ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Barraquer-Simons syndrome: literature review and case report
Síndrome de Barraquer-Simons: revisão da literatura e relato de caso
Case Reports -
Year2016 -
Volume31 -
Issue
2
André Luiz de Araujo França1; Luís Alberto de Souza Leite1,2; Jeanine Maria Tejo Caminha1,2; Carlos Lacerda de Andrade Almeida1,2; Ênio Gomes de Araújo1; Ernani Coelho Alencar1; Rafael Neves de Souza1; Jonathan Augusto Vidal de Oliveira1; Pedro Flávio de Oliveira Batista1
http://www.dx.doi.org/10.5935/2177-1235.2016RBCP0046
ABSTRACT
Barraquer-Simons syndrome is a type of lipodystrophy characterized by progressive atrophy of the subcutaneous tissue limited to the upper body. Its involvement is usually symmetrical with craniocaudal evolution, reaching down to the thighs. This syndrome is also known as cephalo-thoracic lipodystrophy or progressive partial lipodystrophy. It is a rare disease of unknown origin that usually manifests at the beginning of the second decade of life and has predominance among women. We report a case and literature review of this rare disease, its therapeutic management, and a comparison with other treatment modalities currently available. During one year and three months follow-up, four sessions of facial fat grafting were performed following the principles of structural fat grafting. The use of this therapeutic modality, improved significantly facial contour, and almost complete disappearance of depressions and irregularities, and preservation were achieved during follow-up time. A number of treatments have been described as effective for lipodystrophy, such as: use of alloplastic materials, autologous grafts, local and microsurgical flaps. Each treatment has advantages and disadvantages. Decision depends on the surgeon's experience, availability of resources, specific materials in each center.
Keywords:
Lipodistrophy; Rare diseases; Surgical flaps; Face.
RESUMO
A síndrome de Barraquer-Simons é uma lipodistrofia caracterizada por progressiva atrofia do tecido celular subcutâneo limitada à parte superior do corpo. Seu acometimento costuma ser simétrico e com evolução craniocaudal, podendo atingir até as coxas. Também é conhecida como lipodistrofia céfalo-torácica ou lipodistrofia parcial progressiva. É uma doença rara, de origem obscura, que geralmente se manifesta no começo da segunda década de vida e tem predominância no sexo feminino. O presente trabalho objetiva trazer uma revisão da literatura e relatar um caso desta rara patologia e sua condução terapêutica, comparando-a a outras modalidades de tratamento disponíveis atualmente. Durante o período de um ano e três meses de seguimento, foram realizadas quatro sessões de enxertia de gordura seguindo os princípios da lipoenxertia estruturada. Por meio desta modalidade terapêutica, foi possível obter uma melhora importante do contorno facial com desaparecimento quase completo das depressões e irregularidades características da doença e preservação do resultado durante o tempo de acompanhamento. Diversos tipos de tratamentos foram descritos como efetivos para as lipodistrofias: uso de materiais aloplásticos, enxertos autólogos, retalhos locais e microcirúrgicos. Cada um deles possui suas vantagem e desvantagens e a escolha dependerá da experiência do cirurgião e da disponibilidade de recursos e materiais específicos em cada centro. A lipoenxertia se mostrou uma forma de tratamento eficaz, simples, segura e de baixo custo para tratamento da síndrome de Barraquer-Simons.
Palavras-chave:
Lipodistrofia; Doenças raras; Retalhos cirúrgicos; Face.
INTRODUCTION
Primary lipodystrophies constitute a heterogeneous group of rare diseases with prevalence of less than 1:100,000 per inhabitants1. They can be classified based on extension of manifestations as partial, limited to a body part, or generalized. In relation to symptoms onset time, it may be hereditary or acquired. The congenital partial lipodystrophy is known as Dunnigan type, and the congenital generalized lipodystrophy as Berardinelli type2.
The rare Barraquer-Simons syndrome was first described by Barraquer in 1906, and then by Simons in 19111-3. This is a partial and acquired lipodystrophy, which usually appears at the beginning of the second decade of life and has predominance among women. In general there is no previous family history and the origin of the disease is unclear. This disease is often associated with viral infections, and recently it has been related to a mutation in the gene encoding blades nuclear B2 subtype (LMNB2), which probably acts as a predisposing factor but not a determinant of its emergence4. Many genetic mutations have been identified as causes of inherited lipodystrophy, however, in acquired lipodystrophy such as Barraquer-Simons this relationship is not well established 4. Perhaps, there is the need to associate genetic susceptibility to other triggering factors2-4.
The syndrome is characterized by progressive atrophy of subcutaneous limited to upper body, and its involvement is usually symmetrical with craniocaudal progress, reaching down to the thighs5-7. It is also known as caphalo-thoracic lipodystrophy or progressive partial lipodystrophy.
Patients usually complaint about changes in facial contour, but in 20% of cases it may be associated to systemic manifestations such as autoimmune diseases (glomerulonephritis, lupus, dermatomyositis, hypothyroidism and pernicious anemia), neurologic or metabolic disorders such as dyslipidemia, resistance insulin, type 2 diabetes and hypocomplementemia2,6.
OBJECTIVES
We report a case and literature review of Barraquer-Simons syndrome, its management with serial fat grafting, and an approach of other therapeutic options.
MATERIALS AND METHODS
Case report
A 46-year-old woman (IM), a school teacher, born and raised in Águas Belas-PE, was admitted to the plastic surgery service at Hospital Agamemnon Magalhães for evaluation and treatment in April/2012.
The patient complained about progressive atrophy of adipose tissue that began 20 years ago on the cheek region with left to right progression, and also to other parts of the face (bilateral temporal region and bilateral orbital region). She reported posteriorly fat atrophy extending to distal end of the left arm.
The patient denied alcohol consumption, use of tobacco products or drugs. She did not have other comorbidities or similar cases of the disease in her family. No other complaints were reported by patient.
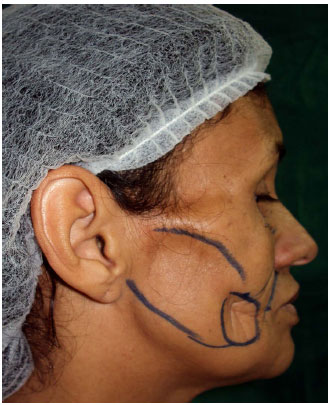
Upon examination, the patient was emaciated, without impairment of general condition or cognitive. She had areas of lipoatrophy on bilateral cheek region, more prominent at right side, end up forming a deep groove on site. The patient also presented subcutaneous atrophy on bilateral temporal and orbital regions (Figures 1, 2 and 3).
 Figure 1.
Figure 1. Preoperative marking of the first fat grafting. A subcutaneous atrophy on temporal region is observed, mainly on cheeks, creating a deep sulcus on the site.
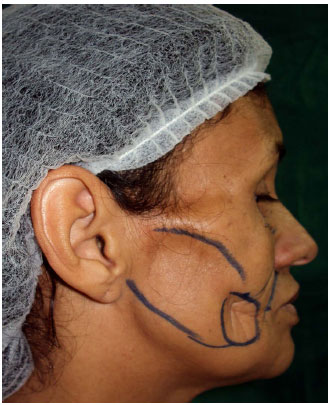 Figure 2.
Figure 2. Preoperative marking of the first fat grafting.
 Figure 3.
Figure 3. Preoperative marking of the first fat grafting.
The patient underwent four sessions of facial fat grafting following the principles of Coleman8 structural fat grafting with a change in processing fat by decantation instead of centrifugation.
Initially the asepsis, antisepsis with chlorhexidine solution and affix sterile field were carried out. After a small area of abdomen or thigh was infiltrated with lidocaine 0.4%, bupivacaine 0.0005% and epinephrine 1:200,000, but always respecting the maximum doses of lidocaine (7 mg/kg) and bupivacaine (2 mg/kg).
We used a thin cannula (2 mm) of two holes attached to a luer lock 10ml syringe. Liposuction was proceeded in a small area of the abdomen under anesthesia with low negative pressure (2 ml syringe). Afterward, collected material was washed with saline solution and decanted for about 15 minutes. After decanting, both the lower portion of the decanted (blood, anesthetic solution, serum) and the oily supernatant were discarded, we used only the central portion.
After this step, infiltration of anesthetics was proceeded in some areas of the face. In each session, approximately 35 ml of fat was grafted, which was divided in different parts of the face. A micro cannula measuring 1.2 mm attached to a 1ml syringe was used for grafting. Small amounts of fat were injected in each pass of the cannula, to guarantee creation of several tunnels and maximum contact with the host tissue.
The dressing was done by Micropore® adhesive tape and the donor siste was maintained under pressure with compression bandaging for a few days.
The patients was kept under surveillance for approximately 3 hours. Because no changes or symptoms at donor/recipient site were seen, she was discharged.
RESULTS
The therapeutic modality used improved significantly facial contour with almost complete disappearance of depressions and irregularities common in the disease, and preservation of the outcome during monitoring time.
Improvement on the facial contour mainly on cheek region was seen compared with the preoperative period in which a deep depression was observed. Filling of orbital regions has brought more harmony to the face, removing the appearance of sunken eye. Temporal filling along with cheek attenuated the apparent prominence of the zygomatic arch observed before the surgery (Figures 1 to 7).
 Figure 4.
Figure 4. Result after two fat grafting session. Improvement of contouring mainly on cheeks. Persist atrophy on temporal and periorbital region.
 Figure 5.
Figure 5. Result after two fat grafting session. Improvement of contouring mainly on cheeks. Persist atrophy on temporal and periorbital region.
 Figure 6.
Figure 6. Result after four fat grafting session. Disappearing of "cadaveric" appearance with improvement of contouring and harmony of the face.
 Figure 7.
Figure 7. Result after four fat grafting session. Disappearing of "cadaveric" appearance with improvement of contouring and harmony of the face.
Face lipodystrophy is a problem that can affect patients' social life. This disease changes give the idea of unhealthy appearance and may cause social stigma associated with HIV. To reestablish the harmony of facial contour is fundamental to help patients regain self-esteem and be motivated.
DISCUSSION
A number of treatments have been described to restore face contour after lipodystrophy. Alloplastic materials can be used such as silicone implants, polymethylmethacrylate filling, or autologous tissues such as fat grafting or flaps (pedicled or microsurgical)9.
Alloplastic materials have advantages of be simple and practical for application, but may be accompanied by local reactions such as inflammation and granuloma10 and they usually are costly, which constitutes a limiting factor for wide use in most Brazilian centers.
Fat grafting is an adequate treatment for the facial abnormalities seen in this syndrome11. This technique is effective, simple, safe and with low cost12.
The principles of structural fat grafting8 were adopted to increase the use of each procedure. For this reason, the use of sm all cannulas favor the aspiration of small lobules of adipocytes, which facilitate revascularization. In addition, in an attempt to promote minimum adipocytes lesion, a low vacuum negative pressure is used. The use of decanter is a way to separate fat from the blood and from the oily supernatant, which enable only the adoption of viable tissue. The grafting of small amounts of fat with each pass of the cannula allows to create multiple tunnels with highest integration with the recipient tissue.
Because procedure is done with minimal incisions and by the use of thin cannulas, risk of complications is much lower than in any open procedure. The most common complications are those related to aesthetics aspects, as overcorrection or irregularities. Cyst formation, infection, hematoma, nerve injury and fat embolism can also be described, but fortunately, they are rare8.
During 1 year and 3 months follow-up, we carried out 4 sessions of fat grafting. In this period grafted volume was preserved after the initial loss, which was estimated at 40%. No complications were reported demonstrating the efficacy and safety of the treatment.
Fat grafting does not require special equipment other than a cannula, which is associated it to be possible done in semi-ambulatory setting, and reduces significantly the cost of the procedure. Therefore, low cost associated with the simplicity of the procedure allows the method to be widely used.
This technique disadvantage is the need of multiple sessions and the fact that some authors suggest partial reabsorption after 4 years, however, they also report that in such cases grafting can be performed again without additional risks to the patient12.
Vascularized tissues can be done using local and microsurgical flaps. Among local flaps, there are pedicled temporalis muscle flap and musculocutaneous pectoralis flap, which were replaced by free flaps that allow greater mobility and possibility of modeling in the recipient area14.
Among microsurgical or free flaps there are the groin flap and scapular flap that may cause unacceptable scars in the donor area and frequently present ptosis. There is also the transverse rectus abdominal flap, which has less chance of ptosis, but leads to higher defect in the donor area, and may evolve to hernias. The deep inferior epigastric artery, as well as the anterolateral thigh flap that provide an adequate modeling on the face, but has a little tendency to ptosis14. Generally, the incorporation of muscle tissue into flap reduces possibility of ptosis due to the greater consistency of the muscle compared to fat tissue and the firm adherence of muscle to surrounding tissues15.
CONCLUSION
Free microsurgical flaps are great alternatives to recover facial contours, with preservation of volume and symmetry in long term15. However, they cause scars on the recipient area, greater morbidity at donor site (scars, hernia ...), increased risk of complications such as flap necrosis, longer hospital stay, specialized infrastructure, longer learning curve, and higher cost.
The fat grafting seems to be effective, simple, safe and low-cost treatment for Barraquer-Simons syndrome.
Patients follow-up over 1 year and three months allowed to preserve the grafted tissue after the initial loss estimated in 40%. A longer follow-up is need for conclusions related with long term tissue preservation, however, in case of appearance of new areas of atrophy or recurrence in areas already treated, these areas can be receive new allografts in the future.
This technique simplicity, safety, and low cost also shows a short learning curve and requires few materials, therefore, enabling it to be widely used.
The choice of treatment modality depends on surgeon's experience, availability of resources and structure at each institution.
COLABORATIONS
ALAF Participated in surgeries. Contributed to the conception and design of the study, drafting the manuscript, review and approval of final version to be published.
LASL Participated in surgeries. Contributed to conception and design of the study, and critical review of the study.
JMTC Participated in surgeries. Contributed to conception and design of the study, and critical review of the study.
CLAA Participated in surgeries. Contributed to conception and design of the study, and critical review of the study.
ÊGA Participated in surgeries.
ECA Participated in surgeries.
RNS Participated in surgeries.
JAVO Participated in surgeries.
PFOB Participated in surgeries.
REFERENCES
1. Capeau J, Magré J, Lascols O, Caron M, Béréziat V, Vigouroux C. Primary lipodystrophies. Ann Endocrinol (Paris). 2007;68(1):10-20. DOI: http://dx.doi.org/10.1016/j.ando.2006.12.003
2. Hegele RA, Joy TR, Al-Attar SA, Rutt BK. Thematic review series: Adipocyte Biology. Lipodystrophies: windows on adipose biology and metabolism. J Lipid Res. 2007;48(7):1433-44. PMID: 17374881 DOI: http://dx.doi.org/10.1194/jlr.R700004-JLR200
3. Santos M, Rabelo R, Vilasboas V, Nogueira L, Talhari C, Talhari S. Você conhece esta síndrome? Síndrome de Barraquer-Simons. An Bras Dermatol. 2011;86(2):391-440. DOI: http://dx.doi.org/10.1590/S0365-05962011000200037
4. Hegele RA, Cao H, Liu DM, Costain GA, Charlton-Menys V, Rodger NW, et al. Sequencing of the reannotated LMNB2 gene reveals novel mutations in patients with acquired partial lipodystrophy. Am J Hum Genet. 2006;79(2):383-9. PMID: 16826530 DOI: http://dx.doi.org/10.1086/505885
5. Franco FF, Spencer LB, Mendes FD, Lopes RG, Braga EVB, Pinheiro AF, et al. Tratamento cirúrgico do paciente com síndrome de Barraquer-Simons: revisão bibliográfica e relato de caso. Rev Soc Bras Cir Craniomaxilofac. 2007;10(4):152-5.
6. Sampaio SAP, Rivitti EA. Dermatologia. 3a ed. Porto Alegre: Artes Médicas; 2007.
7. Azulay RD, Azulay DR. Dermatologia. 5a ed. Rio de Janeiro: Guanabara Koogan; 2008.
8. Coleman SR. Structural fat grafting. In: Bartlett SP, Robert W. Beasley RW, Aston SJ, Gurtner GC, Scott L. Spear SL, eds. Grabb and Smith's Plastic Surgery. 6th Ed. Philadelphia: Lippincott Williams & Wilkins/Wolters Kluwer; 2006. p. 480-5.
9. Spranger S, Spranger M, Tasman AJ, Reith W, Voigtländer T, Voigtländer V. Barraquer-Simons syndrome (with sensorineural deafness): a contribution to the differential diagnosis of lipodystrophy syndromes. Am J Med Genet. 1997;71(4):397-400. PMID: 9286444 DOI: http://dx.doi.org/10.1002/(SICI)1096-8628(19970905)71:4<397::AID-AJMG5>3.0.CO;2-R
10. Dornelas MT, Corrêa MPD, Netto GM, Barra FML, Alves SGS, Dornelas MC, et al. Bioplastia na lipodistrofia de pacientes com HIV/AIDS. Rev Bras Cir Plást. 2012;27(3):387-91. DOI: http://dx.doi.org/10.1590/S1983-51752012000300010
11. Mansouri Hattab N, Lahmiti S, Aimadeddine S, Fawzi S, El Bouihi M, Fikry T. Barraquer-Simons syndrome. Rev Stomatol Chir Maxillofac. 2011;112(3):172-3. PMID: 21514609 DOI: http://dx.doi.org/10.1016/j.stomax.2011.03.005
12. Cedrola JPV, Castro CC, Aboudib JH, Turini T, Castro M, Serra F. Análise do tratamento da Síndrome de Parry-Romberg por lipoenxertia estruturada no Hospital Universitário Pedro Ernesto-HUPE-UERJ. Rev Bras Cir Plást. 2011;26(sup l):1-102.
13. Ducours JL, Poizac P, Ardanza B, Modschiedler T, Caix P. Barraquer-Simons syndrome and facial lipo-filling. Apropos of a case. Rev Stomatol Chir Maxillofac. 1991;92(2):105-11.
14. Teixeira V, Badin AZD, Salles Júnior GS, Vieira JC, Bailak M, Ottoboni E, et al. Síndrome de Barraquer Simon: relato de caso e revisão de literatura. Arq Catarin Medicina. 2007;36(Supl.1):73-5.
15. Goossens S, Coessens B. Facial contour restoration in Barraquer-Simons syndrome using two free TRAM flaps: Presentation of two case reports and long-term follow-up. Microsurgery. 2002;22(5):211-8. DOI: http://dx.doi.org/10.1002/micr.22508
1. Hospital Agamenon Magalhães, Recife, PE, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital Agamenon Magalhães, Recife, PE, Brazil.
Corresponding author:
André Luiz de Araujo França
Rua Cel Anízio Rodrigues Coelho, 678, Apto: 1302 - Boa viagem
Recife, PE, Brazil Zip Code 51021-130
E-mail: andrefranca@pop.com.br
Article received: July 16, 2013.
Article accepted: November 25, 2013.
Conflicts of interest: none.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license