

Case Report - Year 2013 - Volume 28 -
Rhytidoplasty in an 11-year-old patient as adjuvant treatment for post inflammatory elastolysis and cutis laxa - challenges in the treatment
Ritidoplastia em paciente de 11 anos como tratamento auxiliar da elastólise pós-inflamatória (cutis laxa) - desafios no tratamento
ABSTRACT
Cutis laxa is a rare morbidity, is caracterized as a connective tissue disorder manifested primarily by sagging cut and may affect other organs. The authors report a case of cutis laxa in a patient of 11 years old with the development of a senile fascia with pronounced ritidose perioral, periocular and nasolabial sulcus. Rhytidectomy was performed as an auxiliary treatment. The patient showed a good evolution of the postoperative scars with good quality and remarkable improvement in sagging of the midface and later recurrence of the same part in the follow-up evaluation two years. Patient and family were very pleased with the outcome. The surgical team, however, realized the limitation of the procedure and the need for additional treatment with auxiliaries and the like as peeling.
Keywords: Cutis laxa. Rhytidoplasty. Face.
RESUMO
Cútis laxa é uma morbidade rara, caracterizada por ser uma desordem do tecido conjuntivo que se manifesta principalmente por flacidez cutânea, podendo acometer variavelmente outros órgãos. Os autores relatam um caso de cútis laxa em paciente de 11 anos que desenvolveu face senil com pronunciada ritidose perioral e periocular, bem como acentuação dos sulcos nasogenianos. Foi realizada ritidoplastia como tratamento cirúrgico. Apresentou boa evolução pós-operatória, com cicatrizes de boa qualidade e melhora notável na flacidez do terço médio da face e, posteriormente, recorrência parcial da mesma no acompanhamento tardio de dois anos. Paciente e familiares ficaram muito satisfeitos com o resultado. A equipe cirúrgica, entretanto, percebeu limitação do resultado cirúrgico e necessidade de complementação com tratamentos auxiliares como peelings e similares.
Palavras-chave: Cutis laxa. Ritidoplastia. Face.
Cutis laxa is a rare disease characterized by hypoelasticity of the skin due to defective elastin fibers1. It was first described in 1966 by Marshall et al. who described a case of dermatosis of unknown etiology characterized by erythematous papular lesions with centrifugal progression, raised edges, and collarette desquamation. These lesions develop, leading to intense disfiguration and a prematurely aged appearance. There are congenital forms (i.e., autosomal dominant, autosomal recessive, and X-linked recessive) and acquired forms, which differ both clinically and genetically1,4. Symptoms of the congenital form are visible from birth or appear during the first few months of life. This form is transmitted as an autosomal recessive characteristic; it is serious and has high morbidity and mortality rates. The disease has a systemic and syndromic presentation characterized by delayed growth, skeletal dysplasia, pulmonary emphysema, cardiovascular implications, and multiple hernias1,4,5. Symptoms generally appear before 4 years of age, with a variable duration of the active inflammatory phase, reaching the atrophic phase of stabilization in infancy2. This is linked with mutations in the genes for fibulin 4 and 5 as well as a vesicular ATPase subunit5,6.
Meanwhile, the autosomal dominant form has relatively few symptoms, which are limited to the skin (primarily the face), and is linked to mutations in the elastin gene2. The X-linked recessive form is associated with decreased activity of lysyl oxidase, an enzyme responsible for the formation of aldehyde groups, which are essential for collagen cross-linkage. The X-linked form is characterized by diverticula and dysfunction of the bladder and occipital horn growth as well as relatively normal intelligence. Affected individuals typically have a prematurely aged face, hooked nose with everted nostrils, long upper lip, everted lower eyelids, and drooping cheeks. Symptoms of the acquired form, which is often preceded by an undefined fever, usually appear after puberty but sometimes do not appear until mid-life or later2,4. Cutis laxa associated with fever and neutrophilic dermatosis is called Marshall syndrome5.
Histologically, cutis laxa is characterized by a reduced number of elastin fibers in the dermis, with fragmentation and alterations to their normal arrangement4.
Many treatments for cutis laxa have been reported, including corticotherapy, colchicine, dapsone, doxycycline, non-hormonal anti-inflammatory drugs, and cyclosporines as well as surgical procedures such as rhytidoplasty, blepharoplasty, and canthopexy1 ,2,5
CASE OVERVIEW
The present study concerns an 11-year-old mulatto female patient with post-inflammatory elastolysis and cutis laxa. She has been monitored since 2 years of age at the Department of Dermatology, Faculty of Medicine, Botucatu - UNESP. Clinical symptoms appeared at 2 years of age, including disseminated papules and vesicles that progress to dry wrinkly squamous plaques of various sizes with no systemic changes. Such lesions in the facial region give an aged appearance (Fig. 1) with pronounced perioral and periocular rhytidosis as well as accentuated nasolabial folds. She began retinoid-based treatment under the direction of dermatologists at 10 years of age with limited results. At 11 years of age, she was referred to a plastic surgeon and underwent rhytidoplasty under general anesthesia. The procedure began with a temporal incision all the way to the pre-auricular region, bypassing the ear lobe, through the retroauricular region to the temporo-occiptal region and then partially intracapillary. The skin flap was dissected above the superficial muscular aponeurotic system and platysma. Two point tractions were applied to the facial flat in the superior oblique-posterior direction: one in the temporal region, and the other in the retroauricular region. Plications on the superficial muscular aponeurotic system and platysma were performed, because these structures were not flaccid. Excess skin was resected, a continuous aspiration drain was inserted, and layer synthesis was performed (Fig. 2).

Figure 1 - Preoperative images .
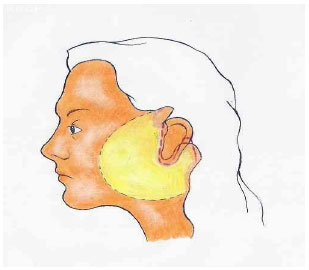
Figure 2 - Schematic diagram showing incision (dotted line), relocated area (yellow), and excess skin.
There were no complications during the intraoperative or immediate postoperative period. At the 6-month postoperative assessment, the scars were thin and light, and noticeable improvement in the sagging of the middle third of the face was observed (Fig. 3).

Figure 3 - 6-month postoperative images.
During 2 years of postoperative follow-up, the scars maintained their quality as expected (Fig. 4). However, there was partial recurrence of sagging skin (Fig. 5). Regardless, the patient and her family members were very satisfied with the results. However, the surgical team found that the surgical outcome was limited; they recommend patients undergo additional more intensive treatments such as peeling.
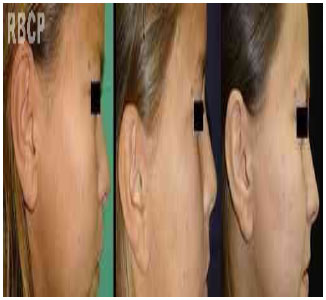
Figure 4 - Preoperative, and 6- and 24-month postoperative images showing scar evolution .

Figura 5 - 24-month postoperative images .
DISCUSSION
Cutis laxa is a rare disease that results in the degradation and agglutination of elastin fibers in the dermis. Post-inflammatory elastolysis and cutis laxa primarily occur in tropical countries (9:1 cases) and mainly affects African Americans (8:1 cases) and females (4:1 cases)2. It forms part of the heterogeneous group of connective tissue disorders characterized by sagging skin and affecting several other organs. Thus, the case described herein is consistent with other cases in the literature with regard to the group most affected by this disease.
Some authors mention performing plication of the superficial musculoaponeurotic system, claiming this produces longer-lasting results when loose, and emphasize the importance of surgically correcting drooping skin1,8. In the present case, plication of the superficial musculoaponeneurotic system and platysma was not performed because of the patient's young age and the fact that they did not sag; thus, only rhytidoplasty with skin resection was performed. Treatment should focus on treating sagging skin, which was the primary symptom in the present case. It should be noted that current surgical procedures such as rhytidoplasty, blepharoplasty, and canthopexy aim to improve the symptoms of cutis laxa without contributing to the involution or cure of the underlying disease; despite these procedures, the disease continues to progress naturally, requiring future treatments. Furthermore, it is important to emphasize that these surgical procedures have limited results; nevertheless, they improve the patient's quality of life including major psychosocial impacts by mitigating the natural evolution of the disease1. Therefore, we encourage the use of additional cosmetic procedures such as peeling and laser treatments to complement surgical outcomes.
CONCLUSION
According to the results of the case reported herein, performing rhytidoplasty in patients with cutis laxa is encouraged, because it significantly improves the stigma of a prematurely aged face, thus creating significant physical, social, and psychological benefits by mitigating the natural evolution of the disease. We also highlight the importance of using additional cosmetic procedures such as peeling and laser treatments to enhance surgical results.
REFERENCES
1. Banks ND, Redett RJ, Mofid MZ, Manson PN. Cutis laxa: clinical experience and outcomes. Plast Reconstr Surg. 2003;111(7):2434-42.
2. Aguilar CR, Gontijo B, Vale ECS. Elastólise pós-inflamatória e cutis laxa (doença de James Marshall): estudo de casos. An Bras Dermatol. 2007;82(4):317-26.
3. Carvalho MLR, Vale ES, Figueiredo VF. Elastólise pós-inflamatória e cútis laxa. An Bras Dermatol. 1991;66(2):83-5.
4. Siqueira MFC, Ministério PA, Valadares ER, Purisch S, Bambirra EA, Pardini VC. Cutis laxa associada à insuficiência cardíaca congestiva. J Pediatr (Rio J). 1999;75(1):63-8.
5. Nahas FX, Sterman S, Gemperli R, Ferreira MC. The role of plastic surgery in congenital cutis laxa: a 10-year follow-up. Plast Reconstr Surg. 1999;104(4):1174-8.
6. Morava E, Lefeber DJ, Urban Z, de Meirleir L, Meinecke P, Gillessen Kaesbach G, et al. Defining the phenotype in an autosomal recessive cutis laxa syndrome with a combined congenital defect of glycosylation. Eur J Hum Genet. 2008;16(1):28-35.
7. Haider M, Alfadley A, Kadry R, Almutawa A. Acquired cutis laxa type II (Marshall syndrome) in an 18-month-old child: a case report. Pediatr Dermatol. 2010;27(1):89-91.
8. Steiner CE, Cintra ML Marques-de-Faria AP. Cutis laxa with growth and developmental delay, wrinkly skin syndrome and gerodermia osteodysplastica: a report of two unrelated patients and a literature review. Genet Mol Biol. 2005;28(2):181-90
1. Second-year resident. Department of Plastic Surgery, Faculty of Medicine of Botucatu - UNESP
2. Lecturer. Professor of Plastic Surgery, Faculty of Medicine of Botucatu - UNESP
3. Associate Member of SBCP. Plastic Surgeon at Hospital dos Fornecedores de Cana of Piracicaba - SP
4. Associate Member of SBCP. Plastic Surgeon at Hospital dos Fornecedores de Cana of Piracicaba - SP
Wellerson Marcos Mattioli
Rua Petúnia, 101/28, Jardim Bom Pastor
Botucatu - SP CEP: 18603-502
Article recceived: 25/03/2011
Article acceited: 24/05/2011
Study carried out in Clinical Hospital of Faculty of Medicine of Botucatu - UNESP, Botucatu, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter