and use of BTE models for 6 months.

Figure 4 - Preoperative period of a patient with traumatic loss of the left ear.

Figure 5 - Preoperative period of a patient with traumatic loss of the rigth ear.

Figure 6 - Split costal cartilage for reconstruction of both ears.
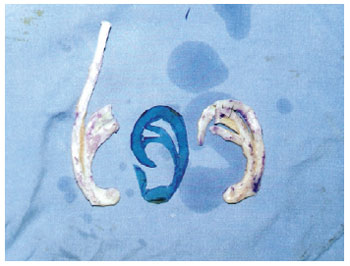
Figure 7 - Split and shaped costal cartilage for simultaneous reconstruction of both ears.

Figure 8 - Postoperative period after reconstruction of the left ear.
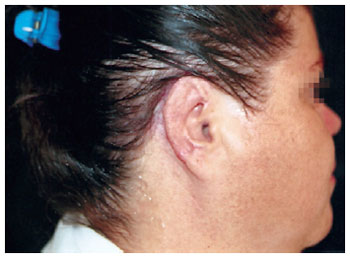
Figure 9 - Postoperative period after reconstruction of the right ear.
The average time for reconstruction after trauma was 6-8 months, and the average time interval between surgeries was 6 months.
According to the standard technique, the form of the contralateral ear was replicated using reversed radiography film; the ear cartilage was reconstructed using cartilage removed from the eighth or ninth ipsilateral costal arc (Figures 10 to 12). Both donor and recipient areas of cartilage were subjected to vacuum drainage. During the second surgery, a total skin graft removed from the inguinal region was placed, and a Behind-the-ear hearing aid (BTE) model (developed by JCS) was used for 6 months when required to avoid scar retraction in cases of reconstructions after major cartilage loss. BTE models are made of 12-mm Plastazote sponge with Velcro (Figures 13 and 14).

Figure 10 - Intraoperative period: removal of costal cartilage and shape of radiography film marking the size of the graft required for reconstruction.

Figure 11 - Intraoperative period: shaped cartilage attached to the receptor bed.

Figure 12 - Immediate postoperative period with retroauricular flap covering the graft.
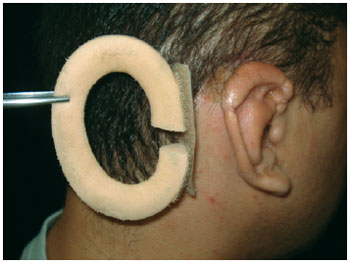
Figure 13 - BTE models used by patients who underwent reconstruction of the upper pole of the right ear.

Figure 14 - Patient using BTE models.
Complications related to surgery included 1 (0.3%) case of hematoma, 1 (0.3%) case of large absorption of the cartilaginous graft, 1 (0.3%) case of infection with exposure of the cartilage (treated with dressings and antibiotics), and 2 (0.6%) cases of scar retraction in the posterior ear after raising the graft -1 of which required surgery, which led to the development of BTE models.
In postoperative visits, 30 patients reported being satisfied with both the esthetic and functional results; 4 were dissatisfied, and 1 of them underwent retouching at a later stage.
DISCUSSION
The demand for reconstructive plastic surgery of the ear has increased over the years due to a higher incidence of traumatic injuries as a result of traffic accidents and interpersonal violence.
Ear reconstructions are very difficult and have a steep learning curve. From the beginning of reconstruction efforts to the development of current techniques, which began to be standardized by Tanzer in 19593, the results have been highly variable due to several factors - the most significant being the surgeon's experience. Another important factor is the patient's age, which influences the quality of costal cartilage; patients younger than 13 years have very little cartilage, whereas patients over 50 years have a higher degree of calcification and postoperative cartilage absorption, which makes it difficult to model the graft due to rigidity.
The incidence of ear reconstructions is higher in young men, mainly because of greater exposure to dangerous physical work, traffic accidents, and interpersonal violence.
Patients included in this study underwent reconstructions using costal cartilage, ensuring more predictable results and less scar retraction.
The period between the first and the second surgeries should be 6 months on average. BTE models are very helpful for avoiding scar retraction after the new ear is formed.
CONCLUSION
Ear reconstruction after trauma is a complex issue in plastic surgery; however, with the standardization and systematization of techniques and a well-established learning curve, the results are very satisfactory, and facial harmony can be restored with low complication rates.
REFERENCES
1. Carreirão S, Cardim V, Goldenberg D. Cirurgia plástica. São Paulo: Atheneu; 2005.
2. Converse JM. Reconstruction of the auricle. Plast Reconstr Surg. 1958;22(2):150-63.
3. Tanzer RC. Total reconstruction of the auricle. The evolution of a plan of treatment. Plast Reconstr Surg. 1971;47(6):523-33.
4. Avelar JM. Reconstrução total do pavilhão auricular num único tempo cirúrgico. (Total reconstruction of the ear pavilion in a single surgical moment) Rev Bras Cir. 1977;67:139-46.
5. Brent B. Reconstruction of traumatic ear deformities. Clin Plast Surg. 1978;5(3):437-45.
6. Nagata S. A new method of total reconstruction of the auricle for microtia. Plast Reconstr Surg. 1993;92(2):187-201.
1. Full member of the Brazilian Society of Plastic Surgery (SBCP), former president of the Regional SBCP - Goiás, former member of the Specialist Commission of SBCP, Head of the Accredited Service of the Brazilian Society of Plastic Surgery, Hospital Geral de Goiânia Dr. Alberto Rassi, Goiânia, GO, Brazil.
2. Resident physician at the Plastic Surgery Service of Hospital Geral de Goiânia Dr. Alberto Rassi, Goiânia, GO, Brazil.
Correspondence to:
José Carlos da Silva
Rua 15, 1.370 - Setor Marista
Goiânia, GO, Brazil - CEP 74150-020
E-mail: jcs.cirurgiaplastica@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: November 9, 2010
Accepted: February 5, 2011
Study conducted at Hospital Geral de Goiânia Dr. Alberto Rassi, Goiânia, GO, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter